In Week 2, we will continue to cover the following courses:
- Professional Practice Part 1
- Dispensing
- Patient Care
In this topic, we'll continue our instruction on prescription forms. We introduced controlled drug prescription forms previously, and now we'll continue with Electronic Prescriptions.
Electronic Prescriptions
Read this page from Te Whatu Ora about signature-exempt prescriptions and answer the following questions to confirm your understanding:
Expiry dates
Prescription forms have a legal expiry date calculated from the date on which the prescription was written. Consult the Medicine Regulations 1984, section 42(3)(c) & (d) to answer the following three questions for each scenario.
Prescription forms for subsidised medications also have a funding expiry date, after which time the medication may still be dispensed, but the subsidy it usually has will no longer apply. The funding expiry date is three months from the prescription date. When you have an answer, select the label or (+) sign below to see if you are right.
This means that someone can legally have a prescription filled three months after it has been written but will pay the full cost because any subsidy that was attached to the medicine has now expired. However prescriptions for Controlled Drugs may vary depending on Class.
Verbal prescriptions
In some instances, a prescription can be given verbally, either face to face, faxed, or over the telephone under the following legislation:
- Prescriptions for non-CD medicines: Medicine Regulations 1984, Section 40A
- Prescriptions for CDs: Misuse of Drugs Regulations 1977, Regulation 34
Take a moment now to click on the links above and read the legislation regarding verbal prescriptions.
About verbal prescriptions:
- Pharmacy technicians and other staff cannot receive any verbal prescriptions. They can only be received by the pharmacist.
- For non-CD and CD verbal prescriptions, the prescriber must be personally known to the pharmacist
- For non-CD verbal prescriptions, the prescriber must issue a prescription to the pharmacist in paper or electronic form within 7 days to confirm oral communication.
- For CD verbal prescriptions in an emergency, the prescriber must issue a prescription to the pharmacist in paper or electronic form immediately that confirms the oral communication.
Limits on supply
The Medicine Regulations, Section 39A, details the quantity of non-CD medicine that can be supplied on prescriptions based on a period of time. This is called ‘limit on the period of supply’. Using your understanding of The Medicine Regulations, see if you can correctly complete the activity below.
Emergency supply
As a pharmacy technician, you may come across the following situation where a customer does not have a prescription form but requires an emergency supply of their usual medications.
What should the pharmacist do?
Scenario:
Fred, a 65-year-old man, approaches you at the dispensary counter with two empty medicine packets and says:
"Hi, I’m in town for the weekend and just realised I didn’t pack enough of my medicines to last until I get home on Monday morning. My doctor told me I should never suddenly stop taking my Atenolol, and I need the Codeine for my back pain. Can I get some of both to last me the weekend?"
Fred hands you the empty packets. You know that Atenolol is a drug used to treat high blood pressure and irregular heart rhythms, and Codeine is a class C controlled drug used to treat pain.
You notice the medicine labels have the name of Fred’s G.P., and both medicines have been dispensed within the last month.
Now, think about your answers to the following questions before selecting the label or (+) sign to see if you got it right.
The legislation that applies to this situation is the Medicine Regulations 1985, section 44(m), which states:
44. Prescriptions for prescription medicines are not required in certain cases
Prescription medicine may be sold or dispensed otherwise than under a prescription given by a practitioner, registered midwife, veterinarian, or designated prescriber if it is sold to or dispensed for—
(m) a person who has previously been supplied with the medicine on the prescription of an authorised prescriber for a particular condition and is so sold or dispensed—
(i) by a pharmacist who is satisfied that the person requires an emergency supply of the medicine for that condition; and
(ii) in an amount not exceeding the quantity reasonably required by that person for 72 hours, or a minimum pack of a special container from which it is not practicable to dispense a lesser amount; or
(n) any person by a veterinarian for the treatment of an animal under the care of the veterinarian or
(o) a person or body authorised to distribute, or a person authorised to administer, the prescription medicine in an approved immunisation programme.
Source: Medicines Regulations 1984.
You will notice that the legislation does not define what an emergency is; therefore, it is up to the pharmacist, in this case that's you, to ask the customer questions, assess and use professional judgement to decide if the situation is an emergency.
Before dispensing an emergency supply at the request of a patient, a pharmacist should check the following:
- That the request is genuine
- That there is an immediate need for the medicine
- If the clinical condition of the patient requires referral to a medical practitioner
- That a New Zealand registered prescriber has prescribed the requested medicine within the past three months to six months
- The patient is not using the emergency supply as their regular supply
- That the strength and dose of the requested medicine are appropriate
- If the patient's prescriber or regular pharmacy should be contacted to confirm that the information provided is correct
In some instances, it is not practical to supply only 72 hours' treatment. In these situations, it is OK to supply an original pack, for example, one inhaler or one month’s supply of an oral contraceptive.
The sale of an emergency supply should be recorded electronically as you would a Pharmacist Only Medicine. The record should contain the following information:
- Date of sale
- Name and address of the purchaser
- Name and quantity of medicine sold
- Name of pharmacist making the sale
The emergency supply of medicines only applies to prescription medicines and not controlled drugs. Therefore, an emergency supply of controlled drugs cannot be dispensed. Customers who run out of their supply of CD medicines will need to go back to their prescriber for a prescription. The prescriber may give that prescription in paper or electronic format.
Under the Misuse of Drugs Legislation 1977, Regulation 34, in an emergency situation, the prescriber may give a verbal prescription over the phone to the pharmacist under the following conditions:
- The prescriber must be personally known to the pharmacist.
- After the verbal prescription is given, the prescriber must immediately issue a paper or electronic prescription that confirms the verbal prescription.
- The prescription must include a statement that it is a confirmation of the verbal prescription and state what date the verbal prescription was given.
Using your learning on this topic, answer the following questions about how you should respond to Fred’s inquiry.
Brand Substitution
The legislation that applies to this situation is the Medicine Regulations 1984, Section 42(4). This regulation states that if an authorised prescriber has written a prescription using a medicine's trade name, then a pharmacist may supply an alternative brand of medicine, provided that:
- The prescriber has not marked the prescription with “No brand substitution permitted” or similar words
- The substitute brand contains the same active ingredients and no other active ingredients
- The substitute brand is the same dose form and strength as prescribed
- There is no clinical reason why the substituted brand should not be supplied
- The patient is informed of the substitution
- The pharmacist records the brand substitution on the prescription
- The pharmacist signs and dates the prescription
As a pharmacy technician, you have certain limitations in your practice. Using the knowledge you gained above about those rules, can you substitute an alternative brand medicine in the following situations?
Decide if the answer is yes or no, and then flip each of the four cards to see if you are right. (Please assume all conditions not mentioned have been met.)
Reciprocal Health Agreements
A reciprocal health agreement is a legislated agreement between the government of New Zealand and another country. The agreement states that citizens from each country are eligible to receive certain government-funded health services while they are in the other country. These health services include pharmacy services.
Read Te Whatu Ora to find out which two countries New Zealand has reciprocal health agreements with and the legislation that applies to these agreements. When you have the answer, see if you are right below.
Select the (+) or the label below to see the information summarised.
- Australian citizens visiting New Zealand on a temporary visa who need immediate and necessary treatment are covered by the reciprocal health agreement, including treatment that is immediately necessary for both new and existing conditions. The provider of the medical treatment will decide as to whether the treatment is ‘immediately necessary’.
- UK citizens temporarily visiting New Zealand who have a condition that worsens, arises after arrival, or without treatment will get worse are covered by the reciprocal health agreement. The provider of the medical treatment will make this decision.
Role of the technician
As a pharmacy technician, it is important you understand the scope of your practice. This means being clear on what care, advice, and dispensing activities you can and cannot carry out. So far in this course, we have identified that as a pharmacy technician, you cannot:
- Make brand substitutions to a prescription.
A pharmacist is the only one permitted to do this; therefore, brand substitution is outside of your scope of practice. - Take a telephone prescription.
A telephone prescription can only be taken by a pharmacist who personally knows the prescriber; therefore, taking a phone prescription is outside of your scope of practice.
Read the excerpt below from the Regulation 42 and Regulation 63 sections of the Medicine Regulations. There is a phrase that appears in both of them that defines the statute limitations on pharmacy technicians when dispensing and compounding medicines. Can you identify it?
42 Dispensing of prescription medicines
(1) Except as provided in subclause (2), no person other than an authorised prescriber, veterinarian, pharmacist, pharmacy graduate, a pharmacy technician, a student, or dispensary technician may dispense a prescription medicine.
(1A) The following persons may not dispense prescription medicines unless under the direct personal supervision of a pharmacist:
(a) dispensary technicians
(b) pharmacy graduates
(c) pharmacy technicians
(d) students
63 Restriction on, and supervision of, compounding medicine
(1) A dispensary technician must not undertake any process of compounding a medicine.
(2) The following persons may compound a medicine, but only if under the direct personal supervision of a pharmacist:
(a) pharmacy graduates
(b) pharmacy technicians
(c) students
(d) despite subclause (1), dispensary technicians who have served an apprenticeship in a pharmacy under the Pharmacy Act 1939.
Did you pick up on the nine-word phrase we were looking for?
These are the words:"...IF UNDER THE DIRECT PERSONAL SUPERVISION OF A PHARMACIST..."
Technician scenario

Keeping in mind the statutory limitations on your role as a pharmacy technician, read this scenario:
It is an extremely busy day today in the pharmacy. The retail assistant hands you a prescription from one of your regular customers and says:
“Joe Bloggs wants to know how long it will take to get this filled. He’s in a hurry because he has to go pick up his kids from Kindy in 10 minutes”.
You know that it won’t take you long to get the prescription ready, but it will take a bit of time before the pharmacist will be free to carry out the final dispensing check.
You tell the assistant it will be a 20-minute wait and suggest Joe comes back later to pick it up.
10 minutes later, you have the prescription prepared and are awaiting the pharmacist's final check. The assistant says
“Is Joe Bloggs' prescription ready?”
You tell her you are waiting on the pharmacist's final check, which will be about another 10 minutes. She replies:
“I told Jo it would be 20 minutes and suggested he come back later, but he wanted to wait and said he wanted to collect it now. He’s getting really annoyed. He’s one of our regulars. Can’t you just give it to him now and tell the pharmacist later?”
How do you respond?
A) “Yes, because he’s one of our regulars and is in a rush.”
B) “No, because I can’t dispense without the direct personal supervision of the pharmacist, which means he has to check the medicines before they are given to the customer.”
C) “Yes, because the pharmacist is in the dispensary with me, so that counts as direct personal supervision.”
D) “No, because everyone has to wait for 20 minutes before they get their prescriptions filled because we are very busy today.”
The answer is:
B) “No, because I can’t dispense without the direct personal supervision of the pharmacist, which means he has to check the medicines before they are given to the customer.”
Self-directed learning activity
Answer these questions to confirm your understanding.
Congratulations! You have completed your second week of learning Professional Practice Part 1. Ka pai!

Controlled drug prescriptions
The laws that control and regulate Controlled Drugs (CDs) are:
- Misuse of Drugs Act 1975
- Schedule 1 lists Class A CD’s
- Schedule 2 lists Class B CD’s
- Schedule 3 lists Class C CD’s.
- Misuse of Drugs Regulations 1977
- Part 3 details the permissions and authority for CD’s under specified situations
- Part 4 details restrictions and conditions for prescribing CD’s
- Part 5 details the general requirements for CD prescription forms
- Part 6 details the registers, records and returns of CD prescriptions
- Misuse of Drugs Amendment Regulations (No 2) 2023
As you may know, CDs are any substance, preparation or mixture that is considered to have a high potential for abuse and/or dependence. These are listed in the Misuse of Drugs Act under three categories according to the level of risk or harm they may cause to people misusing them.
Controlled drugs can be prescribed by the following people, but they each have specific conditions and restrictions to what they can prescribe and the maximum period of supply.
| Medical and nurse practitioners | Must be an authorised prescriber |
| Dentist | Must be an authorised prescriber |
| Midwives | Must be an authorised prescriber |
| Pharmacist prescribers |
Must be a designated prescriber acting within their scope of practice |
| Designated nurse prescriber | Must be a designated prescriber acting within their scope of practice |
Under Section 8 of the Misuse of Drugs Act 1975, the following people may supply a controlled drug:
- A pharmacist
- A pharmacy technician under the immediate supervision of a pharmacist
In order to reduce the risk of harm from the misuse of controlled drugs, there are strict controls and restrictions on CD prescribing. Read pages 34-35 of the Pharmacy Procedure Manual to answer the following questions by selecting any or all that apply.
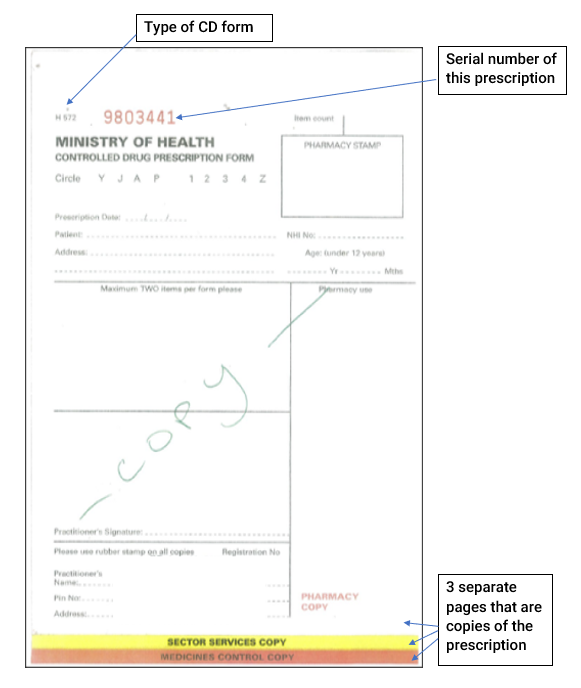
CD prescription format
The format of a CD prescription may be:
- Paper: Written on either an H572 or an H572 triplicate form and must be hand-written by the prescriber.
- Electronic: NZePS barcoded prescriptions that have been successfully scanned/downloaded at the point of dispensing.
Restrictions on CD prescribing labels
Some CDs have additional legal restrictions on their prescribing. Go to the Ministry of Health’s webpage, Restrictions on supply of certain controlled drugs, to find out which CDs have additional prescribing restrictions.
Specialist Recommendation
Both Dexamfetamine and Methylphenidate are CDs that require specialist recommendation on the prescription in order for it to meet legal requirements.
This means either a specialist writes the prescription themselves or an authorised prescriber will write the prescription under the specialist's recommendation. If this is the situation, the prescriber will have a letter from the specialist telling them what to prescribe. The prescriber will write on the prescription the name of the recommending specialist and the date of recommendation. The prescription is then valid for two years before the specialist recommendation needs to be renewed.
As a pharmacy technician, you will need to check that a prescription for Dexamfetamine or Methylphenidate has the legally required specialist recommendation. If it doesn’t, you cannot dispense the prescription.
Special Authority Number
For Dexamfetamine & Methylphenidate prescriptions to be funded, they must first meet the legal requirement of a specialist recommendation and also meet the funding requirement of having a special authority (SA) number.
To get an SA number, the prescriber puts in an application for a government subsidy for a particular person. Once approved, the prescriber is provided with a Special Authority number, which must appear on the prescription to gain the subsidy. SA numbers expire after 1-2 years, depending on the person’s age. As a pharmacy technician, you will be checking for a valid SA number so that the customer can receive the subsidy.
Consider this scenario
David Jones hands you a prescription from his GP for Dexamfetamine. This Controlled drug is part of his treatment plan from his specialist to help with his unwanted ADHD symptoms. The prescription is written on an H572 triplicate form. You check the prescription to see if it meets all the legal and funding requirements and notice that the specialist recommendation and SA number are not on the prescription. What can you do to find these important details? When you think you know, check your answer below.
In this situation, you would review David’s history on Tonqi, RxOne or TestSafe. If there are no details here, check with the patient if they have seen a specialist, then call the GP practice to ask for or to confirm these details.
Self-directed learning activities
Create a journal post in your online campus to record your responses to the following activity. Save and share it with your peers. Check out the journal posts of others to learn more.
- We have discussed the different classes of controlled drugs. Find at least two examples of class B drugs and two examples of class C drugs. For each drug, give the:
- Drug name or names
- The routes of administration. For example, how it enters the body - orally, inhaled, absorbed through the skin.
- The dose forms. For example, is it an oral liquid, tablet, or injectable liquid?
- What it may be prescribed for. For example, treatment of pain and treatment of allergic reactions.
- In order to reduce the harm caused by the recreational use of controlled drugs, there are various publicly funded programmes. One Programme is ‘Know your Stuff NZ (KYSNZ)’. You may already know about this programme. Visit KYSNZ and find out the following:
- What services do they offer?
- Who do they work with?
- Name the law that allows KYSNZ to check substances legally.
Ka pai tō mahi! Great work! That wraps up your second week of Introduction to Dispensing.

Routes of administration
You will be familiar by now with some of the different pathways or routes that medicine can enter the body. When a prescriber decides on a route of administration for a specific medication, they will consider the following factors:
- The pharmacokinetics of the medicine
- How the patient’s body will affect the medicine if taken in this way, including the bioavailability of the medicine if taken by this route
- The pharmacodynamics of the medicine
- How the medicine will affect the patient’s body if taken in by this route
- The urgency of the situation
- How quickly the medicine needs to work. This is called the onset of action
- The length of time the medicine stays in the body and produces an effect.
- This is called the duration of action and also relates to the dose and dose regime
- The advantages and disadvantages of this route of administration including:
- The ease, convenience, and acceptability of the route for the patient
- Unwanted side effects
- Potential for adverse reactions.
Routes of administration can be broken into three main categories, as shown in the graphic below.
Click on the hot spots to read about the three main routes of medicine administration.
What is the route of administration for each of the medicines listed?:
Now you have an overview of the three main routes, let’s take a closer look at each route in turn. Think about whether you know an example medicine that takes the described route before selecting the (+) to see if you are right or to learn one.
Topical Route
Example: Pimecrolimus cream is applied for the treatment of Psoriasis, a skin disease that causes a rash with itchy, scaly patches often on the knees, elbows, trunk, and scalp.
Example: Proctosedyl suppositories inserted into the rectum to treat haemorrhoids, which are swollen veins in and around the anus and lower rectum, similar to varicose vein.
Example: Canesten Clotrimazole internal vaginal cream for the treatment of vaginal thrush, a common yeast infection.
Example: Chloramphenicol ointment to treat bacterial conjunctivitis, a bacterial infection of the conjunctiva of the eye.
Example: Sofradex antibiotic drops for the treatment of inner ear infections.
Example: Budesonide, a steroid nasal spray used to alleviate allergy symptoms.
Enteral Route
Example: Cilazapril tablets to treat high blood pressure.
Example: Buccastem tablets for the treatment of nausea.
Example: Paracetamol suppository to treat pain and fever.
Parenteral Route
Example: Methylprednisolone is a strong steroid used to treat diseases associated with severe inflammation, such as severe allergic reactions and certain types of arthritis.
Example: Pethidine injection to rapidly treat severe pain.
Example: Insulin for the management of diabetes.
Example: Symbicort Turbuhaler for the treatment and management of asthma.
Here are two drag-and-drop activities to put the knowledge in a real-world context for you.
Advantages and Disadvantages
Have a think about your own experiences taking medicines, do some research, discuss with a pharmacy colleague, and then list what you think the advantages and disadvantages of each route of administration are.
Activity - Create a journal post with your thoughts on each route. Copy this template into your notebook. If you want, you can take a photo of your completed work and share it in your journal.
| Advantages: | Disadvantages: | |
| Topical | ||
| Enteral | ||
| Parenteral |
Dose forms

Dose forms refer to the way a medicine is formulated for delivery to the body. You will be familiar with the common dose forms used in a community pharmacy. For example, a medicine may be formulated as a tablet to be swallowed or a cream to apply to the skin. Other dose forms you will be less familiar with are those that are used in the hospital environment, such as intravenous solutions.
Dose form can be divided into four main physical types. These are named in the four dark green boxes in the graphic. Click on the hot spot for each type to see examples.
Dose forms not only contain the medicine, known as the active ingredient, but also inactive ingredients.
Inactive ingredients are:
- additives
- dilutes
- excipients
- preservatives.
Sometimes, a customer may be sensitive or allergic to the inactive ingredients used in the dose form for their prescribed or OTC medicine. They may ask for information to make sure that they are safe for them to take.
Read this health navigator webpage, Excipients in medicines, about inactive ingredients and answer the questions below.
Self-directed learning activities

As we already know, medicines can be given to a person in a variety of dose forms (the word forms is short for 'formulations'). They can be either solid, semisolid, liquid, or gas. Consider what you know about each dose form below before selecting the (+) sign to read more.
Intravenous drugs are injected directly into the bloodstream. In contrast, oral preparations must pass through the wall of the GI tract and blood vessel walls before entering the bloodstream.
An intravenous preparation might be appropriate for a drug when administered during surgery but would be inappropriate for home administration for Paracetamol.
The delay before onset of action varies between preparations of the same drug. Emergency situations often call for intravenous administration of drugs, which might normally be administered by another route.
Additional reading: Intravenous Medication Administration: What to Know
Drugs that are denatured by acid are not effective for oral preparations because they may be destroyed in the stomach.
Watch this video about Injection Techniques.
Blood containing the medicine from the gastrointestinal tract passes through the liver before entering any other organs. During this ‘first pass’ through the liver, part of the medicine (in some cases nearly all) can be broken down into an inactive or less active form. The breaking down of some drugs is so great that the medicine becomes useless when it is administered orally.
Another week of learning is done! Great work!
