Assessment Information
There are no assessments attached to this module.
You should use this time to work on Task 2 from assessment 02A1.
Last week, we looked at the systems and processes needed for receiving the stock we have ordered. This week, we’re looking at medicine recalls.

In today’s lesson, we continue to explore the practices, procedures, and responsibilities of a pharmacy technician in the management of dispensary stock.
Medicine recall
Occasionally, pharmaceutical manufacturers may find it necessary to initiate a "recall" of their products. What do you think is meant by a medicine recall, and what could be the reasons a manufacturer would take this action?
Take a moment to think about this before clicking on the ‘+’ sign below to compare your thoughts with the answer.
A recall means the removal of a therapeutic product, such as medicines, from supply or use. The reason for a recall can include issues with a product’s:
- safety
- quality
- efficacy
- performance.
Go to this page on the Medsafe website to learn more about the types, significance, and levels of recall action. Then, test your knowledge and answer the following five questions.
A recall action is conducted to an agreed level in the supply chain, depending on the distribution of the product and the severity of the issue.
| Supply Level | Description |
|---|---|
| Wholesale | Medicine and medical device wholesalers, suppliers and third-party logistics companies. |
| Pharmacy/retail |
Community pharmacies, medical, dental, and other health care practices. Other general retail outlets, e.g., supermarkets and health food stores, will also include wholesale, hospital/laboratory, and healthcare professional levels. This supply level recall affects pharmacy stock only. This means pharmacy staff will check their stock for the recalled items and remove them as instructed. |
| Consumer | Patients and other consumers will also include wholesale, hospital/laboratory, healthcare professional and pharmacy/retail levels. This supply level recall affects the stock that has already been dispensed to patients. This means the pharmacy will need to check their records and contact any patients who may have been dispensed the recalled item. They will instruct the patients to return the item back to the pharmacy. |
| Healthcare professional | Surgeons, consultants, specialists, dentists, pharmacists, general practitioners, nurse practitioners, etc. (i.e., any healthcare professional supplying, prescribing, or using an affected medicine or supplying, using, monitoring, checking or having implanted a medical device). |
| Hospital / Laboratory |
Hospitals, including private hospitals and residential care facilities, nursing homes and other healthcare facilities. Clinical trial sites, hospital pharmacies, blood banks, pathology laboratories, and personnel in other hospital departments will also include wholesale and healthcare professional levels. |
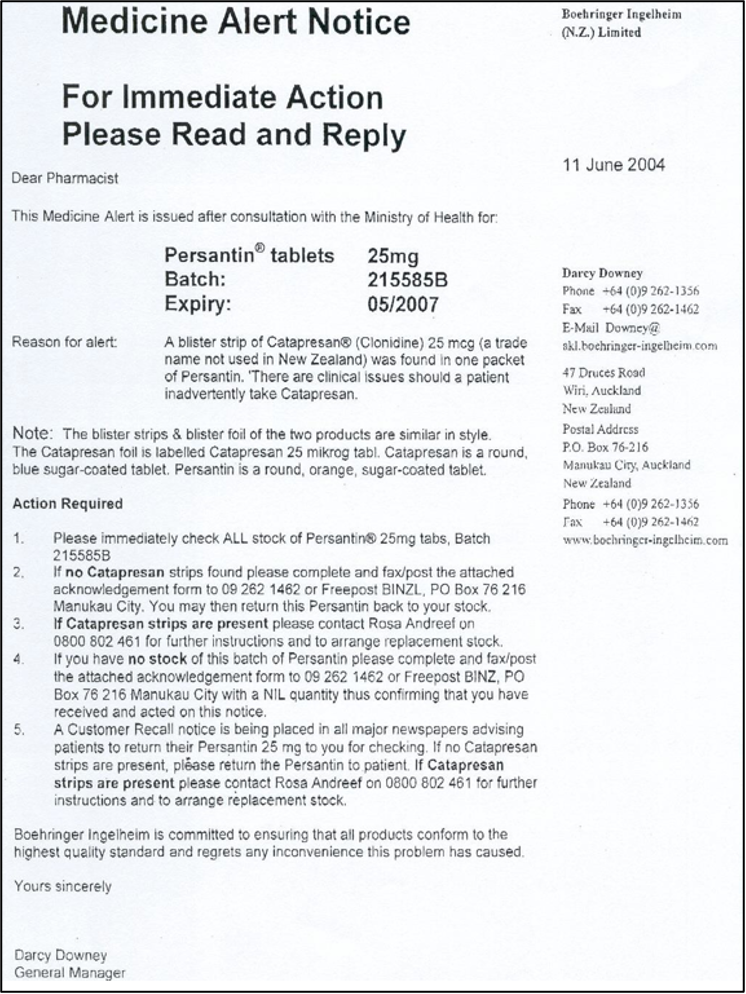
Below, you will see an example of what a recall notice looks like. This notice was for Persantin® (generic name dipyridamole), a drug prescribed for secondary prevention of ischaemic stroke and transient ischaemic attacks. The organisation that issued the recall was the drug company Boehringer Ingelheim. In the notice, you will see the reason for the recall was because a blister pack of a different drug, Catapresan® (generic name clonidine), was found in a packet of Persantin. Catapresan® is used to treat migraine and menopausal symptoms. Using Catapresan® might cause low blood pressure, a dry mouth and sedation.
This is the black-and-white version of the customer recall notice for this product:
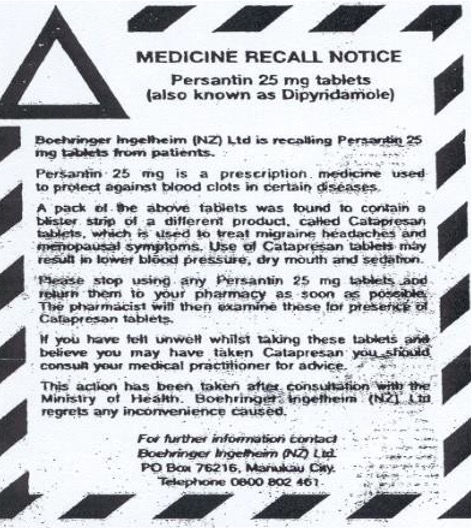
Read through both images of the notice carefully and answer these three questions.
Activity
Now, let's look at a more recent recall from October 2019.
Watch: Zantac and its generic version found with [...] (4:14 minutes)
1. Watch the 4-minute video below from a US television broadcasting company’s news clip about a medicine recall. To help your learning, answer the following questions in your notes.
- What medicine was recalled- generic and trade name?
- What was the reason for the recall?
2. Read this Stuff News article from the same time to see the response to this recall in Aotearoa New Zealand.
Stock return
There are instances when stock needs to be returned to the supplier. This may include when:
- you have ordered the incorrect item
- you have ordered an item, but an incorrect item has been sent to you
- you have been sent an incorrect quantity
- you have been sent expired or short-dated stock
- you have been sent damaged stock.
The steps for returning stock in these situations are:
- Record the invoice number, date, time and what the problem is.
- Notify the supplier of the error and discuss the appropriate procedure to resolve this issue.
- File all paperwork associated with the event and prepare the stock for pickup to be returned to the supplier.
- Ensure computer stock levels are accurate given stock return.

Damaged stock
There are many ways stock in a pharmacy can be damaged and, therefore, no longer be supplied to customers. Take a moment to think about how damage may occur in each of the following situations, and then click the (+) sign to check your knowledge.
- Rough handling of packages by delivery staff and during transit may lead to broken containers, damaged labels, or compromised packaging.
- Extreme temperatures, exposure to moisture, or prolonged exposure to sunlight during transit can affect the integrity and efficacy of pharmaceutical products.
- If pharmacy staff mishandle the stock during the unpacking process, it can lead to breakage, spillage, or damage to the packaging and stock.
- Lack of attention to detail while unpacking can result in accidental damage to fragile items.
- Not putting received stock away into correct storage immediately means the environment can damage the stock or be damaged by people bumping or tripping over packages.
- Inadequate organization or overcrowding of shelves and display units can lead to items falling, getting crushed, or being mishandled by customers or staff.
- Failure to maintain proper temperature control in the refrigerator can impact the efficacy of temperature-sensitive medications.
- Mishandling or accidental dropping while accessing stock from the safe or behind the counter can cause damage to the products.
- Customers who tamper with packaging or open containers inappropriately can lead to contamination of the stock, rendering it unsellable.
- Appropriate storage conditions are not followed, e.g. a fridge item is put on a normal shelf.
- Customers may accidentally drop or mishandle products while collecting them from the pharmacy, resulting in stock damage.
- Failure to take care when putting items in a carrier bag, overloading a carrier bag or, while handing items to the customer, accidentally dropping, breaking, spilling, or damaging them.
Read this scenario:
You are on work placement in a community pharmacy. You have gone to the dispensary to select a box of medicine from the stock shelves. When you pick up the box, it is damp. When you look closer, you see there is water pooling on the shelf under several boxes of medicine. The water also is dripping down onto the stock on the shelf below. You look around and notice there is a slow leak of water coming from the ceiling.
Answer the following questions in your notes. When you are done, review your peers’ responses and see if they have similar or different responses to you.
- What immediate actions do you take?
- What is likely to happen to the water-damaged stock?
- What are the likely consequences for the pharmacy and pharmacy customers of this situation (damaged stock)?
Stock can also be lost through administrative errors such as:
- human error when entering the stock into the computer system
- stock cards are not updated when brands change over, or the wrong brand is dispensed in the computer system
- stocktake is completed incorrectly and infrequently
Stocktake of non-controlled drugs
A regular stocktake of non-CDs is an important business practice for ensuring that the physical number of stock and the number on the computer record are the same. This is the most accurate way of identifying stock loss and helps us understand where our stock is going, e.g. sold, expired, stolen, or damaged. You may remember discussing stock and stocktake in your level 3 programme.
There are different types of stocktake, which include the following:
- Periodic stocktake: Physical inventory counts at specific intervals, such as monthly, quarterly, or annually. It may involve shutting down operations temporarily to count all items in stock.
- Rolling stocktake: Specific sections of inventory are counted regularly throughout the week when the pharmacy is not busy. This ensures that all items are counted at least once during the year without the need for closing down the pharmacy.
- Random spot check: This may be a stocktake of a random sample of items to check and verify that the stock count is correct with no discrepancies. A spot check may also occur after a discrepancy has been found in order to find out more about the issue
The practices and procedures for stocktake in a pharmacy include:
- A stocktake should be performed in the dispensary every six months.
- The dispensary manager/pharmacy manager is responsible for the stocktake.
- The task can be delegated to any/all dispensary staff.
- Before updating stock levels, check for reasons for discrepancies. There may have been a mix-up between blister packaging stock and dispensing stock, a dispensing error, or some other reason.
- Large discrepancies should always be investigated before changing stock levels after a stocktake.
Here’s how to stocktake using Toniq:
- Press 3 (Stock Reports) → Press 7 (stock reports)→ Press 1 (stock check).
- There are some fields you can tick here depending on how your pharmacy organises the dispensary, e.g., Generic / Brand.
- Type the letter of the alphabet of stock you want to stock take, e.g., letters A-C.
- Press F12 (create report) → Press F9 (print report).
- Count the stock items and enter the correct figure. If there is a discrepancy, continue until all items have been checked.
- Annotate the stock form with your name and initials.
- Update the computer stock level.
Stocktake of controlled drugs
There are legal requirements when it comes to the stocktake of controlled drugs.
In the appropriate piece of legislation, find out how often a pharmacy is legally required to carry out a stocktake of their controlled drugs. Record your answer in your notes.
Self-directed learning activity
Medicine Recall:
MORD stands for the Medsafe Online Recall Database.
- Use your internet searching skills to find this database.
- Once you have found the database webpage, read the explanations of the database and recalls, then search the database for:
- Brand name: Zantac
Ingredient: Ranitidine Hydrochloride
Commencement date: [You do not need to fill in this field, just click the ‘search’ button.]
- Brand name: Zantac
- Find out the following and record the answers in your notes.
- What organisation recalled Zantac film-coated tablet 150mg?
- What organisation recalled Zantac double-strength tablet 300mg?
- What was the issue stated with the above tablets?
- What level was the recall for the above tablets?
- When was the recall commencement date for the above tablets?
- What organisation recalled Zantac solution for injection 50mg/2ml?
- What was the issue stated with the solution for injection?
- What level was the recall for the solution for injection?
- When was the recall commencement date for the solution for injection?
- Today, can a healthcare provider prescribe Zantac tablets or a solution for injection?
Stock Damage:
What practices and procedures does your pharmacy carry out to reduce the likelihood of stock loss due to damage? Record your answers in your notes.
Tau kē (fantastic) – you have completed this week's learning of Professional Practice Part 1!

Graduated glass measuring cylinders are used for measuring liquids.
Reconstitute medicines as a pharmacy technician
As a pharmacy technician, you will be involved in the reconstitution of medicines. It is important that you understand the practices and procedures to do this in a safe and hygienic manner.
In the table below, review some terminology related to reconstitution.
Solutions versus Suspensions
The words suspension and solution are not interchangeable. They mean different things. Carry out your own research to learn about the meaning of each word, and use the Document tool to save your work as a resource.
Here are a few of the key differences between solutions and suspensions.
- When a solution is correctly prepared, it’s transparent when exposed to light.
- In a suspension, the size of the particles is larger than in a solution.
- A suspension is a heterogeneous mixture.
What do you think are the reasons some medicines are in powder form for reconstitution at a later time?
- Stability: Some medications, especially antibiotics, may have limited stability when dissolved in liquid form. By providing them as a powder, the active ingredients are protected from degradation and maintain their potency for a longer period. This allows for a longer shelf-life of the medication.
- Convenience: Preparing medications in powder form allows for greater flexibility in dosing. Different strengths can be achieved by adjusting the amount of powder and diluent used during reconstitution. This provides healthcare professionals the ability to customise the dosage according to the patient's needs.
- Storage and transportation: Powders are often more stable and easier to store and transport compared to liquid formulations. They occupy less space and are less prone to leakage or spillage during handling and transportation.
How did you do? Did you get some or all of these reasons?
Solutions
Now that you know the difference between a solution and a suspension, let’s look at an example of an oral solution that requires reconstitution.
In this scenario, the solution is reconstituted by the customer at home.
 Source: Bargainchemist.co.nz Source: Bargainchemist.co.nz |
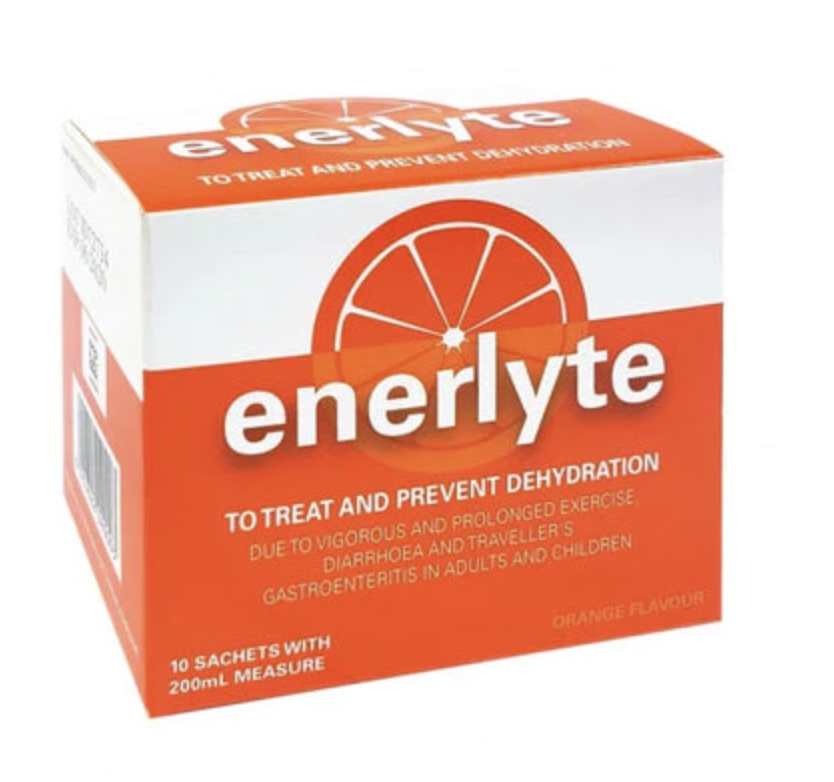
Mathew has come into the pharmacy to purchase Enerlyte® for his husband Paul. Paul has food poisoning, and his doctor recommended he take Enerlyte® - an oral rehydration solution to replace the fluids he has lost through vomiting. Enerlyte® comes as 10 individual powder sachets in a box. The box also contains a 200ml plastic measuring container. Each sachet, when mixed with the specified amount of liquid, is one dose of Enerlyte. |
What advice would you give Mathew about how to reconstitute this product?
Write your answer down in your own notes before clicking on the plus sign to reveal the key points. You may want to research this product to help you with your notes.
Researching and making your own notes first is an active learning strategy that will help you learn and remember!
- Read and follow the instructions on the packaging for how to prepare the solution.
- Never take without mixing with water first.
- Use fresh, cold drinking water in the amount stated.
- Use the measuring cup to measure the water.
- Add contents of sachet(s) to the water- (use the stated quantity of sachets).
- Stir well to mix before drinking.
- Follow instructions for how long it can be kept after mixing and where it should be stored (usually in the fridge).
- Do not boil or freeze the solution.
Suspensions
In a community pharmacy, the types of medications that a pharmacy technician will most commonly reconstitute are antibiotic oral suspensions. Examples include:
- Amoxicillin
- Amoxicillin & clavulanic acid (Augmentin)
- Flucloxacillin
- Trimethoprim
- Cephalexin
- Azithromycin
The components of an oral suspension are:
The Solute:
This is the active ingredient or ingredients. It is medication in a solid form, often referred to as ‘the powder’. It may also contain excipients or inactive ingredients, such as stabilizers or fillers.
The Dilutant:
This is the liquid, inactive ingredient. The liquid is usually tap water unless otherwise specified on the instructions.
Reconstitution process
Let’s look at the practices and procedures involved in the reconstitution process.
For those who have experienced reconstitution in the workplace:
Reflect and provide a brief explanation or list, of the practices and procedures you encountered during the reconstitution process. You can highlight the key steps, safety measures, and any other essential aspects that you found noteworthy.
For those who haven't experienced reconstitution yet:
Reflect and write a brief explanation, or list, of what you think might be involved in the practices and procedures of the reconstitution process. Consider key steps, safety measures, and any other steps in the process.
Self-directed learning activity
For this week’s SDL, spend some time reflecting on the topics and sub-topics in ‘Introduction to Dispensing’ that you have covered so far.
You may want to carry out the following activities to support your learning:
- Create a list of the topics and sub-topics in this course.
- Review key learning points.
- Make notes to consolidate.
- Prepare for upcoming assessments.
- Organise your previous notes.
- Do any extra reading or research required to help fill in any learning gaps?
- Find the answers to any questions you may have- you might want to talk to fellow students, your tutor, or staff in your work placement.
Ka pai, good work - that’s another week of Introduction to Dispensing completed!
This is an illustration of the Escherichia Coli bacteria. This bacteria is commonly known as E.Coli and can cause illnesses such as food poisoning, urinary tract infections and pneumonia.
In the last lesson, we looked at the structure and shape of bacteria. To review your learning, answer the following questions.
The bacteria that colonise (live on) the human body thrive in warm, moist conditions. Bacteria obtain their nutrients by absorption from the environment.
Some are:
Aerobic: They require oxygen to grow and multiply. Most commonly found on the skin or in the respiratory system.
Anaerobic: They thrive where there is no oxygen, for example, deep within tissues or in wounds.
Bacteria reproduce by dividing. This is called binary fission (asexual reproduction). Under ideal conditions (exactly the right temperature and sufficient nourishment for all cells), this division can occur every 20 minutes, an extremely rapid reproduction. After only six hours, a single bacterium can multiply to form a colony of 250,000 bacteria. This very rarely happens, however, because ideal conditions rarely occur, and in a healthy individual, the body’s immune system destroys the invading bacteria.
As we know, not all bacteria on and in the human body cause illness.
Bacteria are important in the following ways:
- GI Bacteria - Bacteria in the gastrointestinal tract provide essential functions such as aiding in digestion and breaking down dietary fibre.
- Vitamin synthesis - Bacteria in the gut can create certain vitamins that are essential for biological processes. These vitamins include vitamin K, biotin, and folate.
- Nutrient production - Some bacteria produce beneficial compounds in the body, such as short-chain fatty acids (SCFAs) in the gut. SCFAs serve as an energy source for the cells lining the colon and support a healthy gut environment.
- Immune system development - Certain bacteria assist in training the immune system to recognize and respond appropriately to pathogens.
- Protection against pathogens - The presence of beneficial bacteria can help prevent the colonisation of harmful pathogens. By occupying specific environments and competing for resources, beneficial bacteria can inhibit the growth of pathogenic organisms, thereby protecting the body from infections.
Watch: Bacterial Pathogenesis (10:48 minutes)
Let’s look at the ways that bacteria are harmful and cause damage and illness to humans. Watch the video below as Professor Dave explains ‘bacterial pathogenesis’ and the defences that our bodies have against bad bacteria, and then answer the following quiz to check your understanding.
How did you go? Don't worry if you didn't get all the questions correct; take this as a learning opportunity and note those answers down to help you recall them in the future.
Treatment of bacterial infections
The antimicrobial agents that bacterial infections are treated with are antibiotics. A group of medicines that you will be familiar with and will learn more about as you continue your learning.
Antibiotics were originally obtained from moulds and fungi but are now produced synthetically. The first antibiotic was discovered in 1928 by Sir Alexander Fleming, which we know as penicillin.
Currently, there is a wide range of antibiotics available, which are grouped into different classes. These classes include:
- Penicillins
- Cephalosporins
- Tetracyclines
- Macrolides
- Quinolones
- Sulfonamides
- Aminoglycosides
Each class of antibiotic destroys bacteria either directly or by inhibiting their ability to carry out specific functions for survival and growth.
Antibiotics are divided into two spectrums:
| Narrow Spectrum | A type of antibiotic that targets specific types of Gram-positive or Gram-negative bacteria. | Example: Vancomycin is primarily effective against gram-positive bacteria, such as staphylococcus aureus (skin and soft tissue infections) and streptococcus pneumonia (pneumonia and meningitis). |
|---|---|---|
| Board Spectrum | A type of antibiotic that can affect a wide range of bacteria. | Example: Cephalosporins (like Cefaclor). Cefaclor may be considered a second-line treatment for otitis media, sinusitis, cellulitis, diabetic foot infection and mastitis. |
When a health practitioner decides that a patient requires antibiotics to treat an infection, there are several factors to consider when selecting the most appropriate type to prescribe. Let’s look at a typical scenario:
Mary cut her finger last week with a kitchen knife while chopping vegetables. She cleaned the wound and could see it wasn’t very deep. She covered it with a dressing and went about her usual activities. Over the last two days, the cut has become painful, and on inspection, the skin around the wound is inflamed, red and hot.
What do these signs and symptoms indicate?
That the wound has become infected.
Mary decided to visit her GP, who confirmed the wound had become infected. The GP said it was important to swab the wound to get a specimen of the bacteria to send to the lab for testing.
The purpose of this testing is to:
- to confirm the infection has been caused by a bacteria
- to identify the strain of bacteria
- to identify if the bacteria is gram-positive or gram-negative
- to identify which antibiotics are appropriate for treatment.
The doctor said it may take several days to get the results, so in the meantime, he will prescribe an antibiotic for her to start today.
Why did he do this and not wait for a few days for the results?
Infections can worsen if treatment is delayed.
After speaking with Mary and confirming she had no allergies and any contraindications, the doctor prescribed a 10-day course of Flucloxacillin oral capsules. He told Mary he would contact her when the lab results came in. He would then advise her if she should continue on the Flucloxacillin or if he needed to change her to a different antibiotic.
A few days later, the lab results confirmed the infection had been caused by staphylococcus aureus. The doctor tells Mary to continue on the Flucloxacillin as prescribed until the full 10-day course of treatment has been completed. On day 8, Mary notices the wound looks fully healed. She wonders if she can stop the antibiotics now.
Why is it important for Mary to take the last two days of her 10-day course of antibiotics?
- To make sure the bacteria are fully eliminated
- Minimise the risk of antibiotic resistance developing
Resistance and super bugs
You have already come across the term resistance in relation to antibiotic use. Let’s now review what we know about microbial resistance and the development of ‘super bugs’.
Bacteria, like all organisms, are programmed to survive. There are two types of microbial resistance:
- Intrinsic: This resistance is usually a result of specific characteristics or features of the bacterial species that make them naturally less susceptible to the effects of certain drugs. These characteristics are having an impermeable cell membrane that resists antibiotics getting into the bacteria, bacterial enzymes that can inactivate specific antibiotics and pumps that actively pump out antibiotics from within the bacterial cell.
- Acquired: This resistance is when bacteria that were previously susceptible to an antibiotic acquire mechanisms to resist its effects. These mechanisms are mutation, transfer of resistance genes from one bacterium to another, and the use and misuse of antibiotics create selective pressure, favouring the survival and growth of bacteria that have acquired resistance.
Take a moment to think about reasons why bacteria developing resistance to antibiotics is a concern to humans.
- As more bacteria become resistant, fewer options remain for treating infections caused by those bacteria.
- Infections may become untreatable, resulting in more severe illness and life-threatening consequences.
- A person is infectious for longer; therefore, there is more opportunity to spread and pass the infection to others.
- Treating resistant infections requires more money and resources, including additional hospitalization, longer treatment durations and more complications.
- More money and time are needed to develop new antibiotics or alternative treatment strategies.
How did you go? You can see why there are a few reasons why this is a concern. Antibiotic resistance has led to the development of ‘superbugs’. Read this news article to learn what a superbug is and its impact on human health. Make your own notes with the key points in your notes.
Self-directed learning activity
Watch: Bacterial Infections in Humans (9:21 minutes)
Mātakitaki mai (watch it), watch the following video from Professor Dave on bacterial infections in humans, then answer these questions in your notes:
- What is meant by the incubation period?
- What factors determine the length of the incubation period of a disease?
- What is the prodromal phase of an illness, and what symptoms is a person likely to experience in this phase?
- What is the name of the phase of an illness when a pathogen reaches peak toxicity, and what are the common symptoms in this phase?
- What is the convalescence phase, and are pathogens still present in the body during this phase?
- What happens to pathogens if a person stops taking their antibiotics during the convalescence phase?
- Describe the pattern of infection in a latent infection such as tuberculosis (T.B.).
- Do people who are carriers of infection experience symptoms of the disease?
- At what stage of the infection cycle can infectious diseases be transmitted from one person to another?
- What is the difference between a localised and a systemic infection?
- What is the name given to the natural habitat of a pathogen? Give two examples of a natural habitat.
- What is horizontal transmission of disease?
- Explain the oral faecal route of transmission.
You’ve completed another week of learning, ka rawe (awesome)!
