This week, we will start the learning with information about preparations and concentrations.

Pharmaceutical preparations & concentrations
As a pharmacy technician, you need to understand the concept of concentration related to pharmaceutical preparations.
Pharmaceutical preparations consist of:
- Ingredients = active and inactive substances, often a solid.
- A vehicle = a substance that helps deliver the active ingredients to the desired site of action, usually a liquid.
In pharmacy, when we are compounding, we are combining specific amounts of ingredients with a specific amount of a vehicle to make a pharmaceutical preparation to meet the needs of our patients. For example, the doctor has prescribed omeprazole suspension for a patient who has difficulty swallowing capsules. In this situation, we would combine omeprazole powder (active ingredient) and sodium bicarbonate powder (inactive ingredient) with water (vehicle) to make a suspension that the patient can easily swallow.
When we make a pharmaceutical preparation such as the omeprazole suspension in the example above, it is crucial that we follow the SOPs for compounding and the instructions for the specific preparation. This includes selecting, calculating, measuring, and mixing the right amounts of ingredients and vehicles. If we do not do this, the patient is put at risk of serious harm.
- They would not get the desired effect and treatment for their health concern.
- They may experience adverse reactions.
- There is a potential for an overdose.
- The stability and effectiveness of the preparation are impacted, making it ineffective.
- The taste and texture are not acceptable, so the patient won’t want to take it.
In pharmacy, concentration is an expression of the ratio of the amount of an ingredient to the amount of product. It is written in fraction form, where the letter ‘w’ refers to a weight and the letter ‘v’ refers to a volume.
| w | weight |
| v | volume |
We will now take a look at some examples of concentrations of pharmaceutical preparations.
|
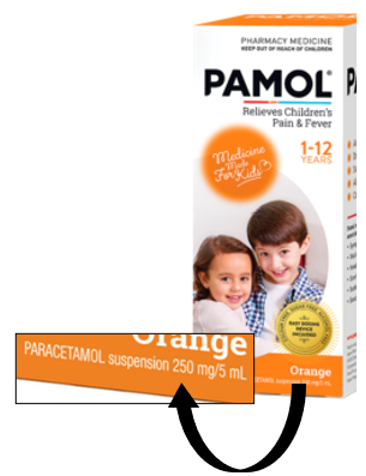
w/v: In the case of a solid ingredient in a liquid vehicle, the ratio is expressed as weight per volume or w/v. Example: Pamol ® suspension. Our solid ingredient is paracetamol, measured in weight (mg), and our liquid ingredient is an orange-flavoured syrup measured in volume (ml). |
 |
|
v/w: If a liquid ingredient is formulated into a solid vehicle, the ratio is expressed as v/w. Example: 10% Glycerol in non-ionic cream. In this example, the glycerol is the liquid ingredient measured in volume. The non-ionic cream is considered the solid ingredient because it is measured in weight. |
 |
|
v/v: If both drug and vehicle are liquids, it is expressed as v/v. Example: Xerostom® mouth spray. In this example, the drug pilocarpine (generic name) is the liquid ingredient measured in volume, in a liquid ingredient (a mixture of different types of oils and liquids). Both ingredients are measured in volume. |
 |
|
w/w: If both the drug and the vehicle are solid in nature, the ratio is expressed as w/w. Example: 0.5% Hydrocortisone in Cetomacrogol cream. In this example, the hydrocortisone is the solid ingredient measured in weight, and the cetomacrogol cream is also the solid ingredient measured in weight. |
 |
Complete this scenario-based activity. We’ll help you determine the dose based on the concentration.
Consider this scenario:
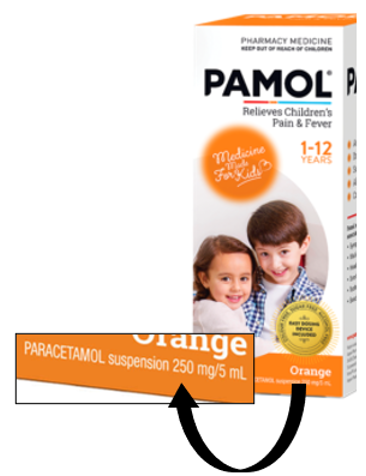
Sal has this bottle of Pamol® suspension. This is an OTC product. The label says that it contains 250mg in 5ml. What volume of this suspension is needed to give a 300mg dose?
You could take this approach:
Start with estimating:
We estimate our answer has to be more than 5ml because we already know that every 5ml of suspension contains 250mg. 250mg is smaller than the 300mg dose that we want. Therefore, our answer must be more than 5ml. Knowing this helps us to check if we made a mistake in our calculations. It would not make sense to get an answer that was less than 5ml.
Lay out the calculation:
x = the quantity in ml that we are trying to find out.
- We want: 300mg in xml
- We have: 250mg in 5ml
Our calculation in numbers looks like this:
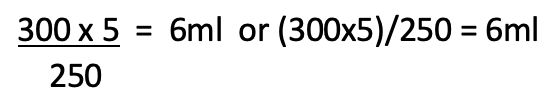
This means Sal should measure out 6ml of this suspension in order to get 300mg of paracetamol.
This is just one method to work out the answer. You may have a different method to arrive at the same answer.
Using your preferred method, work out the solutions to the following scenarios using Pamol (250mg in 5ml) as the medicine. Then, click the label or the '+' sign to view each answer.
Moana was given 10ml of Pamol suspension.
500mg
Thomas is prescribed a 125mg dose of Pamol.
2.5ml
Charles is given 15ml of Pamol.
0.75g
We want to give Mei 50mg of paracetamol using this bottle of Pamol.
1ml
You will be required to calculate the correct quantity of medicine to dispense for each prescription to ensure the patient receives an adequate supply to last for the duration of their prescribed treatment.
Consider another scenario:
Iosefa comes into your pharmacy with a prescription for his 2-year-old daughter. She has been prescribed 6ml of paracetamol suspension 120mg/5ml, four times daily for five days. How many ml will you dispense?
Write your answer on a piece of paper and show how you got to that number.
6ml x 4 doses = 24ml
24ml per day x 5 days = 120ml
Dispense 120ml
You may also be asked to calculate a dose and the quantity to dispense based on body weight. For example:
- A young patient who weighs 9kg is prescribed Ibuprofen 100mg/5ml suspension. The prescription states the patient is to have 7.5mg/kg tds for 1/12.
To work this out, we will start by asking ourselves: what is the dose in ml that the patient requires?:
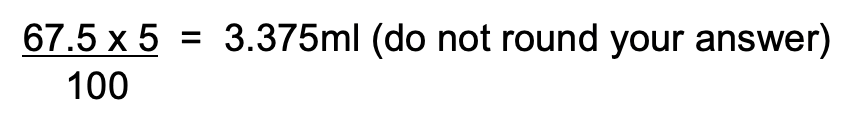
- 7.5mg x 9kg = 67.5mg
- We want: 67.5mg in xml
- We have: 100mg in 5ml
Therefore, our calculation will look like this:
Now that we know these numbers, we can move on to the second part, which is finding out the quantity to dispense.
- We know that tds means three times per day.
- We know that 1/12 means 30 days.
Therefore, our calculation will look like this:
- 3 x 3.375 x 30 = 303.75ml to be dispensed
Calculate the answers for the following. You will find out if you are right immediately, and the activity will automatically progress through all five questions.
Let’s now move on to another scenario where you are required to calculate the total quantity required to dispense.
Have a go!
Look at the following prescription:
Sugar Tablets 50mg
Sig. 2t od for 1/52 then 2t bd for 2/52 then 4t bd for 3/52 then 5t bd
Mitte. 12/52
Please dispense in 4-week lots.
At first glance, this may look complicated, but on closer inspection, you will see that you already have the skills to find the answer.
Ask yourself the following questions:
- If I received this prescription, what would I need to do in order to dispense it?
- Do I understand all of the abbreviations?
- How many 4-week lots are there in the period of supply for 12/52?
Your challenge is to find out how many tablets to dispense for each of the 4-week lots in this prescription.
Forum discussion
Document your answers and how you went about calculating the quantities for each 4-week lot. Then, share your work with your classmates on the forum. By sharing your methods with your classmates, you get to discover new methods and support each other in your learning.
Self-directed learning activities:
Take the following seven-question quiz to ensure you can perform the required calculations.
Excellent job! You completed week 7 of Professional Practice!
Cautionary and advisory labels
The Pharmaceutical Society of NZ’s (PSNZ) Cautionary and Advisory Labels (CALs) have an important role to play. Given its name, take a moment to consider what you think that might involve.

CAL's role is to oversee additional label information placed on medicine to:
- prompt counselling of customers on specific advice
- prevent or reduce adverse reactions
- warn of important side effects
- ensure the medicine is taken in the most effective manner
- meet the professional and legal obligations regarding medicines information.
Can you think of any medicine warning labels you see regularly as a consumer?
The professional and legal obligation to provide CALs are contained in the following documents:
- Pharmacy Council Code of Ethics 2011
- Code of Health and Disability Services Consumer Rights 1996.
| CALs may be a separate brightly coloured label (recommended by the PSNZ) or abbreviated forms of the CALs can be printed on the dispensing label. |  |
When attaching CALs, it is important that they are placed so that they do not cover up the main label directions. Generally, they should be used regardless of whether an abbreviated version of the label is included in the main label.
A prescriber who, for any reason, does not wish a Cautionary and Advisory Label to be used in a particular case should endorse the prescription with ‘N.C.L’, which stands for ‘No Cautionary Label’.
When a patient or their representative collects a prescription that has a CAL attached, it is important that the person handing over the prescription ensures the CAL information is pointed out and explained verbally.
For each of the CALs listed below, click on each label or (+) symbol to read the full advice and information:
The intent of this label is NOT that people should stop taking the medicine if they intend to drive or operate machinery, but that they should determine whether or not drowsiness is a problem. For some medicines, it is important to advise that the medicine should always be taken in order to continue being able to drive, e.g. antiepileptic medicines to prevent seizures, but to be aware of the possibility of drowsiness.
This label applies to all medicines with effects that include sedation or products that contain an ingredient having sedative properties. A label of this nature is already required by law in the sale of some over-the-counter medicines.
The term limit is included on the label to indicate that alcohol consumption is not prohibited but should be moderated. This is to reduce the probability of patients stopping their medicines so as not to interact with their alcohol intake while reinforcing that excess alcohol is not recommended.
This label applies to medicines where alcohol is not recommended either through additive risk of sedating effects, alcohol altering the metabolism of the medicine, or the medicine may alter the metabolism of alcohol, causing adverse effects.
This label applies to medicines with actions that are decreased in the presence of food.
This label applies to those medicines with actions that are significantly altered by antacids, iron, or calcium.
This label is not used on many medicines but applies to those where certain foods or drinks may significantly affect the use of the medicine, such as monoamine oxidase inhibitors (MAOIs) and tyramine-containing foods.
This label is included on those medicines whose metabolism or actions are commonly altered by the concurrent use of other medicines eg. warfarin, ciclosporin, oral contraceptives, etc.
It is intended to be a prompt to seek professional advice whenever another medicine is prescribed or before purchasing over the counter.
The storage conditions for many medicines are critical. This label will apply to those preparations where storage at temperatures between 2º and 8ºC is necessary.
Products should not be frozen since this may also result in a loss of activity or destabilisation.
Certain products have a short shelf-life due to chemical instability or the possibility of bacterial contamination.
Dilution or admixing of medicines affects the strengths of preservatives, stabilising agents, suspending agents, etc., and the stability of the preparation cannot be guaranteed after a certain time.
Ophthalmic preparations, in particular, carry the risk of contamination once the container is opened. Breakdown or loss of the preservative can occur, and coupled with the risk of bacterial contamination, the use of these products after their “use by” or “expiry” may be harmful.
Some medicines cause serious photosensitivity reactions when people taking them are exposed to sunlight.
Since it is not possible to predict an individual’s response to a photosensitising medicine, it is considered desirable for a warning label to be attached to medicines that have been shown to cause photosensitising reactions.
This label is specifically applied to medicines that cause a reaction upon abrupt withdrawal, which is greater or different from that which would be expected to occur if the condition had been left untreated. These may occur through the development of new symptoms or a rebound effect of the condition being treated.
This label is also recommended for medicines where a break in treatment is extremely undesirable, such as in tuberculosis and HIV, which may lead to resistant strains.
While all solid dose forms of medicines should be taken with water while sitting or standing upright, this label is commonly used on medicines that have been implicated as causing adverse effects if retained in the oesophagus.
This label applies to those medicines whose absorption or metabolism is considerably altered by grapefruit or grapefruit juice, and there is a risk of significant clinical effects. Clinicians should refer to drug interaction information for more detailed advice on significance and management.
This label is applied to medicines that are strictly for external use only.
An instruction to shake the bottle before measuring the required dose in order to ensure the medicine is evenly dispersed. Often used for suspensions.
*Note: There is no Label 12.
As well as CALs, there are also dispensing label references that can be added to the labels as appropriate. These are:
- Ref A: swallow whole; do not crush or chew
- Ref B: with food
- *Ref D: until the medicine is finished
*Note: There is no reference C.
You've just taken a lot of information on board, so have some fun and check your knowledge by answering the next ten questions about CALs. Don't worry if you don't get them all correct. Just make sure to note down the correct answer so that you can remember it going forward. Have fun!
Self-directed learning activities
For your SDL activity this week, we would like you to reflect on your knowledge of CALs with medicines that you have at home. If you find anything that interests or surprises you, feel free to discuss it with your tutor and peers when you're next in class.
- If you have a prescription medicine at home, take a close look at the printed medicine label. If you don’t have one of your own, perhaps someone in your household is happy for you to look at one of theirs.
- Does it comply with the label legislation?
- Does it have any CALs?
- Look at the words used, the label placement and all the other features you have learned about.
- Take a closer look at a non-prescription or OTC medicine.
- Examine the packaging for:
- the wording used
- instructions
- information.
- Are there any warnings?
- How are they similar, and how are they different to the labels for prescription medicines?
- Examine the packaging for:
Another week of Introduction to Dispensing is complete. Well done.

Pain
Each kind of pain medicine has benefits and risks. Some types of pain respond better to one kind of medicine than to another kind. As we know, pain is felt differently for each person, and what works for one person’s pain may not work for someone else.
Take a moment to study and learn the terms in the completed activity.
OTC pain-relieving medicines work by reducing the effect of a chemical called prostaglandin. Prostaglandins act as chemical signals that control different processes in the body, including the transmission of pain signals to the brain and signals to the body to cause inflammation and fever—reducing or blocking the effects of prostaglandins results in the relief of pain, inflammation, and fever.
Paracetamol
Paracetamol is used to treat mild to moderate pain. It is thought to work by blocking prostaglandins from transmitting pain signals from the nerves in the spinal cord up to the brain.

Answer these three questions about paracetamol.
Paracetamol overdose can occur accidentally or in the context of self-harm. As a result of paracetamol being metabolised (processed) in the liver, a small amount of a toxic compound is formed, but the liver is able to detoxify this quickly. In an overdose, the liver cannot keep up with the amount of detoxification needed, which results in a build-up of the toxic compound. The build-up damages the liver and causes it to fail. It can take several days for the effect of a paracetamol overdose to be felt, by which stage it is too late to treat the overdose, and the person will die.
Alcoholism and heavy drinking damage the liver and its ability to function. Therefore, these people, along with those who have impaired liver function for other reasons, are at risk of a paracetamol overdose due to the liver not being able to metabolise it.
Ibuprofen
Ibuprofen is used to reduce mild-to-moderate pain and inflammation. It works by stopping the damaged or infected body tissues from producing prostaglandins.

Answer these questions about ibuprofen.
As with Paracetamol, an overdose of Ibuprofen may not be felt right away. Mild symptoms include ringing in the ears, GI disturbances, rash, blurred vision, and sweating. Severe symptoms include low blood pressure, difficulty swallowing, severe headaches, seizures, and coma.
Headache

Headaches are very common. There is a wide variation in the type of pain you could experience with a headache and how long it may last. Headaches can be broken into two categories:
- Primary - No clear cause, such as migraines
- Secondary - Have a clear cause, such as headache from an illness
Headache: treatment and advice
Journal post
Did you know it is possible to cause a headache from the overuse of medications taken to get rid of a headache? People who have primary headaches such as migraines or tension headaches are at risk of developing an overuse headache.
For this next activity, you will need to use your internet searching skills to complete the worksheet on primary and secondary headaches. Don’t forget you can use any of your programme resources, including discussion with classmates, to help you.
Get started by downloading the worksheet.
Skim and scan this article from bpacNZ to find out the answers to the following questions.
- Define a medication-overuse headache.
- What are the general clinical observations and symptoms of this type of headache?
(Hint: if you are not sure of some of the language used in this article, do a Google search on the terms.) - How can this type of headache be avoided?
Document your answers in your own words in a journal post and then share it with your tutor and peers.
⚠ When to refer to the pharmacist
When assessing a customer with a headache, you need to be alert to any headache warning signs and indications for referral to the pharmacist.
Warning signs
- The first headache in a person over 50
- Headaches that are brought on by:
- lying down
- cough
- specific activities.
- Headaches described as:
- “The worst headache of my life.”
- New or different to previous headaches
- Severe right from the start
- Develop after a head injury or trauma
- Worsen over time (months).
- Headaches with other symptoms, such as:
- High blood pressure
- Muscle aches
- Weight loss
- Changes in consciousness
- Confusion
- Gait disturbances
- Loss of balance
- Memory loss
- Seizures
- Speech difficulties.
Other signs
- The customer also has a fever, rash, or stiff neck.
- The symptoms have lasted longer than 24 hours.
- The customer is aged less than 12 years old.
- Older people experiencing reoccurring headaches that come from the temples.
- The customer has headaches occurring more than once a month.
- When a customer is attempting to purchase large quantities of analgesics.
- Symptoms have persisted despite treatment with adequate doses of pain relievers.
- The customer is taking medications, including complementary medicines.
- The customer is pregnant or breastfeeding.
- The customer has other health conditions.
- The customer has allergies to medicines.
Period pain
Experiencing painful periods is called Dysmenorrhoea. (‘dys’ from the word bad and ‘menorrhoea’ from the word menstruation).
Dysmenorrhoea is divided into two types:
| Primary | Pain without an underlying problem. It is common and affects more than half of all women at some stage. |
| Secondary | Pain with an underlying cause, such as endometriosis. |
Common signs and symptoms of dysmenorrhoea include:
- lower abdominal cramps that can be mild to severe
- headache and ache in the back extending to the thighs
- nausea and vomiting
- constipation
- diarrhoea
- breast tenderness or pain
- fatigue.
Dysmenorrhoea: treatment and advice
In this week's SDL, we’ll look at the appropriate treatment and advice for this type of pain.
⚠ When to refer to the pharmacist
- When the customer is over 30 and experiencing period pains for the first time.
- Very heavy menstrual bleeding- changing pad or tampon every 1-2 hours.
- If pregnant or postmenopausal and has vaginal bleeding.
- Has an intrauterine device (IUD).
- Pain persists beyond the first two days of period.
- If there is fever and vomiting at the same time.
- NASIDs are not fully effective.
- Pain is described as severe or distressing.
- Abnormal discharge or bleeding between periods.
- Pain unrelated to menstruation or during intercourse.
- Pain is worse with each period.
- the customer is taking medications, including complementary medicines.
- the customer has other health conditions.
- the customer has allergies to medicines.
Self-directed learning activities
Activity 1
Watch: Period Pain | How to Stop Painful Period Pain [...] (10:27 minutes)
- Watch this video clip from Abraham, the pharmacist who discusses the science behind why period pain happens. He then goes on to provide self-care and medication advice to help reduce pain and bloating. He also talks about when a person with period pain should seek help.
Activity 2
- Paracetamol and ibuprofen are over-the-counter medicines that can relieve period pain. You already know quite a bit about these medicines. However, mefenamic acid may be a medicine that you are not familiar with. Using resources such as the NZ Formulary, Medsafe, and other trustworthy sources, find out the following information about mefenamic acid and create a journal post to document your answers:
- Trade names for mefenamic acid
- Is mefenamic acid classified as:
- General sales?
- Pharmacy only?
- Pharmacist only?
- Prescription?
- What type of pain reliever is it:
- Analgesic?
- Antipyretic?
- NSAID?
- What are the possible side effects?
- Save and share your journal post with your tutor.
That wraps up week 7 of study. Ka pai - good work! It's time to complete your Learning Check-in before moving on to Week 8.
