Nau mai hoki mai — welcome back to our exploration on working ethically and professionally as a pharmacy technician.
In this section, we are going to look at working with patients and working with health care professionals in relation to the Pharmacy Council Code of Ethics.
In our last section on this subject, we explored the difference between personal and professional ethics. We noted that while the Pharmacy Council Code of Ethics is primarily intended for pharmacists, pharmacy technicians are also expected to incorporate the principles of the Code into their professional practice.
Go to your Code of Ethics document and answer the following three questions. Download it again if necessary.
Take some time now to read through the Code of Ethics to find out more about each principle. You may like to make your own notes with one or two key points about each principle. This will help you to better understand each of the three core values.
Working with patients

When we apply the Pharmacy Council Code of Ethics to the scope, role, and responsibilities of the pharmacy technician, we can describe the ethical principles that guide how you work with patients as follows:
- Making the health and well-being of the patient your first priority
- Respect the patients' rights
- Carry out your duties with honesty and integrity
- Take responsibility for your own professional behaviour and actions
- Take responsibility and be accountable for your own work
Let's look further at each of these in the following tūmahi (activity). You may like to discuss this with a classmate and share your ideas before submitting your own work.
Working with healthcare professionals
Pharmacy technicians are expected to show professionalism and ethics when interacting with patients and adhere to these standards when working with fellow healthcare professionals. This approach ensures that patients receive the necessary care in a timely manner with the goal of contributing to patient health and well-being.
Go to the Code of Ethics document again, look at Principle 7 on page 14, and then complete this short activity about it.
Once again, by applying the Code of Ethics to your role as a pharmacy technician, we can describe working with pharmacy and other healthcare professionals in an ethical and professional manner.
- Effective communication with health professionals.
- Assisting health professionals to carry out our professional duties.
- Build and maintain good working relationships with health professionals.
- Respect and acknowledge the roles of health professionals.
Self-directed learning activity
Scenario
You are on work placement in a community pharmacy. Talia, the retail assistant in your pharmacy, sees that you are learning about the Code of Ethics. She says, "Isn't ethics and that professional stuff just about being nice to our customers? It's just common sense, really. Why do they need to write it down?"
What do you think? Is working professionally and ethically as a pharmacy technician common sense? Does a professional Code of Ethics need to be a written document?
Write and share your opinion on this with your classmates in the forum. Don't forget to read their opinions too!
Well done, you have completed the Professional Practice Part 1, Week 17. Keep up the great work!
Compliance packaging

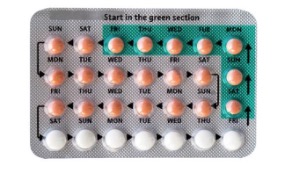
Kia ora, and welcome to this topic, where we look at the advanced dispensing technique of compliance packaging, a method of organising and packaging medications for patient use. See the picture above for an example of one type of compliance packaging.
In your classroom sessions and during your work placements, you'll have the chance to learn about and actively engage in this method of dispensing medications.
Providing medications in compliance packaging is a service offered by many pharmacies to help patients better manage their medication schedules and ensure they consistently take their prescribed medicines as directed. This approach empowers patients to be independent and in control of their health and medication routines. When patients can follow their prescribed medication treatment, their health and well-being are enhanced.
Before we go on, let's take a critical look at the term' compliance'. In the field of healthcare, the term 'compliance' refers to the extent to which patients follow the prescribed treatment plan, medication regimen, or medical advice provided by healthcare professionals.
The term 'compliance' has negative connotations of strict obedience to medication orders and rules imposed on a patient. If a patient does not follow the medicine orders, they are 'non-compliant'. This implies they have failed and are to blame for not following the prescribed treatment plan.
These negative connotations are at odds with the modern healthcare system perspective of patient-centred care, informed consent and partnership between healthcare providers and consumers.
Forum activity
"Compliance"
Perhaps the word 'compliance' needs to be replaced with a word that more accurately reflects a patient-centred perspective? Read this article on the topic.
Now that you have read the article, what do you think? Do we need to stop using the word 'compliance' when referring to treatment plans? What do you think about using the word 'adherence' or 'concordance'? Maybe you have a suggestion for a new word?
Share your thoughts in the class forum.
Non-compliance
There are numerous factors that result in non-compliance with medication treatments. These can be broken into the following:
| Primary non-compliance | Given a prescription but did not get it filled. |
| Secondary non-compliance | Got the prescription filled and started taking the medication but stopped before the full course was completed. |
| Unintentional non-compliance | Not taken as prescribed, either accidentally or due to factors outside of their control. |
| Intentional non-compliance | Consciously not taken as prescribed due to specific factors or concerns. |
Take a moment to reflect and consider what specific circumstances, situations or factors could result in these types of non-compliance. You may have experienced some of these yourself at some point.
Create a list of those factors. Once yours is done, check it against ours below and see what's new to you. Each item on the list is broken down into the factors that may contribute to the circumstances. Expand the labels or select the (+)s to learn more.
Factors contributing to non-compliance of medication treatments
- Lack of awareness: The patient may not be aware of the need for the prescribed medication.
- Financial constraints: Inability to afford the medication
- Transportation issues: Difficulty in accessing the pharmacy to fill the prescription.
- Language barriers: Language differences may hinder understanding of medication instructions.
- Health literacy: Limited health literacy can lead to misunderstandings about the importance of the medication.
- Side effects: Experiencing unpleasant side effects may lead to discontinuation of the medication.
- Improvement in symptoms: Patients may stop taking medication when they feel better, thinking they no longer need it.
- Complex regimens: Difficulty in following complex dosing schedules.
- Medication interactions: Concerns about potential interactions with other medications.
- Cost: Financial constraints may result in intermittent use of the medication.
- Forgetfulness: Patients may forget to take doses as prescribed.
- Complex regimens: Difficulty following complicated dosing instructions.
- Cognitive impairments: Conditions such as dementia can affect a patient's ability to adhere.
- Physical challenges: Physical limitations, like difficulty swallowing pills, can lead to non-compliance.
- Miscommunication: Misunderstanding medication instructions due to language barriers or lack of clear communication with healthcare providers.
- Doubts about medication: Patients may doubt the necessity or effectiveness of the medication.
- Fear of side effects: Concerns about potential side effects
- Personal beliefs: Conflicting personal beliefs, such as religious or cultural views, can influence non-adherence.
- Desire for autonomy: Some patients may want to manage their health without medications, seeking alternative approaches.
- Stigma: Stigmatization of the condition being treated may deter patients from taking their medication.
- Addiction Concerns: Fears of dependency or addiction to medication can result in non-compliance.
Compare and contrast this list with your own list or ideas. Were they similar? Are there any factors that should be on this list but aren't?
Non-compliance with medications can be a complex situation, influenced by factors like the patient's individual situation, healthcare systems, and the nature of the medicines themselves. To tackle this effectively, healthcare providers need to understand these factors and create plans to help patients make informed choices about their prescribed medicines. They also play a crucial role in helping patients overcome any barriers that might get in the way of taking their medicines as directed. One practical solution in this effort is using compliance packaging to make medication management more accessible.
Types of compliance packaging
Various types of compliance packaging are available to assist with medication adherence. One type is pre-packaged medicines by the manufacturer. Let's take the example of the oral contraceptive pill (OCP).
The oral contraceptive pill
Packaging typically includes the following features:
- Multiple sheets of blister packs: These are individual sheets made of foil with blisters placed inside a box.
- Single daily dose in each blister: Each blister in the sheet contains one daily dose of the pill.
- Day labelling: Each dose is clearly labelled with a day of the week, making it easy to follow the regimen.
- Directional arrows and coloured sections: Some packaging includes directional arrows and coloured sections on the foil. These markings indicate where and when to start taking the pill and where to find the next daily dose.
- Organised for one menstrual cycle: Each sheet of the blister pack is organised to represent one menstrual cycle. Depending on the specific type of OCP, it may contain a combination of active pills and placebo (sugar) pills. Active pills are taken daily to provide contraception and other non-contraception benefits, while placebo pills are included to mimic a natural menstrual cycle. Typically, placebo pills are taken during the time when a person would normally have their period and may be different in colour and size to the active pills.
- Alternatives: Some OCPs contain only active pills. During the menstrual period, no pills are taken for a specific duration, usually seven days, after which the active pills are resumed.
These packaging details can vary depending on the type of OCP being used. Understanding these features is essential for both healthcare providers and patients to ensure the correct administration of oral contraceptives.
 |
 |
Think about the features mentioned above. What are the advantages or benefits of this type of compliance packaging? Challenge yourself to create your own list before clicking on the labels or (+)s to see the answers.
- Convenience: Compliance packaging simplifies the process of taking the OCP by providing clearly labelled daily doses. Patients don't need to manually sort their pills each day. Simplifies medication management, particularly for patients who are juggling multiple medications.
- Travel convenience: Compliance packaging makes it easier to pack and manage medications when away from home.
- Reduced risk of missing doses: The day labelling ensures patients take the correct pill on the right day, reducing the risk of missed doses and improving adherence.
- Ease of use: Directional arrows and coloured sections guide patients on when and where to start taking the pill and where to find the next dose, making it easier to follow the regimen.
- Organisation: Each sheet represents one menstrual cycle, helping patients stay organised and ensuring they don't miss any active pills.
- Mimicking natural cycle: Packaging includes placebo pills that mimic a natural menstrual cycle. This helps in maintaining a routine and provides a familiar pattern.
- Reduced confusion: Patients can easily distinguish between active and placebo pills, reducing the chances of errors in pill-taking.
- Consistency: Compliance packaging promotes consistent pill-taking behaviour, which is crucial for medication effectiveness.
- Improved adherence: With clear labelling and organisation, patients are more likely to adhere to their medication regimen.
- Reduced waste: Individual blister packs reduce the likelihood of accidentally dropping or losing pills, minimizing waste.
- Greater confidence: Patients can have confidence that they are taking the correct pills at the right time, reducing anxiety and uncertainty.
Now that we have looked at the features and benefits let's think about the disadvantages or limitations. Consider what these may be before clicking on the (+) to reveal some suggestions.
- Disruption of routine: If the packaging does not contain the sugar pills, then the daily routine is disrupted, and there is a potential to forget to restart the active pills on time.
- Complexity: The presence of placebo pills and different sections on the packaging can be confusing for some patients, potentially leading to errors in pill-taking.
- Visual impairments: Patients with visual impairments may have difficulty reading the packaging labels and following the day-specific dosing.
- Inconvenience: People taking multiple medications may prefer their OCP to be packaged with their other medicines, not in separate packaging.
- Costs: Increased manufacturing costs to produce this type of packaging.
- Environmental impact: This type of packaging generates more waste and is less environmentally sustainable compared to pills dispensed in a single container.
In our next session on this topic, we will look at other types of compliance/adherence packaging that you will be involved with as a pharmacy technician.
Self-directed learning activity
In today's self-directed learning (SDL) activity, we'll be applying the reading skills of skimming and scanning.
If you're not familiar with these reading techniques, here's a brief explanation:
Skimming and scanning involve reading specific parts of a text to find key information quickly. In this activity, we'll be using these skills to explore a research article on compliance packaging. Your objective is to efficiently extract valuable insights from the article to support the learning from this session. To help you skim and scan, you will notice that some key points have been highlighted for you. As you read, you may want to add to your own notes from this session.
Me tīmata tātou — let's get started! Read the article now before moving on to Introduction to Patient Care.

Talofa and welcome to the next session in your Introduction to Patient Care course. You've been putting in a lot of effort to gain the knowledge and skills necessary to be a great pharmacy technician. You should be very proud of your efforts. Kātahi te tangata pukumahi ko koe! You are a hard worker!
Everything you've learned and practiced so far has been aimed at preparing you to be able to achieve the following:
- Provide advice and guidance on the use of dispensed medicines.
- Advise patients on routes of administration for dispensed medicines.
- Advise patients on dose forms for dispensed medicines.
- Advise patients on the use of accessories for dispensed medicines.
- Apply knowledge of medicines as they relate to the treatment of a range of common health disorders.
- Assess the health of pharmacy clients to determine common health disorder treatment requirements.
- Advise pharmacy clients on medicines to treat common health disorders.

In the upcoming weeks, we'll revisit your learning, delving deeper and expanding on what you already know. This is your opportunity to reflect, identify any knowledge gaps, and take a more active role in shaping your learning journey as you prepare to become a qualified pharmacy technician.
We encourage you to take advantage of the resources available to you to seek information and expand your learning. Remember, people are valuable resources, too. Engage in conversations (kōrero) with your tutor, classmates, and pharmacy colleagues to enhance and support your learning journey.
A whakataukī (proverb) to help inspire you to keep learning:
Ko te manu e kai ana i te miro, nōna te ngahere,
Engari, ko te manu e kai ana i te mātauranga, nōna te ao
The bird that consumes the miro berry owns the forest,
The bird that consumes learning owns the world.
Pharmacology
Time to recap what you know about pharmacology by answering the following five multichoice quiz questions.
Tino pai — very good. Hopefully, you got most of those right. If not, don't worry. Studying the solutions will help confirm your understanding.
Pharmacokinetics
To help you remember some other important pharmacology concepts from this course and prepare for more detailed ones later, we have an article for you to read. Some of the information in the article would already be familiar to you. Answer the eight questions below to help consolidate your knowledge before using the following Document activity to reflect on and record your answers.
Click here to access the article on pharmacokinetics.
And now, put together your resource with this Document Tool activity.
Pharmacodynamics
As noted in the quiz at the beginning of this lesson, pharmacodynamics is about how quickly a medicine starts to have an effect on the body, for how long and how intensely. In essence, it is how a drug affects our bodies.
To expand on this idea, we can say that pharmacodynamics explores how drugs affect the behaviour of cells in our body. It focuses on how medications can change how a cell functions or alter its rate of operation. Understanding pharmacodynamics is about comprehending how drugs influence the activities of our body's cells and how these interactions lead to desired therapeutic effects. Stay tuned for this in course 8.
Forum Post
Consider what we've covered in pharmacology so far in this programme.
Do you believe it's important for pharmacy technicians to understand pharmacokinetics and pharmacodynamics?
Write a brief paragraph explaining your opinion and share it on the class forum.
Routes of administration
Time for another recap quiz! Answer these five questions to recap your knowledge of routes of administration.
Systemic circulation is a term you have come across when exploring how medicines move through the body. In the next activity, you get to check your understanding of the term.

Scenario
During your work placement at a community pharmacy, a customer approaches you with a question about their medication. They mention coming across the term 'systemic circulation' and ask you to explain what this means. You have learnt about this in your introduction to pharmacology, so feel confident you can provide a simple and easily understandable explanation for this patient.
Come up with your explanation before clicking on the label or (+) to reveal our suggested explanation.
Systemic circulation is like the body's transportation system for blood. It's the movement of blood from the heart through the blood vessels of the body. As the blood moves around the body, it delivers oxygen and nutrients to all the cells, tissues, and organs and removes waste products like carbon dioxide.
Do you think this is a good explanation? How does it compare to what you would say?
We've just provided a lot of information. Let's consolidate your learning with this two-question knowledge check.
Journal post
Bioavailability
Bioavailability is another term you have looked at previously. Write a brief explanation of what this word means in your journal and publish your work.

As you will recall, the bioavailability of a medication is influenced by the route of administration. This is because each route has different levels of absorption and metabolism. High bioavailability means that a large portion of the administered drug is absorbed into the systemic circulation to become available for its intended therapeutic action. On the other hand, low bioavailability means that only a small portion of the administered drug is absorbed into the systemic circulation.
Considering what you already know, answer these two questions:
Journal post
What factors will a prescriber consider when determining the most suitable route for a specific patient's prescription?
Record your answers in your journal and publish your work.
Kei runga noa atu! Outstanding job on your dedication to revising and reinforcing your pharmacology knowledge. By successfully completing this learning session, you've not only strengthened your foundation but also set a strong course for the upcoming phases of your program. Keep up the fantastic work!
Self-directed learning activity
Read this summary guide of the most common routes used to administer drugs, the advantages and disadvantages of each drug route, and examples of dosage forms that are used to deliver the active drug to the intended site of action in the body.
To get the most out of this learning activity, create your own notes to add to the resources you have already gathered on this topic.
Tino pai! That’s week 17 done and dusted.
