When your clients hire you, they trust that the programme you design, will not hurt them. They expect a safe training program. Knowledge of the skeletal system is critical to creating an injury-free fitness plan.
A sound understanding of the skeletal system and joints helps you recognise structure and movement issues. It makes it easier to identify where an issue may arise and how to correct it.
In this topic, you will learn:
- The overview of the skeleton
- Types of bones
- Bone functions
- Bone development
- The spine
- Bone mineral density
- Poor bone health
- Joint anatomy and terminology
- Synovial joints
- Other joint types
- The Spine
- Joint conditions
- Exercise and Joints.
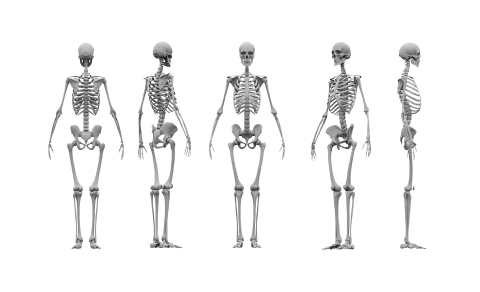
The images below show the skeleton from different perspectives. In this topic, we look at bones, what they do, how they grow, and how they all fit together to make up the skeleton (in other words, their 'structure and function').
These are the main bones you should know the locations of. Study these carefully. If you are keeping a personalised vocabulary reference guide, add these bone names to it. You may also wish to create flashcards to practice your recall.
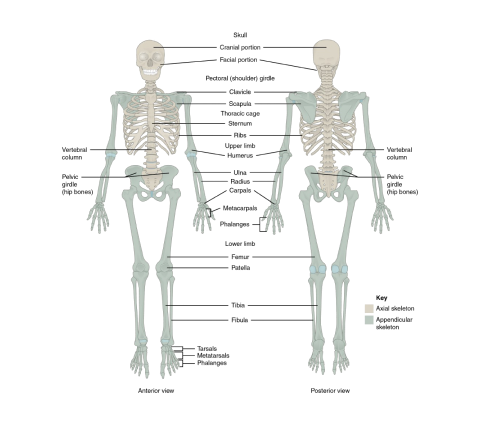
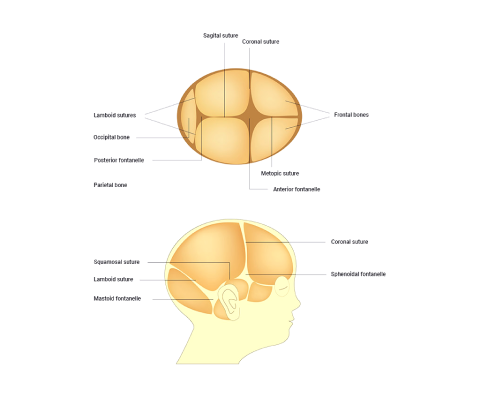
The adult human skeleton is comprised of 206 named bones. Most of these are paired, that is, they have a 'friend' on the other side of the body. What’s on the left is typically on the right also. The skeletons of infants and children have more bones than the adult human skeleton. This is because, as our skeletons develop, our bones fuse together (e.g., bones of the skull) and therefore, the total number of bones decreases.
Bones are anatomically grouped into two different divisions. This enables speedy identification and provides an idea of their role in the skeleton.
Divisions of the skeleton:
- Axial skeleton
- Appendicular skeleton
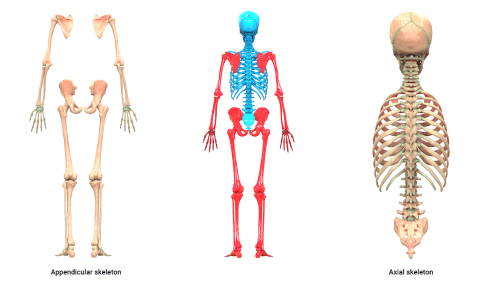
Axial skeleton
The axial skeleton is represented in blue in the preceding image. Eighty (80) bones exist within the axial skeleton. The term axial implies axis. So you can figure out that structures down the body's midline (the spine is our imaginary midline) form the axial skeleton.
- Skull
- Face
- Auditory bones (ossicles)
- Vertebral column
- Sternum and ribs
Appendicular skeleton
The appendicular skeleton is represented in red in the preceding image. These bones include everything that 'hangs off' the axial skeleton - the appendages. The appendicular skeleton consists of 126 bones. This includes the bones of the:
- Arms and legs
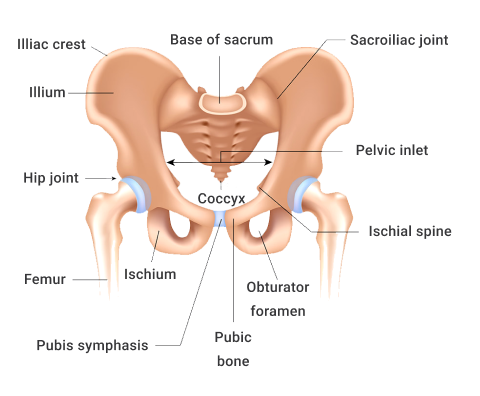
- Pelvis
- Hands and feet
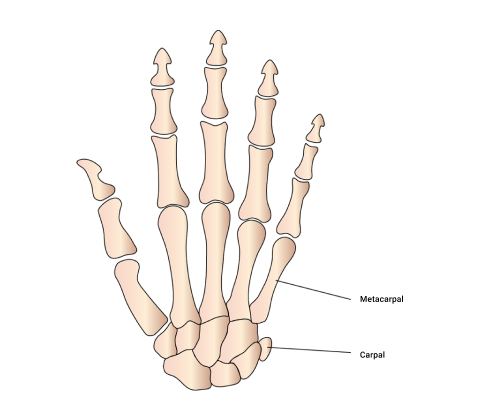
Can you name all the bones in the image below? Additional research may be needed.
Bones come in different shapes and sizes. The shape and size depend on the role of the bone.
There are 5 different shapes of bone.
- Flat
- Long
- Short
- Irregular
- Sesamoid
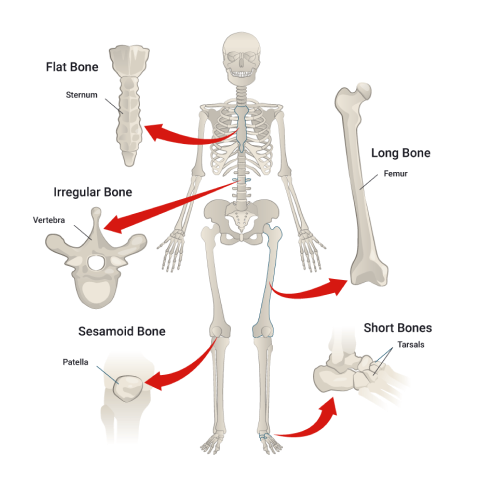
The structure once again mirrors function. The shape of the bone provides a clue to the function of the bone. Let's take a closer look at bone shapes, structure, and function.
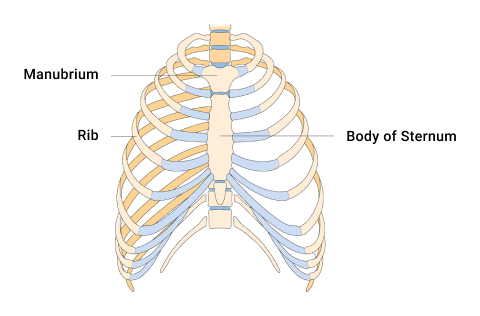
Flat bones
Flat bones offer protection and many sites for ligament and tendon attachment. They provide coverage of large areas. Examples include:
- Cranium
- Ribs
- Sternum
- Scapula
- Pelvis
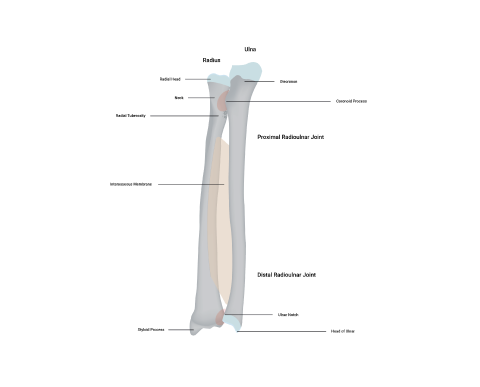
Long bones
A long bone is typically longer than it is wide. Long bones can act as levers for muscles to act on. Examples include:
- Humerus
- Radius
- Ulna
- Femur
- Tibia
- Fibula
- Metacarpals and metatarsals
- Phalanges.
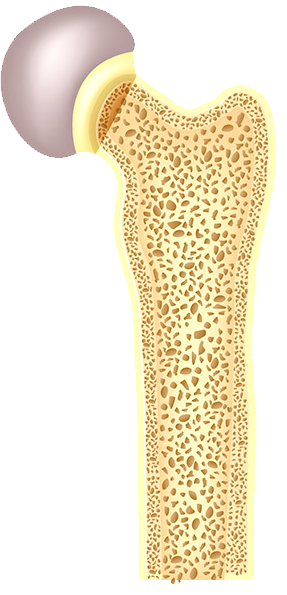
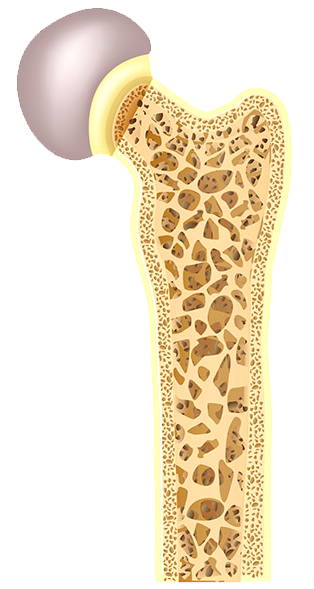
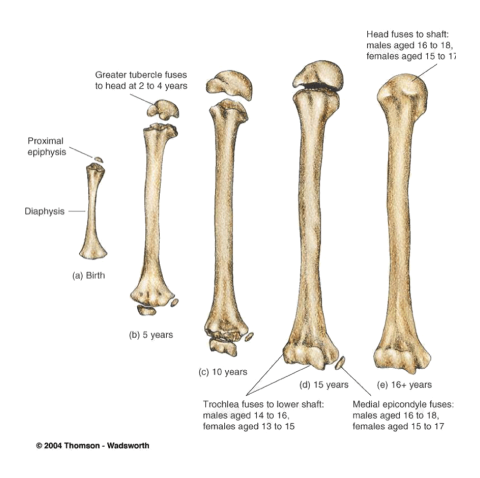
A typical long bone consists of the regions shown in the following diagram. To fully understand both the skeletal system and also its relationship with exercise, you must familiarise yourself with these regions and their components.
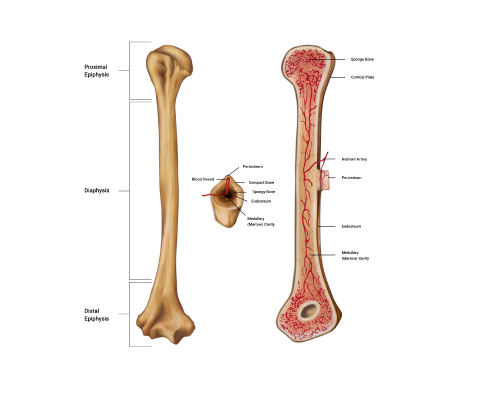
Regions of a long bone explained
The 3 main regions of a long bone are the proximal and distal epiphyses, the diaphysis, and the medullary cavity.
- The epiphyses (e-pif-i-seez): These are found at both the proximal and distal ends of a long bone and named accordingly. The singular is epiphysis. The regions are typically the widest regions of a long bone and are filled with spongy bone (houses red bone marrow) and covered with a shell of compact bone.
- The diaphysis (di- af-y-sis): Known as the 'bone shaft' or 'body', this is the middle section of a long bone. The diaphysis is long, cylindrical, and hollow. The diaphysis connects with both the proximal and distal epiphyses.
- The hollow region of the diaphysis is known as the medullary cavity. This is where we find yellow bone marrow and many blood vessels (in adult bones). The hollow design of a long bone enables great strength to be achieved whilst maintaining a long yet lightweight bone which is much easier for our muscles to help move than a heavy, dense structure.
Short bones
These are equal in length and width. They cannot move much but can move in most directions a little. They provide stability and can facilitate some movements. Examples include:
- Carpals (wrist)
- Tarsals (feet)
- Talus (where the tibia meets the foot)
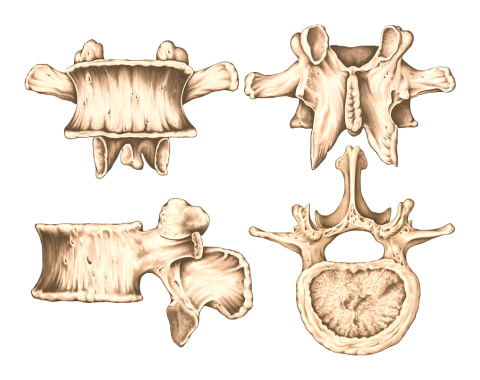
Irregular bones
These vary in shape and don't fit into any other category. They often have a complex shape which aids their role in protecting internal organs. Examples include:
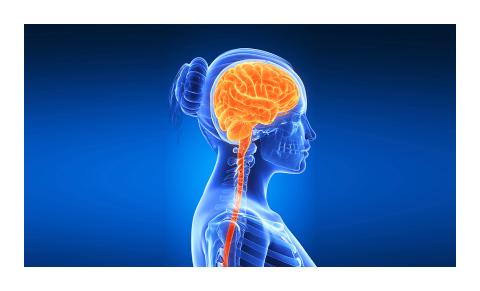
- Vertebrae of the spine (protecting the spinal cord)
- Pelvic bones (ileum, ischium, and pubic, which protect our pelvic organs)
Sesamoid bones
Derived from the Latin sesamum meaning 'sesame seed' due to its typically small size. These bones are often embedded within a muscle or a tendon. They relieve tension within muscles and tendons, allowing for increased weight-bearing and tolerance by redistributing forces throughout a muscle or tendon. In doing so, the sesamoid bones protect the muscles and tendons from significant strain and injury. Examples include:
- In the patella (knee cap) - this is the most common sesamoid bone
- Others can be found in the hand and the foot
Watch
Enjoy the following video, which gives a colourful and simple summary of bone shapes, examples of their location, and the functions of each.
The skeletal system is responsible for 6 main functions.
- Support
- Protection
- Movement (assistance in movement)
- Blood cell production
- Mineral storage and release
- Storage (adipose/fat storage)
You need to be familiar with these functions as this will support you in achieving a more complete understanding of the human body and medical conditions that affect the skeletal system. The skeletal system and its functions impact how you will design programmes.
Support
The skeleton provides a structural framework, like scaffolding, which provides a structure for our body. Without the skeleton, we would essentially be a 'blob'. It also provides an attachment site for muscles, ligaments, and tendons.
For example, the vertebrae supports the torso and head.
Protection
Bone is the hardest substance in your body. It is used in many places to protect the vulnerable organs underneath from outside forces. Examples include the ribs protecting the vital internal organs such as the heart and lungs, and the cranium protecting the brain. Remember, structure mirrors function. There is a reason we are built the way we are!
Movement (assistance in movement)
Bones provide attachment points for ligaments and tendons. Muscles are attached to bones via tendons. The bones act as rigid levers for movement to occur. This movement is articulated by joints. When a muscle contracts, it shortens and pulls on the bone it is attached to. As a result, movement occurs.
What are some everyday movements your body performs? Which bones make this movement possible?
Blood cell production
The soft, spongy material in the middle of bones is called bone marrow. It produces approximately 95% of the body's blood cells.
Both red and white blood cells are formed in the bone marrow. Red blood cells (erythrocytes) carry oxygen from the lungs to the rest of the body. White blood cells fight infections and help the immune system. Platelets are another type of blood cell that is formed in the bone marrow and helps to control bleeding (John Hopkins Medicine, n.d.).
The following picture shows the many blood components produced in the bone marrow.
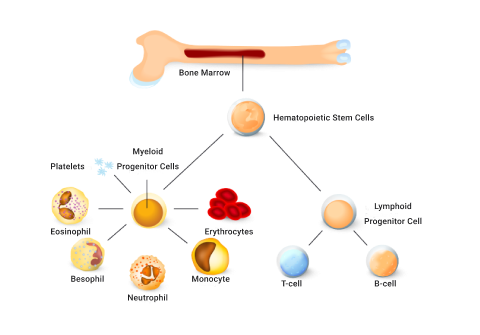
In children, blood cells are created in long bones like the femur. In adults, blood cells are mostly formed in the spine (vertebrae), hips, ribs, skull, and sternum.
Mineral storage and release
Bone is the body’s main storage of calcium. It stores around 99% of the body’s calcium and releases it when needed. Calcium is hugely important for bone growth and development and many other functions in the human body, such as muscle contraction.
Bones also store iron, potassium, and phosphorus and release them into the blood when the body needs to use them.
The pelvis, sternum, vertebrae, and clavicle are all important bones for mineral storage and release.
Storage (adipose/fat storage)
Fat tissue is also stored within the bone in the bone marrow. Bone marrow is primarily located in the ribs, vertebrae, sternum, and pelvic bones. This is additional energy storage and can be released when required to maintain physiological processes.
Watch
The following video provides a good overview of the major functions of bones.
Welcome to your very first system of the human body, the skeletal system!
Bone anatomy
Bone is composed of several types of tissues working together. These are bone, cartilage, adipose, connective tissue, and nervous tissue. This is why each bone in your body is technically considered an organ.
Development
Bone is classified as a dynamic living tissue as it continues to perform a process called 'remodelling', which is the process of new bone-forming and the breaking down of old bone.
Bones determine your body's dimensions - your size and proportion. Our bones begin to form after just six weeks as a foetus and continue to grow until a person is approximately 25 years of age.
Research suggests peak bone mass may be considerably lower for females. Scientists think it is now important for young women to endeavour to build 'bone banks' while young to lay down as much bone as possible before they turn 20 years old. To do this, we must ensure adequate calcium in our diet and perform regular loaded exercise.
Watch
This video explains how bones grow naturally inside the body and considers how bones might be grown outside the body in the future. Watch the video and complete the summary.
The term 'bone mineral density' refers to the amount of bone mineral (mainly calcium) present in a bone. Bones with high mineral density are stronger, can withstand greater forces, and are less likely to fracture. Bones with low mineral density are weaker and more prone to fracture under stress.
Normal bone
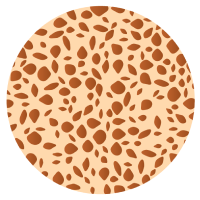
Osteopenia
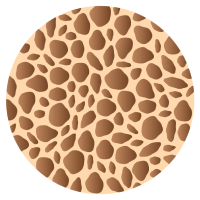
Osteoporosis
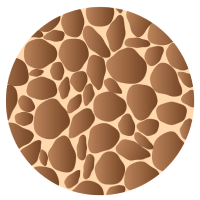
Severe Osteoporosis
Factors contributing to bone density
3 factors are critical in developing bone mineral density:
- Sex hormones: Testosterone and estrogen hormones (among others) stimulate bone deposits.
- Nutrition: Adequate food intake, including regular consumption of calcium.
- Loaded exercise: This refers to exercise that places repetitive stress on bones to encourage bones to adapt (strengthen).
How to enhance bone mineral density
We want to use exercise to improve bone strength via increasing bone mineral density.

Research has clearly shown a direct relationship between exercise and bone health. But not all exercise affects bone the same when it comes to building strong, healthy bones or preventing poor bone health, such as osteoporosis.
Loaded exercise is the key to maintaining bone mineral density and bone health.
Loaded exercise
The term 'loaded' refers to an activity that places at least body weight on bones, such as running, dancing, low-impact aerobics, or skipping. These are weight-bearing aerobic activities on your feet, where bones are supporting your weight.
When placed under mechanical stress, bone tissue becomes stronger. This is due to an increased rate of bone production, which occurs quicker than the bone reabsorption (breakdown) phase of the bone remodelling process. Activities such as jumping and running stimulate the process of bone remodelling more effectively and efficiently than activities such as low-weight-bearing activities (e.g., cycling and water-based activities) because these do not elicit the same response in terms of bone density.
To stimulate bone growth, the exercise must create stress on the bone.
People who do regular loaded physical activity produce denser and more mineralised bones when compared with sedentary individuals.
Occupations and sports that are predominantly one-arm dominant (e.g., tennis players, baseball pitchers, or cricket bowlers) result in more mineralised bones on the dominant side.
Resistance exercises can also strengthen bones, e.g. weightlifting, free weights, body weight, and exercises with resistance bands.
It is also important to include exercises for stability and balance. Improved stability and balance will help prevent falls, and help muscles work together to keep the body stable.
Nutrition
The other key factor in bone health is nutrition. You must provide your body with enough essential minerals to support bone growth and maintenance.
Watch
Dr Jen Gunter explains what you can do for strong, healthy bones in this short video.
Factors to consider when selecting exercises for bone mineral density
3 characteristics of exercises that have the largest impact on increased bone density are:
- Strain magnitude
- Strain rate
- Strain frequency
Strain magnitude
The amount of stress placed on the bones.
This is higher in exercises such as gymnastics and weightlifting, where the force or impact of the exercise is greatest.
Strain rate
This is the velocity over which the strain is placed on the bones.
This is higher in exercises such as jumping or plyometrics, where the rate at which the impact is felt is high.
Strain frequency
This is how often strain is placed on bones during the course of an activity.
This is higher in exercises such as running, where the impact on the bones frequently occurs during the exercise session.
Order of importance
Strain magnitude is the most important of the three factors for bone density. Velocity is the next most important factor, followed by frequency.
- Strain magnitude
- Strain rate (velocity)
- Strain frequency
Cross-training
Athletes involved in sports that have low strain magnitude (such as water-based sports and cycling) would benefit from a form of cross-training that is higher in strain magnitude. E.g., a water polo player may benefit from doing some weight training to ensure their bone density is maintained.
Cross-training is a form of training that typically incorporates multiple training systems through various exercises to develop and enhance overall performance.
It is important to have the correct balance of these when designing training programmes. Consider a thorough pre-screening session when working with new and existing clients.
It’s important in developing a safe and effective exercise programme design, to take the time to sit down with your client, take them through a pre-screening questionnaire and consider providing an example. Break the ice with the client to gain a thorough (but not intrusive) medical history to ensure you are aware of any potential risks you can avoid, by selecting the correct exercise and exercise frequency. This comes under the mindset of programme design and pre-screening. We'll look at this in greater detail in future modules.
Poor Bone Health
If only little stress is placed on bones, bones will demineralise.
Use it or lose it!
Bone demineralisation can happen for a variety of reasons:
- Sedentary lifestyle
- Low-impact endurance exercise
- Becoming bedridden
Nutritional deficiency can also contribute.
Normal bone
Osteopenia
Bone wasting conditions
Bone growth is dependent on sex hormones. As the levels of these hormones reduce with age, bone mineralisation decreases, and bone atrophy (wasting) can start to occur.
All of us will eventually suffer from osteopenia which is a natural de-mineralisation of bones as we get older.
If this gets to the point where daily living is compromised, it is known as osteoporosis.
Osteoporosis is a disease where new bone generation does not keep up with old bone removal. The bones become weak and brittle and more at risk of breaking. Risk factors for developing osteoporosis include:
- being over the age of 50.
- being physically inactive.
- having low levels of micronutrients such as calcium and vitamin D.

Introduction
Joints or 'articulations' are formed at the point where two bones meet. They are the connection between bones in the body and link the skeletal system as a functional whole system. Without joints, our skeleton would be a rigid deck structure unable to move. Have you ever been unfortunate enough to have a limb in a cast? If so, you know how this limited functional movement.
Joints and connective tissue hold the bones of our skeletal system together while still allowing some degree of movement.
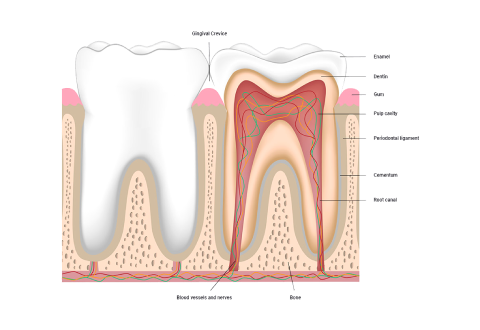
A joint is a point of contact:
- between two bones.
- between bone and cartilage.
- between bone and teeth.
Joints have 2 main functions:
- Hold the skeleton together
- Give the skeleton mobility
In this topic, we focus on the names, structure, function and classification of joints within the skeletal system. You will learn:
- The science behind names
- Joint types and classifications
- Synovial joints
- Cartilaginous joints
- Fibrous joints
- Common joint conditions
- Exercise and joint considerations
The Science Behind Names
In anatomy and physiology, you will read terms in both Latin and Greek as well as English. This can feel overwhelming. But, if we break down words into smaller parts, they become more familiar.
Typically, the scientific joint names are derived from the names of the bones involved. So looking at the names help us gather information about the structure, function, and location of the joint.
With practice, you will soon be able to easily 'translate' these names. This will support your understanding of anatomy and physiology. When this knowledge is combined with knowledge of muscle tissue, structure, and function, you will have a solid understanding of:
- where muscles and bones are located in the human body.
- which muscles are in a specific area.
- what bones are involved.
- which joints are present.
- how these all work together to provide particular movements.
Translating joint names
The scientific joint names are derived from the names of the bones involved. Let's break down "sternoclavicular joint".
- "sterno" = the sternum
- "clavicular" = the clavicle
So the sternoclavicular joint is where the clavicle meets the sternum. In the image, you can see this also applies to the acromioclavicular joint. It is located between the acromion and the clavicle.
- Sternoclavicular joint
- Clavicle
- Acromiaclavicular joint
- Acromion
- Concaid process
- Sternum
- Scapula
- Humerus
- Supraspinatus m.
- Subscapularis m.
- Infraspinatus m.
- Teres minor m.
Can you figure out which bones are involved in the following joints? Expand the accordion to check.
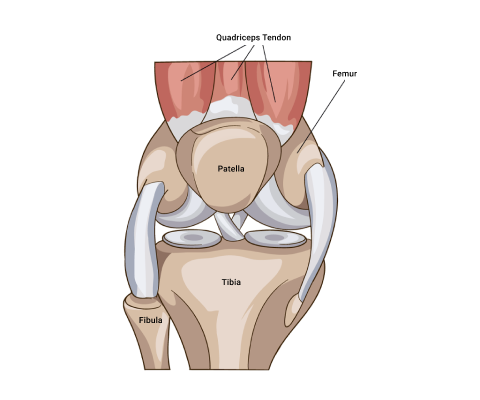
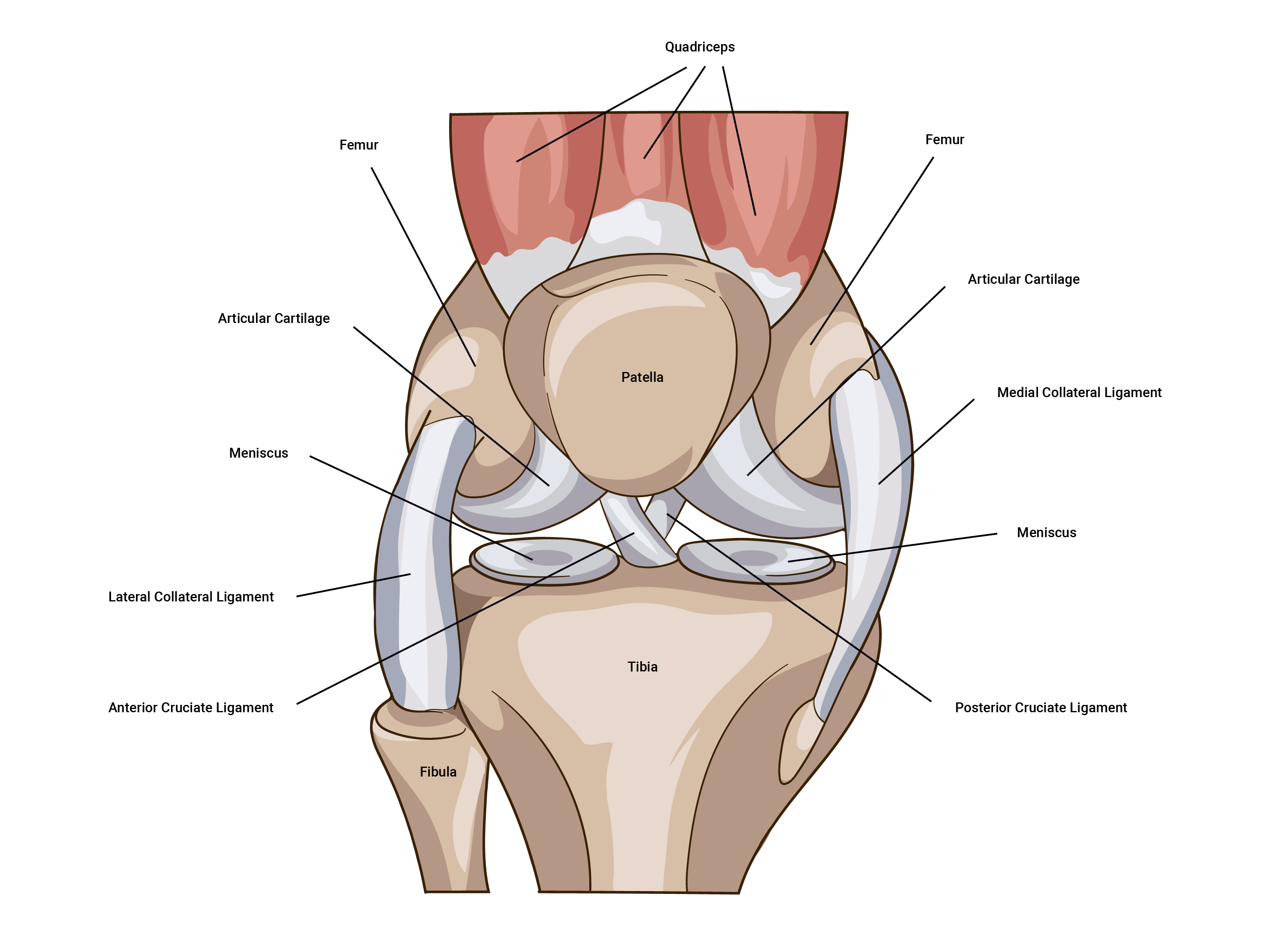
The tibiofemoral joint is where the femur meets the tibia. In this situation, the joint (synovial) is made complete by the patella (knee cap). Note, the patella completes the knee structure and is not classified as a component of a synovial joint.
The glenohumeral joint is where the humerus meets the glenoid cavity of the shoulder.
Of course, there are more common names for the key joints of the body.
- Hip joint: Iliofemoral joint (involving the ileum and the femur)
- Knuckle join: Metacarpophalangeal (involving the metacarpal bones and the phalangeal bones)
- Elbow joint: Humeroulnar joint (involving the humerus and the ulna)
- Ankle joint: Talocrural joint (involving the tibia, fibula and the talus (heel bone))
Sometimes it pays to be specific. As you've now seen, there are multiple joints that we could call a 'shoulder joint'. The language you use with clients, colleagues, and other health professionals will differ.
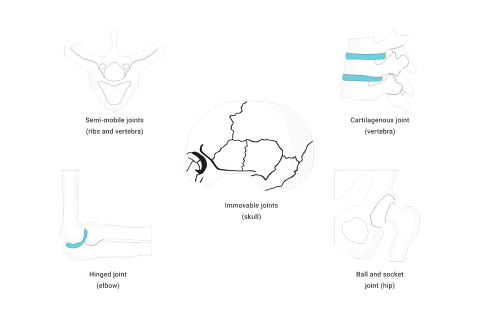
Joint Types and Classifications
The skeletal system contains different classifications of joints based on structural composition and function (degree of movement).
Structural classification
The structural classification of joints is based on the dominant type of connective tissue.
- Synovial joints
- Cartilaginous joints
- Fibrous joints
Functional classification
The functional classification is based on the amount of movement permitted.
- Diarthrosis (freely moveable)
- Amphiarthrosis (slightly moveable)
- Synarthrosis (immovable)
How do structural and functional classifications relate?
The two classification schemes correlate.
Synovial joints are diarthrosis
They move freely. These can be further broken down into 6 groups based on how they move:
- Ball and socket joint
- Hinge joint
- Pivot joint
- Gliding (plane) joint
- Saddle joint
- Condyloid (ellipsoidal) joint

As a personal trainer, synovial joints are the joints you should become most familiar with. The risk of injury is generally greater at these joints due to the greater range of movement and subsequent reduction of the strength of the joint. These are the joints where movement happens, so knowledge of these joints and how they move is essential to exercise prescription. Synovial joints are where we will focus the most when studying joints for personal training.
Cartilaginous joints are amphiarthrosis
They are slightly moveable. Movement is needed but only to a certain degree. An example of this type of joint would be intervertebral discs in the vertebral column, where individual vertebrae are separated by cartilage, allowing some slight movement.
Fibrous joints are synarthrosis
They do not move. These joints are held together by tough tissue (specifically fibrous connective tissue), which develops during childhood. The cranium is an example of a fibrous joint (Physiopedia, n.d.).
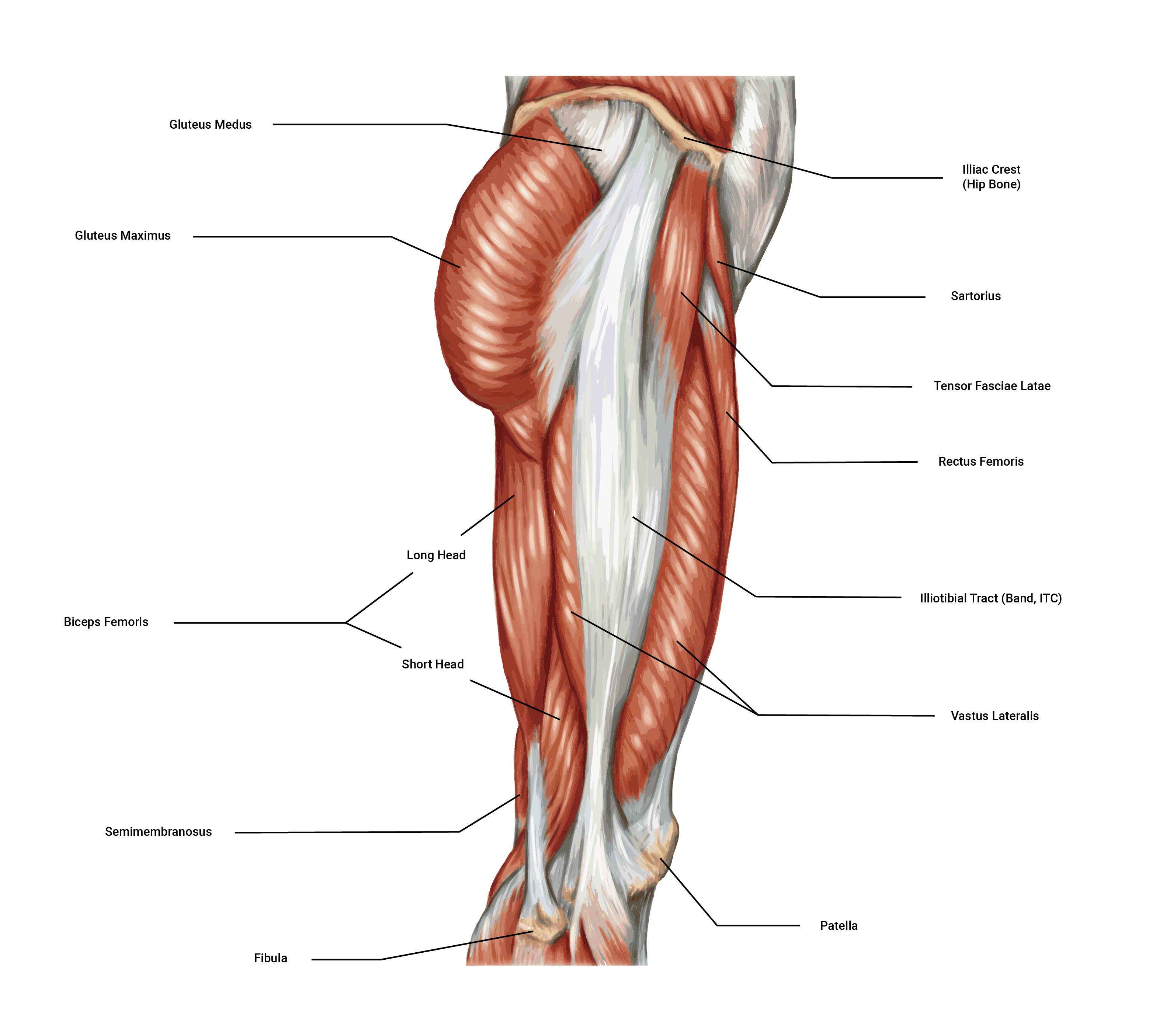
Compare the images in the following slider. Look at:
- The knee joint in the first image
- The vertebral column or spine in the second image
- The cranium in the third image
Do the movements yourself. Are the joints moving freely, moving slightly, or immovable?
The primary purpose of synovial joints is to prevent friction where two or more bones meet. All synovial joints are diarthrosis joints, but the extent of movement varies and is often limited by the connecting ligaments. Nearly all joints of the limbs and most joints of the body are synovial joints (Physiopedia, n.d.).
Structure
A synovial joint has a synovial cavity between the bones. This cavity is filled with synovial fluid. The synovial fluid:
- allows smooth, frictionless movement.
- provides nutrients.
- removes wastes.
The synovial fluid acts as a lubricant, like oil in an engine, allowing all parts of the joint to move against each other smoothly. A synovial cavity allows significant movement of the joint.
Synovial joints also contain hyaline cartilage, known as articular cartilage. Articular cartilage provides shock absorption and reduces friction.
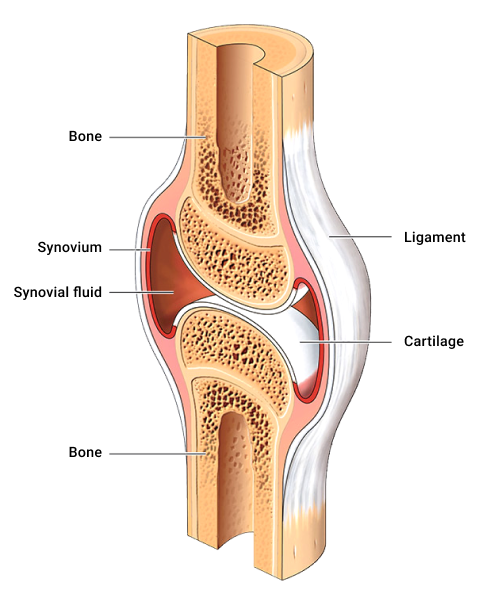
Typical structural components of synovial joints
Synovial fluid is produced by the synovial membrane and housed within the cavity. Synovial fluid is a semi-thick, clear/pale yellow fluid (which resembles the consistency and appearance of an uncooked egg white). This fluid forms a thin covering over the surface of the articular capsule.
The articular cartilage lines the ends of the bones but does not join them.
A fibrous joint capsule surrounds the joint to join the two articulating bones and enclose the synovial cavity.
The synovial membrane (synovium) secretes synovial fluid.
Accessory ligaments are present in the region of the synovial joint, e.g., the medial and lateral ligaments of the knee. They are not part of the synovial joint directly, but they support the joint.
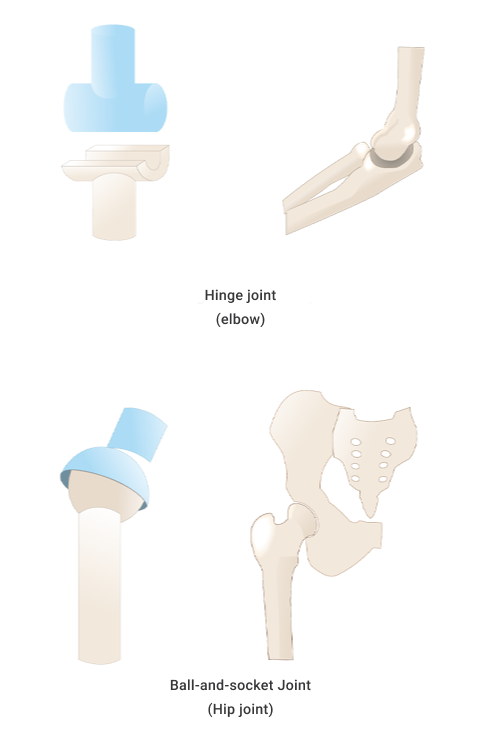
Types of synovial joints
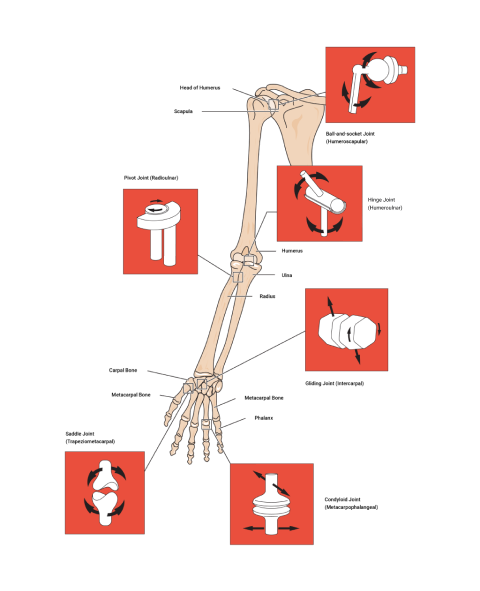
| Type of joint | How it moves | Example(s) |
|---|---|---|
| Ball and socket | Ball and sockets are due to the end of one bone having a 'ball' like end and the other bone having a 'socket' that the ball sits in. They move in multiple planes; for example, to flex, extend, rotate, abduct, adduct, and in circumduction. | Shoulder and hip |
| Hinge | A hinge moves in one plane only, like a door hinge. | Elbow and knee |
| Pivot | A pivot is a pure 'rotating' joint. | Neck, between C1 and C2 |
| Saddle | A saddle is when the end of one bone is like a concave 'saddle' that the other bone sits over, like two legs on a riding saddle. It allows a substantial range of movements. | Fingers and thumbs |
| Gliding (plane) | Gliding occurs when short bones glide along each other in all directions (but not far). Think of it like sliding two coins together between your fingers. | Intercarpal |
| Condyloid (ellipsoidal) | Condyloid refers to shallow ball and socket joints that can do everything a ball and socket joint can do except rotate. | Wrist |
Name that joint!
Practice labelling the joints to get familiar with the names. Use the exact spelling as the list provided in the activity. For example, "Ball-and-socket" contain hyphens.
Movements
The movements provided by synovial joints include:
- Flexion and extension
- Abduction and adduction
- Circumduction
- Rotation
- Supination and pronation
- Lateral flexion
- Elevation and depression
- Protraction and retraction
- Ankle dorsiflexion and plantar flexion
Review Movement Terms in Anatomical Terminology if you need a refresher.
Move your synovial joints corresponding to those circled in the image. Identify the type of joint and the movement(s) for each joint.
Based on your knowledge of movement terms and how the different synovial joints move, can you match the movements to the joint type?
Cartilaginous Joints
Cartilaginous joints contain no synovial cavity. The articulating bones are joined by cartilage (hyaline or fibrocartilage). They provide more movement than fibrous joints but less than synovial joints. The joints between the ribs and the sternum (breast bone) are examples of cartilaginous joints. They are represented in blue in the following image.
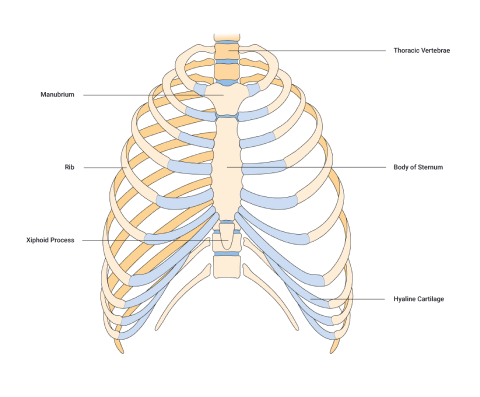
Structure
Cartilaginous joints occur where the bones are bound by cartilage (either hyaline or fibrocartilage) which permits little to no movement. Cartilaginous joints lack a synovial cavity.
Two types of cartilage can join bones via a cartilaginous joint:
Softer and with more give. Glassy appearance, often with a bluish hue. Think of the gristle on the end of a chicken drumstick bone.
Tougher, denser, more rigid cartilage.
Structurally, there are two types of cartilaginous joints:
- Synchondroses (primary cartilaginous joints)
- Sympheses (secondary cartilaginous joints)
Symphyses
Symphyses (the plural of symphysis) may have either hyaline or fibrocartilage. These joints are slightly mobile. E.g., the pubic symphysis within the pelvis provides strength and stability, plus flexibility and movement during times such as pregnancy and childbirth.
Synchondroses
Synchondroses refers to where the articulating bones are connected via hyaline cartilage. For example, the epiphyseal plate (also known as the growth plate) within long bones.
Fibrous Joints
Fibrous joints lack synovial cavities. Bones are held together by dense, irregular connective tissue composed of collagen fibres that emerge from the matrix of one bone into the matrix of the next. The bones do not have a joint cavity between them and instead are directly connected to each other. The amount of movement depends on the length of the connective tissue. Some may be slightly moveable, but in general, most fibrous joints are immovable.
Fibrous joints fall into 3 categories.
- Sutures
- Syndemoses
- Gomphoses
Examples of fibrous joints include the joints which hold the teeth in their sockets, and joints holding the bones of the skull together.
Sutures
Sutures are typically found between the bones of the skull. In older adults, these sutures are immovable. However, in children and infants, they are slightly moveable. A baby's skull has 'soft spots' when born. It is this softer skull that allows movement and aids in childbirth. As the baby develops, we see the connective tissue turn to bone, and the skull grows and solidifies.
Synostosis
Synostosis is a type of suture that, as a person develops into adulthood, changes its structural composition, and some sutures are replaced by bone. When this occurs, this joint is no longer referred to as a suture but a suture that is now synostosis, where two bones have completely fused into one. Examples include:
- Bones of the skull
- Shafts and heads of long bones
- First rib to the sternum
Syndesmoses
Syndesmoses are immovable to slightly moveable. Within a suture, there is no space between the articulating bones. However, within a syndesmosis, there is more distance and volume of dense irregular connective tissue between the articulating bones of a syndesmosis.
The bones are held together by an interosseous membrane. There are two main interosseous membranes within the human body, between the tibia and fibula (shin bones) of the leg and the radius and ulna of the forearm.
Gomphoses
These are immobile joints between the teeth and their sockets.
The spine makes up approximately two-fifths of your total height.
The spine is both strong and flexible. It is strong enough to support the head, neck, and body whilst being flexible enough to facilitate movement. It also protects the spinal cord, a very delicate and fragile structure that runs down the hollow passages of the vertebral column.
Vertebrae
The spinal column is composed of 33 independent bones referred to as vertebrae. These vertebrae are divided into 5 sections where the structure of each vertebra is slightly different due to the functions each performs. The vertebrae are held together by a strong network of ligaments and cushioned by vertebral disks.
Each of the following regions of the vertebral column has a specific number of vertebrae.
The cervical
This has 7 cervical vertebrae in the neck region. From the topic vertebrae to the bottom vertebrae in this region, these are named C1- C7.
The Thoracic
This has 12 thoracic vertebrae in the chest/thorax region. From the topic vertebrae to the bottom vertebrae in this region, these are named Th1-Th12.
The Lumbar
This has 5 lumbar vertebrae in the lower back region. From the topic vertebrae to the bottom vertebrae in this region, these are named L1-L5.
The Saccrum
There is 1 sacrum, which consists of 5 fused sacral vertebrae. This is referred to as the S1.
The Coccyx
There is 1 coccyx, which consists of 4 fused coccygeal vertebrae. This is referred to as the S2.
This amounts to having 33 irregular independent bones in total.
You need to know:
- the regions
- their order
- the names of each vertebrae. (C1-C7), (Th1-Th12), (L1-L5), (S1), (S2).
- the bones in each region
- the structural changes between the vertebrae of each region
This knowledge may not be called upon daily, but it underpins the rest of your anatomy, physiology, and exercise-based knowledge.
Here is a handy mnemonic to remember the regions and the number of vertebrae:
You have Cereal at 7, Tea (cuppa) at 12, Lunch at 5 (ok, it’s a late lunch) and then a Cuddle on the Sofa at 11 (11 = 1 + 1 of the sacrum and coccyx)
Try it out
Imagine you have a client that, in pre-screening, reveals they have back pain. They share with you a referral from their sports physician to their physio. The referral includes the following:
MRI showing mild loss of disc height in T10-T11 and T11-T12 and also minor loss of disc height in T2-T3 but no changes seen in the T7 area.
Vertebral joints
Each region of the spine has varying degrees of movement due to structural differences and the presence of ribs in the thoracic region.
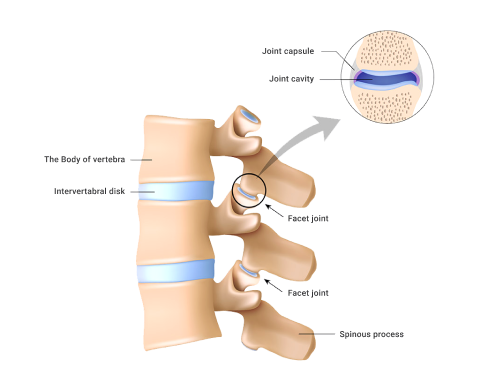
Facet joints
Located between the superior facet of one vertebra and the inferior facet of the vertebrae (refer to the preceding image). Approximately 16% of the body's load is absorbed by these joints. If they are poorly aligned, or under chronic extra stress, they can be the location of common back pain.
Intervertebral joints
Intervertebral joint ( inter~ in between, vetebral~vertebra): This joint is found between the vertebral bodies of the vertebrae. 84% of the body's load should be absorbed here if well aligned.
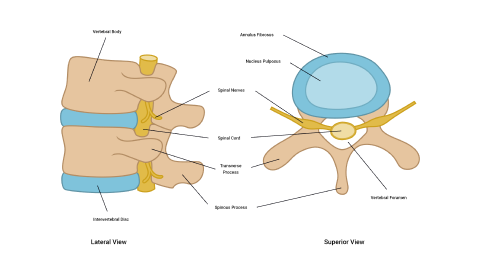
Intervertebral discs
There are 3 joints between each vertebra - 2 facet joints and 1 inter-vertebral joint. Each intervertebral joint is separated by an intervertebral disc. Together as a team, the intervertebral discs and the vertebra form the vertebral column.
The intervertebral discs are comprised of 2 main components:
- The annulus fibrosus: The annulus fibrosus are tough fibro-cartilage rings. These are very strong under compression, but susceptible to torsional (twisting) stress.
- The nucleus pulposus: The nucleus pulposus is mainly made up of water (90%) and provides shock absorption like water-filled cushions.
Did you know?
Disc height changes over the course of a day due to axial loading. This results in us being taller in the morning than at night!
Watch
Enjoy this short yet stunning 3D video of the human skeleton looking at the different regions of the spine.
As we age, we will likely experience some wear and tear, inside and out. Within the human skeletal system, degenerative conditions do present themselves. Aging usually impacts functions such as:
- synovial fluid production within a joint.
- the thinning of articular cartilage.
- the shortening of some muscular ligaments along with a decrease in flexibility.
However, with supportive lifestyle factors, a good exercise regime, and diet, the onset of these can be delayed (if not totally prevented).
Arthritis
Arthritis is an inflammation of the joint cartilage. This inflammation has a negative impact on a joint's range of motion due to a decrease in the flexibility of the surrounding ligaments. Knowing about arthritis will help you develop safe and functional exercise programmes for the elderly population that will help maintain the functions of ligaments, tendons, muscles, synovial fluid, and articular cartilage.
There are over 100 types of arthritis, but the 2 most common are osteoarthritis and rheumatoid arthritis. Can you identify the differences between a normal knee joint and one with arthritis in the following images?
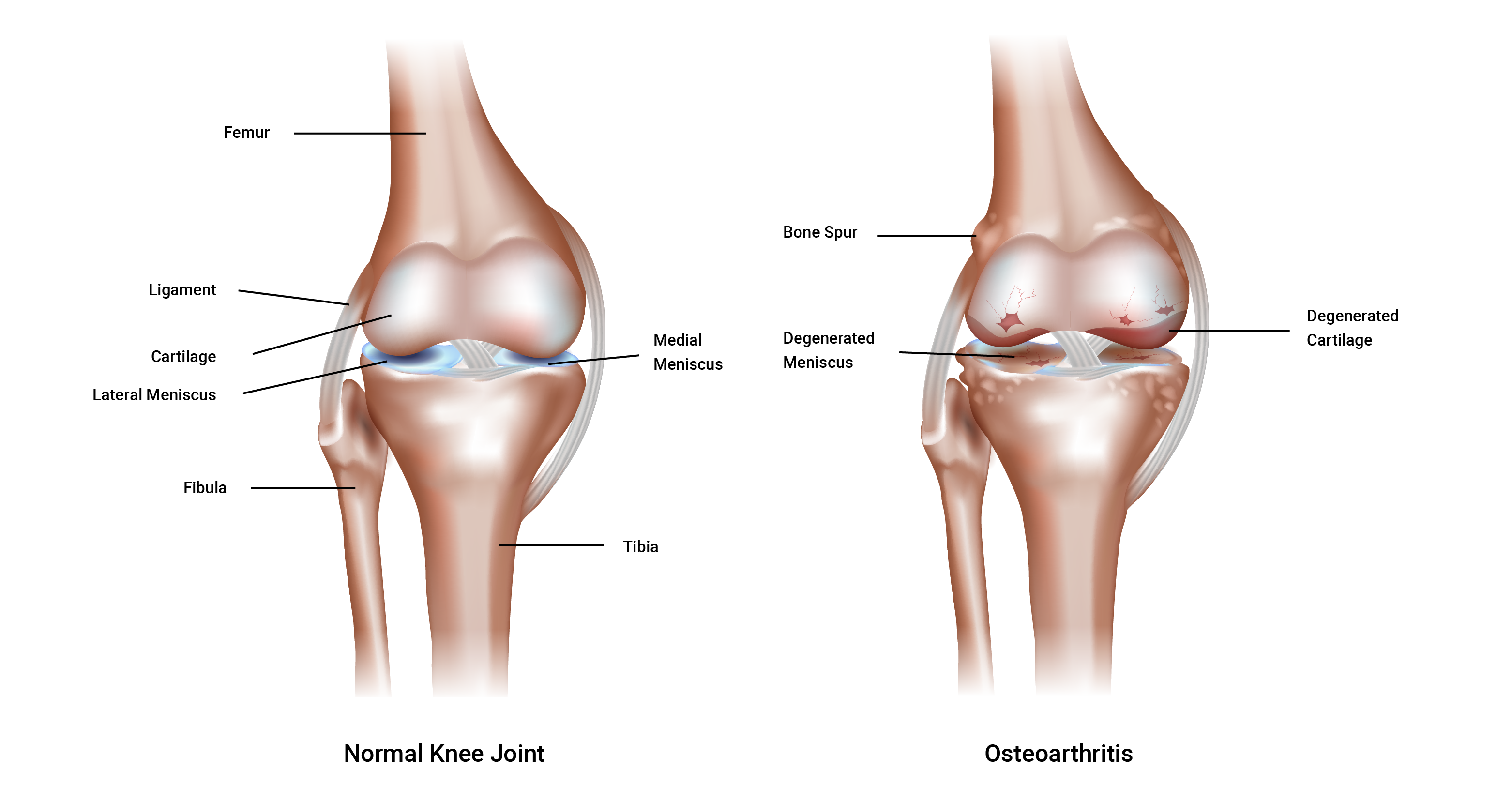
Osteoarthritis
Osteoarthritis is a largely age-related degeneration. Although this does not mean that younger generations are immune to osteoarthritis. It can be caused by wear and tear over time or disuse due to a lack of meaningful activity, leading to weakened (thinner) cartilage. This is referred to as a degenerative joint disease. The cartilage is lost from aging, obesity, joint irritation, muscle weakness, and general wear and tear. You can see the importance of effective exercise programming when working with clients who may have osteoarthritis.
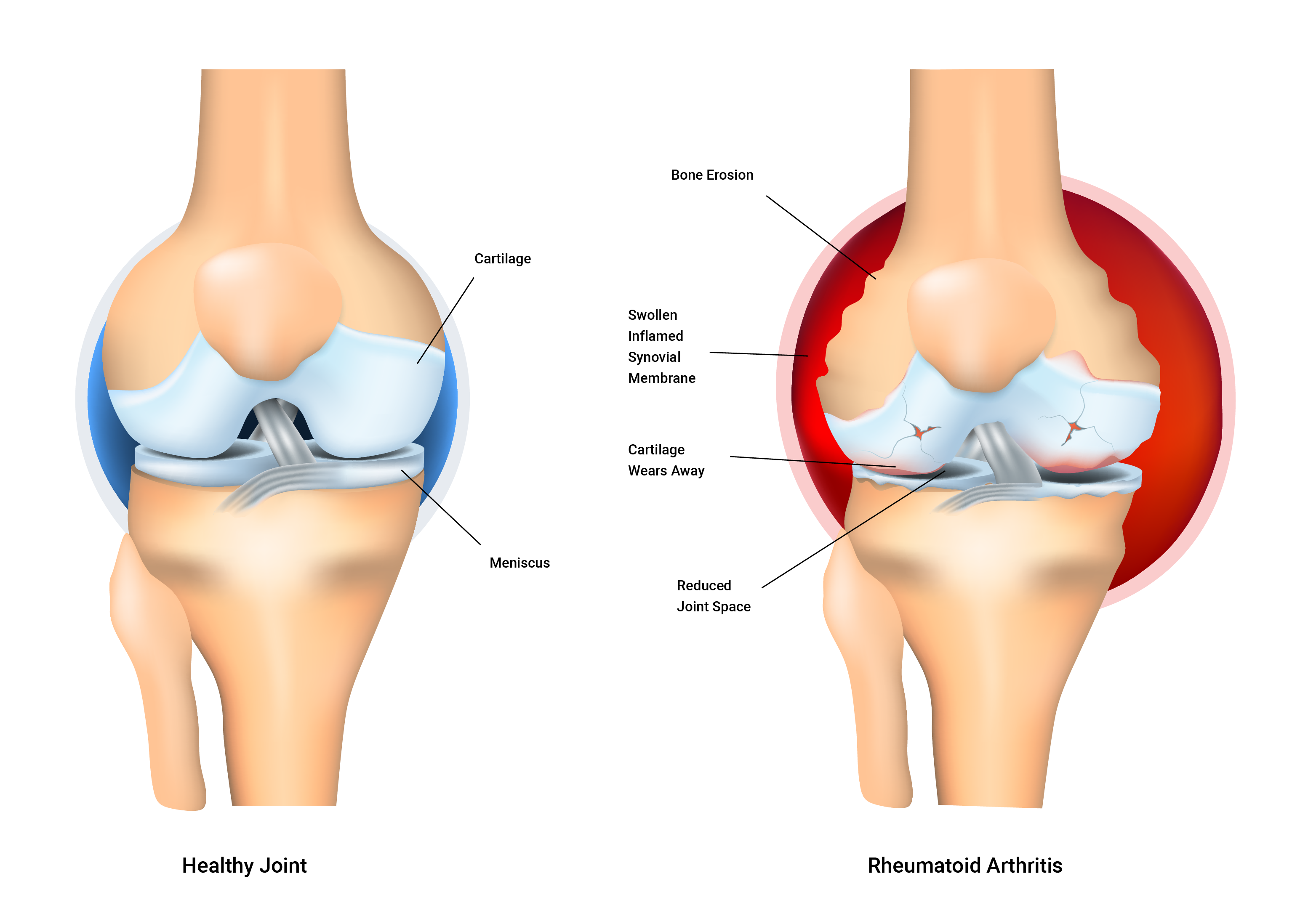
Rheumatoid arthritis
Rheumatoid arthritis is an auto-immune disorder. It occurs when your body’s immune system attacks the tissues of the body, in this case, its own joint linings and cartilage. These attacks affect the synovium.
Rheumatoid arthritis is a disease of the synovium that will invade and destroy a joint. It can eventually destroy the bone and cartilage inside the joint. It is typically characterised by inflammation of the joint, which can cause swelling, loss of function, and pain. Sadly, if one joint is affected, it is likely the other one will also be affected (but not usually to the same degree).
The exact cause of the immune system’s attacks is unknown. But scientists have discovered genetic markers that increase your risk of developing rheumatoid arthritis fivefold.
With exercise, the synovial fluid becomes less viscous and is more easily taken in by articular cartilage. This is beneficial because the synovial fluid provides essential nutrients to nourish the bone, and other cells remove unwanted debris to keep the synovial joint 'clean and tidy'. Cartilage acts like a sponge and has tiny pores that allow fluid to enter and leave.
Exercise design should consider the need for, and the benefit of, repetitive compression for nutrition and waste removal.
Connective tissue
There are 3 types of connective tissue within joints.
- Cartilage forms a cushion between bones to stop them from rubbing against each other.
- Ligaments are like strong cables or strings that hold bones together.
- Tendons attach muscles to bones or other muscles.
Joint stability vs range of motion
Unfortunately, it is difficult to achieve both ideal joint stability and ideal range of motion at the same time because an increase in one of these often occurs at the expense of the other. A balanced and well-thought-out programme design should keep this in mind.
Joint stability (resistance to displacement)
Joint stability is resistance to displacement and depends on 3 key factors:
- Joint ligaments
- Muscle tension
- Fascia tension
Let's look at each of these.
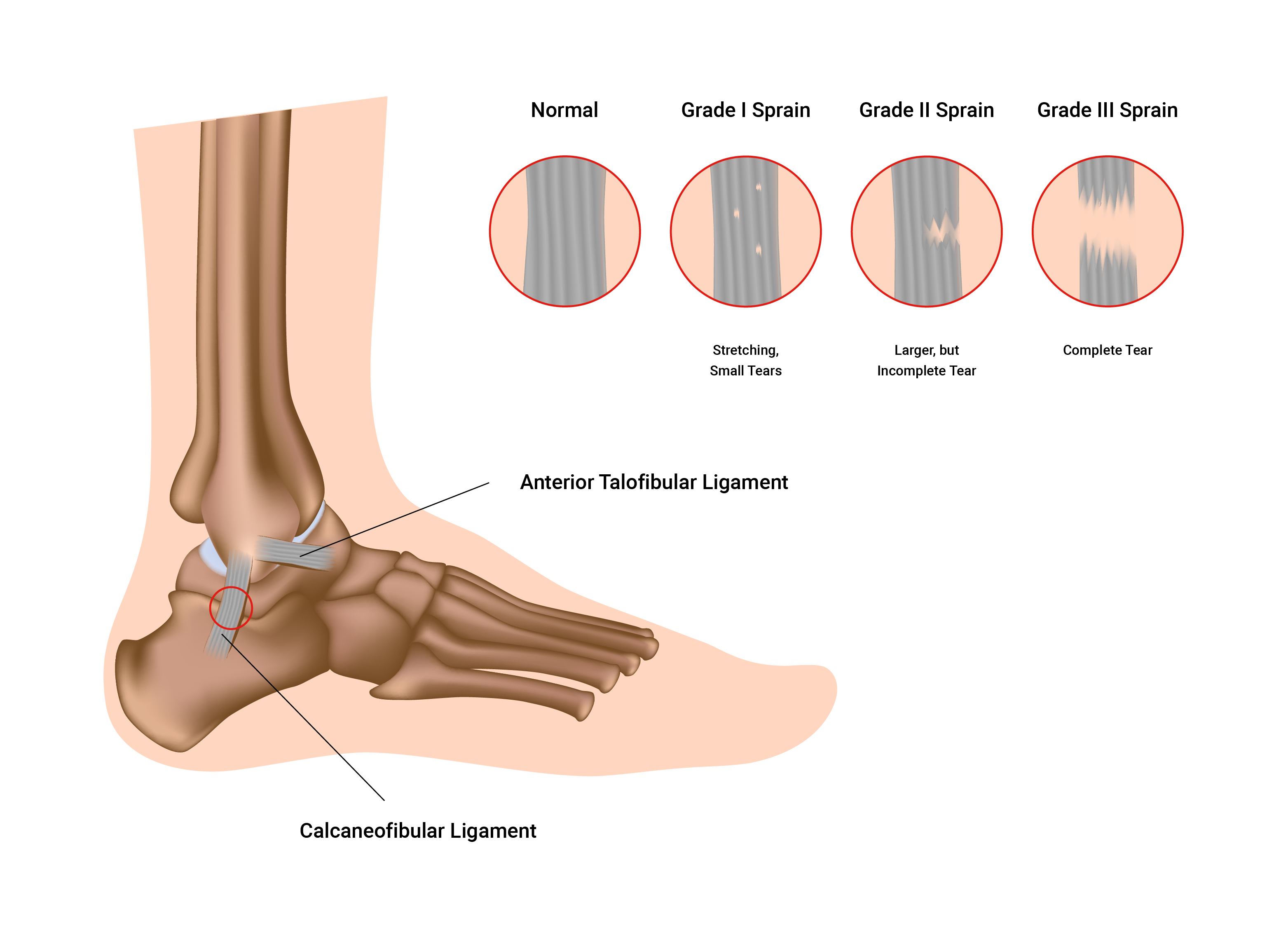
1. Ligaments
Ligaments are strong and flexible. They attach the ends of bones to form a movable joint. A ligament's main function is to maintain the correct relationship between bones. They also have receptors that monitor movement speed and range and resist undesirable movements.
Ligament injury (sprain)
Ligaments are not very elastic. If they are over-stretched, they might never regain normal length.
Once stretched, their usefulness is permanently affected and joint stability is diminished. Think of an elastic band or a hair tie. Over time and repeated use, they stretch and begin to lose their shape (become bigger, and get looser). If left to dry, they become rigid and stiff.
Sprains range in severity, often referred to as a 'grade'. This grade outlines the current health and condition of the ligament(s) affected. Sprains range from first-degree to third-degree, with the third-degree often representing a severe (or full) rupture of the ligaments, as well as other symptoms. Recovery time also increases from first- to third-degree sprains. Typically ligaments (and tendons) have a lesser blood supply than muscle tissue which means that their nutrient delivery is less so recovery will be slower.
Think about the main function of the ligament - to attach the ends of bones to form a moveable joint and maintain the correct relationship between bones - as you study the following illustration.
2. Muscle tension
Muscles help static stability and provide dynamic stability. Strength training is an important defence against joint injury. Once ligaments are damaged (lengthened), muscles around the joint must be strengthened to maintain joint stability. This can lead to unfavourable changes in their range of motion.
3. Fascia tension
Fascia is a connective tissue that wraps around individual muscle fibres and groups of muscles. It is flexible and elastic within limits. This facia supports joint stability and integrity by supporting muscle attachment. It can also cross over joints to provide extra stability.
Menisci
Some loaded synovial joints (such as the knee) have flattened, shock-absorbing pads of fibrocartilage called menisci (the singular is meniscus) between the articulating surfaces of bones. These discs support the bones in the joint by binding strongly inside the joint capsule. They also offer depth to shallow joints and help absorb shock. The complete function of the menisci is not yet fully understood however they are known to be strong contributors to:
- absorbing shock.
- providing cushioning and padding in between bony surfaces.
- distributing synovial fluid over the articular surfaces of the joint.
Range of movement
3 key factors affect the range of joint movement.
- Muscles and their tendons (flexibility)
- Bulky tissue (fat, excessive muscle)
- Disease and/or condition (pain)
Flexibility of muscle and tendon
This is the single most important factor in joint range of movement. This can only be increased through dedicated and regular stretching. There is also a genetic predisposition to flexibility.
The bony structure of your joints will ultimately determine the range of motion you can achieve. I.e., deep vs shallow sockets, and the angle of the bones at insertion. Trying to stretch beyond your structural limitations will cause bone-on-bone contact and may result in bony lesions or spurs that result in ongoing pain.
Bulky tissue
Excess fat mass may make a person more restricted in their movement and function. It may also put additional strain and pressure on the internal organs. Excess muscle mass can restrict the range of movement at joints if flexibility is not maintained. It is possible to have both though!
Disease, illness, or condition
Joint disorders, such as arthritis and autoimmune diseases like lupus, can impact joints, making them stiff and swollen. Sprains and dislocations also cause restriction of the range of movement.
Before moving to the next topic, check that you have a good grasp of joints.
Watch
The following video provides a summary of joint types and classifications.
