Afio mai, a warm welcome to Week 35! Our travels will continue along the pharmacological path as we explore drug interactions, with a focus on some common examples (like the well-known effect of grapefruit juice on certain medications). We will then take a detour into a system that we haven't visited for a while - the immune system, before meeting an entirely new body system, the lymphatic system.
Me tīmata tātou, let's get started.
Pharmacoloy recap
Welcome to our last session of pharmacology. Before we get into this session, let’s start with a quick two-question quiz before turning our focus to drug interactions and adverse effects.
Interaction mechanisms
In pharmacology, interaction mechanisms refer to the interactions between drugs as well as interactions between drugs and other compounds (such as food, supplements, or environmental substances). These interactions can affect the pharmacokinetics and pharmacodynamics of the substances involved.
As a pharmacy technician, it is important that you understand interaction mechanisms to ensure patient safety, prevent medication errors, educate patients about medication use and risks, and collaborate effectively with the healthcare team to promote safe and effective patient care.
This week, we will explore and cover the following drug interactions:
- Drugs with other drugs
- Drugs with other compounds
- Drugs with diseases
- Drugs with herbal/ natural remedies.
Interaction of drugs with other drugs (drug-drug interaction)
The interaction of drugs with other drugs presents various situations where the use of one medication may be contraindicated due to its interaction with another drug.
Can you recall instances where the administration of one drug is not recommended if a patient is already prescribed another medication?
Do you know the reasons behind these recommendations? You may recall examples from your previous learning or from the pharmacy workplace.
Examples
Read the following webpage from the New Zealand Formulary (NZF) on Drug Interaction for an overview of drug-to-drug interactions and some examples: Drug Interactions.
Important
When processing prescriptions, pharmacy software such as Toniq will flag interaction alerts. As a pharmacy technician, you must have all alerts checked by the pharmacist.
Current information, explanations and guidance about drug interactions can be found on the NZF website.
Types of drug-drug interactions
Let’s now look at the different types of drug-drug interactions:
Complexing
This is where one medication forms a chemical complex (they stick together) with another drug to form an insoluble salt that cannot be absorbed through the intestine. Therefore, the complex passes through the GI system and is excreted without doing its job.
Drugs that change the acidity of the stomach
Drugs that change the acidity of the stomach can affect the ability of a drug to dissolve in the stomach.
Motility
Motility refers to the movement of substances in the gastrointestinal tract. When one drug alters gut motility, it can affect how another drug is absorbed. This means drugs may move more rapidly or slowly through the gut, which can impact their absorption.
Sometimes, this interaction is used deliberately, as in the combination of paracetamol and metoclopramide, where the absorption of paracetamol is aided by an increase in gut motility.
Clearance
Clearance refers to the interaction where one drug affects the elimination or clearance of another drug from the body. This can occur through various routes, such as renal clearance (excretion via the kidneys), hepatic clearance (metabolism by the liver), or other metabolic pathways. When one drug alters the clearance of another, it can impact the concentration of the affected drug in the bloodstream.
Example
- Amiodarone (antiarrhythmic) stabilises the heart's electrical activity and restores and maintains a normal heart rhythm.
- Digoxin (cardiac glycoside) is used to increase the strength and efficiency of the heart muscle contractions.
Amiodarone decreases the renal clearance of digoxin, causing high digoxin levels in the body.
Scenario
Apply this knowledge to a real-life scenario. Take a moment to think about the implications of the following question before flipping the card to reveal the answer.
Drugs that act on the same site
When both drugs act at the same site, the following effects can occur:
- Additive effects: A greater overall effect than if each drug were administered alone.
- Reduced effects: The drugs may interfere with each other's action, leading to diminished therapeutic responses.
- Opposing effects: The drugs may have opposing actions at the receptor site, leading to conflicting pharmacological effects.
Drugs that act on different sites
When both drugs given in combination act on different sites, they can either:
- Potentiate (increase clinical effect) or
- Antagonise (decrease clinical effect) their pharmacological effects.
In relation to enzymes, this means that there can be an enzyme induction or enzyme inhibition.
Enzyme induction
A drug can cause the action of enzymes to increase, resulting in an increased metabolism of another drug that is metabolised using the same enzyme pathway.
On the flip side…
Enzyme inhibition
A drug inhibits the action of an enzyme, resulting in decreased metabolism of another drug.
Interactions of drugs with other compounds (drug interaction)
Drugs may interact with other non-drug compounds, which can affect the absorption, distribution, metabolism, and excretion of drugs in the body, altering their therapeutic effects. We will explore the interactions of drugs and the following compounds:
- Smoking
- Caffeine
- Grapefruit juice
- Vitamin K
- Alcohol
- Tyramine-containing foods.
Drugs and smoking
Tobacco smoke contains compounds that can induce liver enzyme activity (increase the rate), particularly cytochrome P450 (CYP) enzymes. This induction can cause drugs processed by these enzymes to be metabolised more quickly. As a result, smokers may require higher doses of medications metabolised by these enzymes to achieve the same therapeutic effect as non-smokers.
On the other hand, when a smoker quits smoking, the induction of liver enzymes decreases, and drug metabolism returns to normal. Therefore, lower drug doses may be necessary to avoid potential overdose or adverse effects in former smokers.
Scenario
Ben has been prescribed clozapine for the management of his schizophrenia. He recently took up smoking tobacco. Clozapine is primarily metabolised by the liver.
How will Ben’s smoking affect the therapeutic levels of clozapine in his body?
Jot down your answer on a scrap piece of paper and then select the label to reveal the answer.
Tobacco smoke contains substances that speed up the breakdown of clozapine in the liver. This means that Ben's body may process clozapine faster than usual, resulting in lower levels of the medication in his bloodstream. As a result of this interaction, Ben may experience a decrease in the therapeutic effects of clozapine.
Did you get the answer correct? If not, you may wish to talk to a fellow student or your tutor to strengthen your understanding.
Drugs and caffeine
Caffeine is found mainly in coffee, tea, and energy drinks. Most interactions with caffeine result from competitive inhibition. This means that the caffeine and the other drug can compete to be metabolised by the same enzyme. The ‘winner’ will be metabolised preferentially, resulting in higher levels in the body than the ‘loser’.
Examples
Examples of commonly used drugs that result in a clinically significant increase in caffeine levels are:
- Ciprofloxacin
- Diltiazem
- Fluconazole
- Norfloxacin
- Olanzapine
- Terbinafine
- Verapamil.
Patients starting these medicines may notice side effects from the caffeine.
Grapefruit juice
Grapefruit juice inhibits the enzyme cytochrome P450 3A4 in the gut wall. This means that any drug that is usually metabolised in the gut wall by this enzyme will not be broken down as much as it should be, and blood levels of the drug will be higher.
This interaction cannot be managed by just separating the doses, as the effect on the enzyme lasts several days after the grapefruit juice is stopped.
Examples
Examples of drugs affected by grapefruit juice are:
- Benzodiazepines
- Buspirone
- Carbamazepine
- Oestrogens (COCs)
- Statins
- Tacrolimus.
Note: The interaction happens with grapefruit and its juice. There is a chance that it also may happen with marmalade, so this is also contra-indicated.
Journal post
Drug-Other Compound Interaction
- Create a new journal post titled ‘Drug-Other Compound Interaction’.
- Read the following scenario and answer the two questions in your journal.
- Publish your post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
Scenario
A family member has just been prescribed 20mg of simvastatin once daily at night. Because you are a pharmacy technician, she asks why both her doctor and pharmacist told her not to drink grapefruit juice while taking this medication. She then asks you if she can have grapefruit juice if she takes it at a different time than her simvastatin.
Questions
- Why can't your family member drink grapefruit juice while taking this medication?
- Can she have grapefruit juice if she takes it at a different time than the simvastatin? Why, or why not?
Vitamin K
Foods containing vitamin K can interact with certain medications, especially anticoagulants like warfarin. Warfarin functions by interfering with the action of vitamin K, which is essential for blood clotting.
Consequently, consuming vitamin K-rich foods can counteract the effects of warfarin, potentially reducing its effectiveness in preventing blood clots. Therefore, individuals taking warfarin should be mindful of their intake of vitamin K-containing foods to maintain the medication's efficacy.
Examples
Foods that are high in vitamin K include:
- Leafy green vegetables such as kale and spinach
- Brussels sprouts
- Parsley
- Lettuce
- Cabbage
- Asparagus
- Green beans.
Alcohol
Alcohol is primarily metabolised in the liver by enzymes such as alcohol dehydrogenase, acetaldehyde dehydrogenase, and microsomal enzymes in the liver, such as cytochrome P450 enzymes.
Alcohol can amplify or diminish the effects of certain drugs, leading to unpredictable outcomes or adverse reactions.
Example
Alcohol can intensify the sedative effects of some medications, leading to increased drowsiness or impaired coordination. Conversely, alcohol can also interfere with the metabolism of certain medications, affecting their absorption, distribution, or elimination from the body. This can result in altered drug levels in the bloodstream, potentially reducing the medication's effectiveness or increasing the risk of side effects.
Tyramine-containing foods
Tyramine is an amino acid that helps to regulate blood pressure. It occurs naturally in the body and can also be found in some foods.
Tyramine-rich foods can interact with certain medications, particularly monoamine oxidase inhibitors (MAOIs). MAOIs are a class of drugs prescribed for the treatment of depression. MAOIs inhibit the breakdown of tyramine in the body, leading to an accumulation of tyramine levels. This can result in a sudden increase in blood pressure, known as a hypertensive crisis, which can be dangerous. Therefore, individuals taking MAOIs should avoid or limit consumption of tyramine-rich foods to prevent adverse reactions.
Here's a quick challenge for you. What foods do you think are high in tyramine? Note down at least three examples and then expand the following label to check your answer.
- Aged cheese
- Salami and other cured or processed meats
- Sauerkraut and other fermented or pickled foods
- Vegemite and other yeast extracts
- Some fruit and vegetables.
Interactions of drugs with diseases (drug-disease interaction)
Some drugs can interact with specific diseases or disorders, making the diseases or disorders worse. In this week's self-directed learning activity, you will see examples of these.
Interactions of drugs with herbal/ natural remedies
There are some significant interactions between drugs and natural remedies. Always check with your pharmacist if a customer who is taking a prescribed medicine wishes to buy a natural remedy.
Example
St John’s Wort (used to treat depression naturally) interacts with many medicines. It is an enzyme inducer, so it can increase the metabolism of some medicines, e.g. warfarin, digoxin and oestrogen. It also inhibits the reuptake of serotonin. If given with prescribed meds that also increase serotonin levels, serotonin syndrome may result. This is a serious problem that can be fatal.
Adverse effects
An adverse drug reaction is any undesirable effect of a drug that is not expected as part of a therapeutic effect. They are classified into two groups: A and B.
Type A reactions
- These are the most common. They are predictable because they are due to the normal actions of the drug.
- They may result from incorrect doses, decreased elimination, or increased sensitivity of organs to the drug.
- Decreased elimination results from either reduced metabolism in the liver (liver damage) or reduced clearance by the kidneys (renal damage).
- Increased sensitivity to drugs may result for varying reasons – e.g. in a patient with potassium deficiency, the heart becomes more sensitive to the effects of digoxin, resulting in digoxin toxicity.
Type B reactions
These are unexpected reactions that are not dose-related. Sometimes, neither the reason nor the mechanism for the reactions can be explained.
- Genetic factors: These factors may make a drug act in an abnormal manner.
- For example, some people of African, Middle Eastern and South Asian descent are deficient in the enzyme glucose-6-phosphate dehydrogenase (G6PD). If these people take ciprofloxacin, their red blood cells break down, resulting in pernicious anaemia.
- Host factors: These are individual patient characteristics or conditions that can influence how a person responds to a medication. These factors may include age, gender, genetics, underlying health conditions, organ function, and concurrent use of other medications or substances.
- For example, a patient with HIV is more likely to have unexpected reactions to anti-infective drugs such as co-trimoxazole.
- Women are at greater risk of developing adverse drug reactions than men due to differences in pharmacokinetic, immunological, and hormonal factors.
- Allergic reactions: These occur after initial exposure to a drug. This exposure produces antibodies to the drug, which means that the patient suffers an allergic reaction the next time the drug is administered. Subsequent exposures elicit more severe reactions, so once it is discovered that a patient is allergic to a drug (e.g. penicillin), it becomes contra-indicated.
Patient Counselling
As a pharmacy technician, you will use your understanding of anatomy and physiology to advise patients on medication use for managing health conditions. It's crucial that you effectively communicate this information to patients and their families in a clear and understandable manner.
You must be able to provide correct and accurate information about the following:
- Names of prescribed medicine - this may include the generic and trade names.
- What each medicine is used to treat - this may include mechanisms of action as appropriate.
- The dose, frequency and instructions for administration.
- Any cautionary and advisory labels that apply.
- Storage instructions.
- Side effects and anything else to be aware of as appropriate.
You will talk more about this in class.
Self-directed learning activity
To review your learning on drug interactions, watch this video that discusses:
- drug-drug interactions
- drug-nutrient interactions
- drug-food interactions
- drug supplement interactions
- drug-disease interactions
- drug-laboratory interactions.
Āta mātakitaki, watch carefully and pause to take notes about information that is additional to this week's content.
Watch: Drug interactions [...] (9:27 minutes)
Mahi pai! Excellent work! We've reached the conclusion of our pharmacology journey and wrapped up the Patient Care 2 module. As we transition into Week 36 and start new modules, we encourage you to revisit any section of the online content to reinforce and enhance your understanding. Keep up the great work, kia mau ki te mahi nui!
Kia ora, in this session, we explore the immune system and medicines for the treatment of immune disorders as well as malignant diseases. There is a lot of content to cover this week, so plan your time well, divide your learning into chunks and take regular breaks to stand up, stretch, and move around to prevent stiffness and improve circulation.
Remember to use your learning strategies, such as taking notes, summarising key points in your own words and reaching out for help or clarification if needed. You can tackle the workload efficiently and confidently with effective time management and self-care strategies. Kia kaha rā! You’ve got this!
Immune system recap
We have discussed the immune system previously when looking at the Human Defence System in Week 12, Introduction to Patient Care. That was quite a while ago! Do the phrases “specific” and “non-specific defence” ring any bells? Let's revisit and reinforce your understanding of this system, as the immune system concepts discussed in Week 12 are building blocks for the content we will cover this week.
Forum activity
- Take a moment now to reflect on what you currently know about the immune system, its purpose and the meaning behind the phrases "specific" and "non-specific defence".
- Set a timer for five minutes and jot down as much as you can remember.
- Use whatever recall method you like. You may choose to write bullet points, a table, a mindmap, or even draw pictures.
- Once you’re done, upload your notes to the forum: Week 35 - A&P: Immune System Recall. Add a comment about how you found this activity. You may like to reflect on the following:
- Did this activity help solidify your understanding of the immune system?
- Was it challenging to recall specific details?
- Would you use this activity as a study method in the future? Why, or why not?
- Make sure to have a look at your peers' notes too. You might find that you pick up a new note-taking style or identify key points you had forgotten about. This activity effectively draws your previous learning to the surface and will provide a foundation for this week's learning.
The immune system
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens, such as bacteria, viruses, fungi, parasites, and other foreign substances. It can be broadly categorised into two main components: innate and adaptive immune systems.
The innate (non-specific) immune system
The innate immune system does not give long-lasting immunity against a pathogen but is quick-acting. It responds in the same way to all types of pathogens and is triggered when pathogens are identified or when damaged, injured or stressed cells send out alarm signals. There are two lines of defence:
- The first line = barriers to prevent pathogens from entering the body. This includes the skin, mucus membranes, cilia and stomach acid.
- The second line = back up to the first line. It includes the inflammatory response, phagocytes, and interferons.
Cells of the innate immune system
This image illustrates the different cells of the innate immune system. Expand each of the following labels to read about these types. You may like to refer back to this image to visualise the cells as the content describes them.
- Mast cells are tissue-resident immune cells found in connective tissues throughout the body, particularly near blood vessels and mucosal surfaces.
- They contain granules filled with inflammatory mediators, such as histamine, heparin, and various cytokines.
- Mast cells play a key role in the initiation of inflammatory responses and allergic reactions.
- Dendritic cells are phagocytes located mainly in the tissue in contact with the external environment, such as skin, nose, lungs, stomach, and intestines.
- They capture antigens from pathogens and present them to T cells in secondary lymphoid organs, such as lymph nodes, to initiate adaptive immune responses.
- They serve as a link between tissue and the innate and adaptive immune systems.
- Phagocytes engulf or ‘eat’ pathogens or particles (phagocytosis). They actually wrap their cell membrane around the particle to engulf it, then kill and digest it.
- Phagocytes patrol the body searching for pathogens but can be called to specific locations by cytokines (molecules that send signals to alert the immune system of a problem).
- Macrophages and neutrophils are phagocytes that travel throughout the body in pursuit of invading pathogens.
- Macrophages produce a wide array of chemicals, including enzymes, complement proteins, and regulatory factors such as interleukin 1.
- Macrophages also act as scavengers, ridding the body of worn-out cells and other debris and as antigen-presenting cells that activate the adaptive immune system.
- Neutrophils are the most abundant type of white blood cell in the bloodstream. They migrate toward the site of inflammation in a process called chemotaxis (cell movement in response to a chemical message) and are usually the first cells to arrive at the scene of infection.
- Basophils and eosinophils are related to neutrophils.
- They secrete chemical mediators, such as histamine, that are involved in defending against bacteria and parasites and play a role in allergic reactions, such as asthma.
- Natural killer (NK) cells respond against virally infected cells and tumour cells.
- They identify abnormal cells by detecting changes in their surface proteins and induce apoptosis (programmed cell death) in infected or transformed cells through the release of cytotoxic granules.
The adaptive (specific) immune system
The adaptive immune system (third-line defence) mainly involves two types of white blood cells (lymphocytes).
- B lymphocytes (B cells)
- T lymphocytes (T cells)
Both lymphocytes are produced in bone marrow; however, B cells remain in bone marrow, whereas T cells travel to the thymus. There are two main types of T cells: helper T cells and killer T cells.
There are two types of adaptive immune system responses. These are:
- Humoral (antibody-mediated response): This response system uses B cells and antibodies to respond to pathogens. Antibodies can also activate the complement system, a group of proteins that enhance the clearance of pathogens.
- Cell-mediated (cytotoxic T cell response): This is where cytotoxic T cells directly target and kill infected or abnormal cells. This response is important for eliminating pathogens, such as viruses and certain bacteria, and for controlling tumour growth by destroying cancerous cells.
Cells of the adaptive system
This illustration depicts the cells of the adaptive system. As you expand each of the following labels to read about these cells, make sure to refer to this illustration to create a visual association.
- B cells play a central role in the humoral immune response.
- Upon encountering antigens, B cells differentiate into plasma cells, which produce and secrete antibodies.
- Antibodies circulate in the bloodstream and body fluids, targeting and neutralising pathogens, toxins, and other foreign molecules.
- T cells have roles in both humoral and cell-mediated immune responses.
- Helper T cells (Th cells) are involved in the activation of B cells and other immune cells.
- They help regulate immune responses and enhance the production of antibodies by B cells.
- Cytotoxic T cells (Tc cells) are responsible for cell-mediated immune responses.
- They recognise and kill virus-infected cells, tumour cells, and other abnormal cells through the release of cytotoxic molecules.
- Cytokines are signalling molecules produced by various cells of the immune system.
- They play crucial roles in regulating immune responses by modulating immune cells' activation, proliferation, and function.
You will notice that there are immune cells that participate in both innate and adaptive immune responses. These cells bridge the gap between the two systems, facilitating communication and coordination of immune responses. Later, in your SDL activities for this week, you will learn more about each of these immune systems.
Phew, as this was a lot of content to absorb, complete the following seven-question pātaitai (quiz) to check your understanding.
Lymphatic system
The lymphatic system is a system we have not discussed previously. It is part of the immune system and plays a major part in the body’s defence against infection and cancer. It is a collection of organs, ducts and tissues responsible for fighting infection and draining lymph back into the bloodstream.
Watch: The Circulatory System Part 3: The Lymphatic System (7:06 minutes)
Join our good friend, Professor Dave, as he explains what lymph is, what it has to do with the circulatory system and what the lymphatic system actually does. Feel free to take notes as you watch and then complete the short quiz that follows to summarise the difference between lymphatic vessels and lymph nodes.
Disorders of the immune system
Allergy
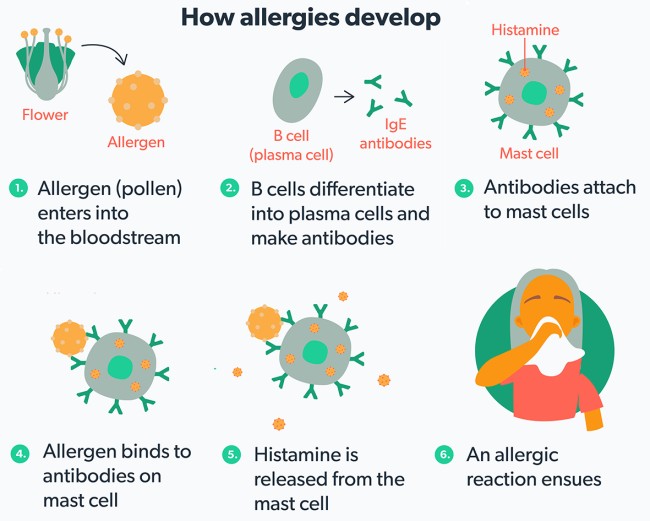
Allergies are an immune disorder caused by an inappropriate response of the immune system to a substance (allergen) that, in most people, causes no response. When an allergen enters the body for the first time, it is identified as foreign, triggering a response from plasma cells. These specialised B cells produce antibodies, specifically immunoglobulin E (IgE), against the allergen. These antibodies then attach to mast cells, which are tissue cells containing packets of histamine and other substances.
Upon re-exposure to the same allergen, it binds to the antibodies on the surface of mast cells, leading to their rupture and the release of inflammatory substances, including histamine. This release results in allergic symptoms. It is believed that individuals with higher levels of IgE are more prone to allergies, often described as atopic, experiencing conditions like asthma and eczema more frequently.
This image from Allergy New Zealand simply illustrates how allergies develop, using a common allergen, pollen, as an example.
If you wish to read more, check out the webpage here: What is an allergy?
Signs and symptoms
You will be familiar with the signs and symptoms of allergic reactions (such as hay fever). These include the following:
- Sneezing
- Runny or stuffy nose (rhinorrhoea or nasal congestion)
- Itchy nose
- Postnasal drip (mucus dripping down the throat from the back of the nose)
- Itchy, watery eyes (allergic conjunctivitis)
- Coughing (usually due to postnasal drip)
- Scratchy or sore throat.
Treatment
Treatment for allergic reactions typically involves the use of antihistamines, which function by inhibiting action at the H1 receptor. They work by blocking the effect of histamine, one of the chemicals released during an allergic reaction. Histamine causes dilation of blood vessels, leading to redness and swelling due to fluid leakage into the tissue. However, since histamine is not the sole chemical responsible for allergic reactions, antihistamines address most, but not all, symptoms of inflammation.
Other pharmacological treatments may include steroids and decongestants.
Anaphylaxis
Anaphylaxis is an immune system disorder. It is a severe allergic reaction that can occur rapidly after exposure to an allergen. During anaphylaxis, the immune system overreacts to an allergen, leading to widespread physiological (functional) changes in the body. These changes typically involve the release of various inflammatory mediators, particularly histamine, from immune cells such as mast cells and basophils.
Histamine causes:
- vasodilation (widening of blood vessels)
- increased vascular permeability (leakage of fluid from blood vessels into surrounding tissues)
- smooth muscle contraction, particularly in the airways.
Other inflammatory mediators, such as leukotrienes and prostaglandins, contribute to the systemic inflammatory response, further exacerbating symptoms. If left untreated, anaphylaxis can progress to anaphylactic shock, where a severe drop in blood pressure can lead to organ failure and death.
Journal post
Immune Disorder: Anaphylaxis
- Create a new journal post titled 'Immune Disorder: Anaphylaxis'.
- Rangahau (research) to answer the following questions. You may wish to explore these web pages to get started:
- Allergy New Zealand: Anaphylaxis
- Healthify: Anaphylaxis
- Publish your post to 'All course users' so your tutor can review your answers and ensure you're on the right track!
- As usual, you don't want to lose your valuable mahi, so save the permalink to your Index of Journal Posts.
Questions
- What body systems are involved in an anaphylactic reaction?
- What symptoms may a patient experience?
- What are the signs and symptoms that an anaphylactic reaction has progressed to anaphylactic shock?
- What are the possible outcomes if anaphylactic shock is not treated?
Treatment
Anaphylaxis is a medical emergency and is treated with adrenaline (epinephrine).
Watch: HOW DOES ADRENALINE/ EPINEPHRINE WORK [..] (3:22 minutes)
Join Maya, a woman who lives with severe food allergies, as she explains how adrenaline/epinephrine works to treat the body when suffering from an allergic reaction.
Journal post
Treatment: Adrenaline

In an anaphylactic emergency, adrenaline is self-administered via the autoinjector called EpiPen®. There are two sizes:
- EpiPen® Jnr - 0.15mg for children between 7.5 and 20kg
- EpiPen® - 0.3mg for adults and children over 20 kg.
- Create a new journal post titled 'Treatment: Adrenaline'.
- Rangahau (research) to answer the following questions.
- Publish your post to 'All course users'.
- Save the permalink to your Index of Journal Posts.
Questions
- What is the route of administration of an EpiPen®?
- What is the onset of action?
- What is the duration of action?
- Are EpiPen’s funded?
- Where can patients find information about how to use their EpiPen®?
Autoimmune disorders
These disorders are similar to allergic reactions, but instead of the allergen being a ‘foreign invader’, the immune system wrongly identifies its own tissue or organs as foreign. Autoimmune disorders occur when lymphocytes begin to produce antibodies, but the underlying cause is not well understood. There are many autoimmune disorders, but here we will discuss rheumatoid arthritis (RA).
Rheumatoid Arthritis (Mate rumatiki)
In Week 19 of Introduction to Patient Care, we looked at arthritis, noting the differences between osteoarthritis and rheumatoid arthritis. Have a look at the illustration above to review the difference between a healthy joint and rheumatoid arthritis, and then let’s recap what we know about rheumatoid arthritis:
- It is a chronic, systemic inflammatory autoimmune disorder.
- Anyone can get rheumatoid arthritis at any age, but it commonly develops between the ages of 25 and 50.
- Causes are not fully understood, but women are affected more than men, and smokers have a higher rate than non-smokers.
- It may affect many tissues and organs but mainly attacks the joints, producing inflammation of the synovial membrane that lines joints and tendon sheaths.
- Joints become swollen, tender and warm, and stiffness limits their movement, particularly early in the morning on waking or following prolonged inactivity.
- Joints are affected symmetrically. For example, if the left knee is affected the right knee will be also.
- With time, RA nearly always affects multiple joints, most often the small joints of the hands, feet and cervical spine, but larger joints like the shoulder and knee can also be involved.
- Eventually, there is a loss of movement and erosion of the joint surface, causing deformity and loss of function.
- Rheumatoid arthritis can also produce inflammation in the lungs, pericardium, pleura, and sclera, and also nodular lesions, most common in subcutaneous tissue under the skin.
- Symptoms may come and go with no particular pattern. Some people will have flares and periods of remission.
Treatment
The pharmacological treatment for rheumatoid arthritis (RA) typically involves the use of several classes of medications aimed at reducing inflammation, relieving pain, slowing down disease progression, and improving overall joint function.
Select the (+) symbols to read about each of the following treatments:
- DMARDs stands for ‘Disease-Modifying Anti-Rheumatic Drugs’.
- They are an unrelated group of drugs that are grouped together because of their use in rheumatoid arthritis to slow down the progress of the disease by modifying the immune system in some way.
- They decrease inflammation, though they are not categorised as anti-inflammatory drugs.
- They can take up to six months to reach full therapeutic effect and are best started early to limit joint damage.
- There are two main groups of DMARDs:
| Conventional DMARDs | Biological therapies |
|---|---|
| Example: Methotrexate. | Example: Infliximab |
|
Methotrexate's mode of action involves inhibition of folate metabolism, interference with purine synthesis, and modulation of adenosine signalling, leading to suppression of inflammation, reduction of immune cell proliferation, and improvement of autoimmune symptoms in RA and other autoimmune diseases. Folic acid supplementation is often prescribed at the same time as methotrexate to help alleviate the potential side effects associated with methotrexate therapy, such as gastrointestinal upset, mouth sores, and liver abnormalities. The folic acid must be taken a few days apart from the methotrexate. Some prescribers suggest ‘Methotrexate on Monday and Folic acid on Friday’ as an easy way for patients to remember what to take and when to take it. Information about methotrexate can be found at the NZF here: Methotrexate. |
The mode of action of infliximab involves targeting TNF-alpha, a central mediator of inflammation, and blocking its inflammatory effects. By neutralizing TNF-alpha, infliximab helps reduce inflammation, alleviate symptoms, and slow disease progression in conditions like rheumatoid arthritis. Its use is indicated Information about infliximab on the NZF can be found here: Infliximab. |
- Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain, swelling, and inflammation associated with RA flares.
- They provide symptomatic relief but do not alter the underlying disease process.
- Pain relievers such as paracetamol may be used to relieve pain associated with RA, particularly in combination with other medications.
- Steroids, such as prednisone and prednisolone, are potent anti-inflammatory medications used to relieve symptoms during RA flares quickly.
- They are often prescribed short-term and at the lowest effective dose due to their potential for long-term side effects.
Journal post
RA Treatment
Use the information above and any reputable resources of your choosing to provide a patient with professional advice in the following Documentation tool activity.
- Complete the following Documentation tool activity.
- Download and save the completed activity.
- Create a new journal post titled 'RA Treatment'.
- Upload the completed activity to your post and publish it to 'All course users'.
- Save the permalink to your Index of Journal Posts.
Cancer
Cancer (malignant neoplasm) is a class of diseases in which a group of cells display uncontrolled growth, invasion (intrusion on and destruction of nearby tissue), and sometimes metastasis (spread to other locations in the body via lymph or blood). Most cancers form a tumour, but some, like leukaemia, do not.
Normal cells undergo a tightly regulated process of growth, division, and death (apoptosis) to maintain tissue homeostasis. However, cancer cells acquire mutations or genetic alterations that disrupt these regulatory mechanisms, leading to uncontrolled cell growth. Tumour suppressor genes are inactivated in cancer cells, resulting in the loss of normal functions in those cells, such as accurate DNA replication, control over the cell cycle, orientation and adhesion within tissues, and interaction with protective cells of the immune system.
Cancer can arise from any type of cell in the body and is caused by a combination of genetic, environmental, and lifestyle factors. Genetic mutations can be inherited or acquired throughout life due to exposure to carcinogens (e.g., tobacco smoke, ultraviolet radiation, certain chemicals), viral infections (e.g., human papillomavirus, hepatitis B virus), hormonal factors, immune dysfunction, and other factors.
Cell growth
Here, you can compare the effects of normal and abnormal cell growth with the abnormal cell growth resulting in a malignant tumour.
Tumours
A tumour is an abnormal growth of cells that can develop in various tissues or organs of the body. Tumours can be classified into two main types: malignant (like the image above) and benign tumours. Let's look at malignant first.
Malignant tumours
These are also known as cancerous tumours. They are growths of abnormal cells that have the ability to invade surrounding tissues and spread to other parts of the body, a process known as metastasis. They often have irregular shapes, may grow rapidly, and can cause significant damage to nearby tissues and organs.
They are life-threatening and often require aggressive treatments such as surgery, chemotherapy, radiation therapy, or targeted therapy to prevent further spread and improve outcomes.
Examples
- Carcinomas (originating from epithelial tissues)
- Sarcomas (originating from connective tissues)
- Lymphomas (originating from lymphocytes)
- Leukaemia (originating from blood-forming cells).
Benign tumours
These are non-cancerous growths that do not spread to other parts of the body or invade surrounding tissues. They are typically well-defined and may grow slowly over time. They may cause symptoms depending on their size and location but are generally not life-threatening. They may require monitoring or surgical removal for symptom relief.
Examples
- Uterine fibroids
- Lipomas (fatty tumours)
- Moles.
Breast Cancer (Mate pukupuku ūtaetae)
Oestrogen and progesterone receptors are proteins found on the surface of breast cells. These receptors are present in healthy breast cells and help control the way breast cells grow, but in 70% of breast cancers, the receptors are over-expressed. These cancers are called hormone-sensitive or hormone receptor-positive, meaning that oestrogen and progesterone can attach to the receptors and fuel the growth of the cancer.
Breast cancer can be divided into two groups:
- Non-invasive (in situ) - cancerous cells that remain confined within the ducts or lobules of the breast tissue and have not spread into surrounding healthy tissue. It is considered an early stage of breast cancer (pre-invasive).
- Invasive - cancerous cells that have breached the basement membrane of ducts or lobules and have invaded surrounding healthy breast tissue. It has the potential to spread (metastasise) to nearby lymph nodes and other organs of the body via the bloodstream or lymphatic system.
Treatment
Pharmacological treatments for breast cancer include a variety of medications that target different aspects of the disease. Here, we will focus on tamoxifen.
Tamoxifen is a type of hormonal therapy used in the treatment of hormone receptor-positive breast cancer. Hormone receptor-positive breast cancer refers to a type of breast cancer in which the growth of cancer cells is driven by the presence of hormone receptors (oestrogen and progesterone) on the surface of the cancer cells. Tamoxifen works by blocking the oestrogen receptors in the cancer cells to prevent them from responding to signals from the oestrogen to grow and multiply.
Journal post
Breast Cancer
- Complete the following Documentation tool activity.
- Download and save the completed activity.
- Create a new journal post titled 'Breast Cancer'.
- Upload the completed activity to your post and publish it to 'All course users'.
- Save the permalink to your Index of Journal Posts.
Melanoma (Mate pukupuku kiri manauri)
Melanoma is a type of skin cancer originating from melanocytes, pigment-producing cells in the skin. It primarily affects the integumentary system, which includes the skin, and can occur anywhere on the body but is most commonly found in sun-exposed areas.
Melanoma occurs when melanocytes undergo malignant transformation and begin to grow uncontrollably. If left untreated, melanoma can invade deeper layers of the skin, blood vessels, and lymphatic vessels, allowing it to spread (metastasise) to other parts of the body, such as the lymph nodes, lungs, liver, brain, or bones.
Stages of melanoma
Here, you can see the five stages of melanoma, with the tumour becoming malignant as it spreads.
Signs and symptoms
Melanoma is less common than other types of skin cancer but is more aggressive and has a higher risk of metastasis. Signs and symptoms may include:
- The fast appearance of a new spot or mole on the skin.
- An existing spot, freckle or mole that changes colour, size or shape (see the ABCDE of Melanoma illustration below).
- A spot that is itchy, tender, painful or bleeds.
- A spot that is raised or shiny.
Journal post
Melanoma
New Zealand has the highest rate of melanoma in the world. It's important not only as a pharmacy technician to know the causes and risk factors for developing melanoma but also for yourself, your whānau and your friends.
- Create a journal post called 'Melanoma'.
- Research to find the following:
- Causes and risk factors for developing melanoma.
- How this type of cancer can be prevented.
- Publish your answers to 'All course users'.
- As always, save the permalink to your Index of Journal Posts.
Treatment
Treatment for melanoma depends on various factors, such as the disease's stage, the tumour's location and size, and the individual's overall health.
One type of pharmacological treatment is immunotherapy. It activates or enhances the body’s immune response against cancer cells.
Example
Let’s look at the example of the drug pembrolizumab.
Pembrolizumab is typically administered intravenously in a hospital setting. It is a type of medication known as an immune checkpoint inhibitor, belonging to a class of drugs called monoclonal antibodies.
Pembrolizumab works by inhibiting PD-1 receptors found on immune cells. These receptors play a crucial role in distinguishing between normal and foreign cells. When foreign cells, such as pathogens or cancer cells, are detected, the immune system responds by initiating an attack to eliminate them. However, cancer cells can mimic normal cells to hide from immune detection. Pembrolizumab blocks PD-1 receptors, preventing cancer cells from hiding from the immune system. This action enhances the immune response, enabling the identification, attack, and elimination of cancer cells.
Papillary thyroid cancer
The thyroid lies at the front of the neck, beneath the voice box (larynx) and is shaped like a butterfly. As you can see in the illustration, it has two lobes that are separated by a thin section called the isthmus. You will remember from previous weeks of learning that the thyroid gland produces hormones that regulate metabolism and other essential functions in the body. These hormones include the following:
- Thyroxine (T4) plays a key role in regulating metabolism, growth, and development and maintaining body temperature and energy levels.
- Triiodothyronine (T3) is the biologically active form of thyroid hormone that is derived from thyroxine (T4). It is more potent than T4 and is involved in many of the same physiological processes, including metabolism, growth, and development.
- Calcitonin is a hormone produced by special cells in the thyroid gland called C cells or parafollicular cells. It helps regulate calcium levels in the body by inhibiting the breakdown of bone and promoting calcium excretion by the kidneys.
Signs and symptoms
Papillary thyroid cancer is a type of thyroid cancer. It often presents as a painless lump or nodule in the thyroid gland. While it can spread to nearby lymph nodes, papillary thyroid cancer generally has a favourable prognosis when diagnosed and treated early.
Thyroid cancers usually develop slowly without any obvious symptoms. The following signs and symptoms can be experienced, but they also occur in conditions that are not thyroid cancer:
- Painless lump or nodule in the front of the neck near the Adam's apple.
- Trouble swallowing or breathing.
- Voice changes, e.g., hoarseness.
- Swollen glands (lymph nodes) in the neck.
Treatment
Depending on the type and stage, thyroid cancer may be treated with surgery, radioactive iodine, hormone treatment, external radiation, or chemotherapy. Some patients receive a combination of treatments.
Radioactive Iodine Therapy
This treatment uses radioactive iodine (I-131, an isotope created from iodine to emit radiation) to destroy thyroid cancer cells anywhere in the body. The intestine absorbs the I-131, which flows through the bloodstream and collects in thyroid cells. Radioactive iodine is chemically identical to nonradioactive iodine. Therefore, the thyroid gland, which takes up iodine to make thyroid hormone, cannot distinguish between the two. Thyroid cancer cells remaining in the neck and those that have spread to other parts of the body are killed when they absorb I-131. It is a targeted treatment. It will not affect other body cells as only thyroid cells pick up iodine.
Radioactive iodine therapy is typically administered orally in the form of a capsule or liquid solution. It may be administered as an outpatient or, if the dose is high, as an inpatient in isolation to protect others from exposure to radiation. After treatment, the radioactive iodine is excreted from the body through urine and sweat over time. Most radiation is gone in a few days. Within 3 weeks, only traces of radioactive iodine remain in the body.
Self-directed learning activity
To round this week off, we have a two-part self-directed learning activity. Follow the instructions to create two separate journal posts, one investigating radioactive iodine therapy and the other where you will do some further rangahau (research) into breast cancer.
Journal post #1: Radioactive iodine therapy
- Create a new journal post titled ‘Radioactive Iodine Therapy’.
- Using reputable resources, answer the following questions.
- Publish your post to ‘All course users’.
- Save the permalink to your Index of Journal Posts. This will allow you to check for feedback and use your hard work for future reference.
Questions
- What precautions does a patient need to follow after the administration of radioactive iodine therapy?
- Why must these precautions be taken?
- How long must these precautions be taken?
Journal post #2: breast cancer detection
- Create a separate journal post titled ‘Breast Cancer Detection’.
- Watch the video that follows, and then do your own rangahau (research) to answer the questions below:
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts.
Watch: Breast checks and mammograms - Breast Cancer Foundation NZ (5:31 minutes)
Questions
- Breast cancer is more common in what age group of women?
- Can men get breast cancer?
- What are the risk factors for developing breast cancer?
- What are the signs and symptoms of breast cancer that people should look out for?
Whakamihi! Congratulations! We've successfully concluded our study of anatomy and physiology, reaching the end of this module. Make sure to complete the Learning Check-in before we meet again in Week 36 where we focus on selecting medicines to treat disorders of different body systems.
