Introduction Mālō e lelei, welcome to this week's learning. This week, we will focus on the organs we use to interpret the world: to take in a beautiful sunset, enjoy the scent of freshly mown grass, hear our friends’ laughter and drink our favourite beverage. Can you guess what we might be… facing? Later this week, we will explore the physiology of diabetes, the causes and symptoms, possible treatments and medication and the impact diabetes has on the body.
In our last Patient Care 2 session, we discussed the musculoskeletal and integumentary systems.
This week, we face the following body organs:
- Eyes
- Ears
- Nose
- Pharynx (throat)
Eye – (Karu or Whatu)
The adult eye is a sphere that is approximately 2.5 cm in diameter. Each eye is located within the protective sockets of the skull, known as eye sockets or orbits. The eyes are the sensory organs responsible for vision.
Structure
For a small part of the body, the anatomy and structure of the eye is fairly complex and has many parts. As some of these are well known to us, test your knowledge of each part's function before expanding the label to see if there’s any information that’s new to you.
Upper and lower eyelids, also known as palpebrae, are thin folds of skin and muscle. Their function is to protect the eye from external factors such as dust, debris and light. Blinking movements of the eyelids clear the surface of the eye and distribute tears for lubrication.
These project outward from the upper and lower eyelids. They act as additional protective barriers against particles (such as dust) in the air as they subtly change airflow around the eye, preventing these particles from landing on the eye.
The white part and tough outer coat of the eye (so no surprise that ‘sclera’ comes from the Greek word for ‘hard’). It maintains the structural integrity of the eye and provides support for all the other eye tissues.
This is the thin layer that lines the front of the sclera and also the inner surfaces of the eyelids. It contains glands that secrete lubricating fluids. The conjunctiva is important in keeping the eye moist and in protecting the eye from infection.
The retina is a light-sensitive layer of tissue at the back of the eye. It contains specialised cells, including photoreceptors called rods and cones:
- Rods are concentrated in the peripheral regions of the retina, are highly sensitive to low levels of light and are crucial for peripheral and low-light vision.
- Cones are primarily concentrated in the central part of the retina, particularly in a small area called the macula. They are responsible for central and colour vision and divide the world into three colours: blue, green and red. There are three types of cones, each sensitive to different wavelengths of light, allowing for colour discrimination.
This is the layer between the retina and sclera. It is full of blood vessels and is responsible for supplying nutrients to the retina. The dark melanin pigment in the choroid absorbs any excess light in the eye.
This modest dome-shaped goggle is the clear, front window of the eye. It is transparent, which allows light to enter the eyeball.
As light passes through the cornea, it becomes refracted. Together with the lens, the cornea is responsible for focusing light onto the retina and does about two-thirds of the eyeball’s focusing – the lens does about a third.
The lens is located just behind the iris. It is attached to the ciliary body. Along with the cornea, it is responsible for focusing light onto the retina. It can change its thickness and, therefore, can change the focus from far to near objects and vice versa (we call this “accommodation”).
This is a clear, watery fluid that fills the anterior chamber of the eye, which is the space between the cornea (the clear front part of the eye) and the lens. This fluid’s function is to maintain the eye's shape, correct ocular pressure and provide nourishment to the cornea and lens. Aqueous humour is continually produced by the ciliary body, a structure behind the iris.
This is the coloured part of the eye – the colour depends on the amount of pigment in the iris. This membrane sits between the cornea and the lens.
The iris is responsible for controlling the amount of light that enters the eye through the pupil. When there is too much light, the iris muscles constrict the pupil to restrict the amount of light entering the eye. Conversely, when it is dark, the iris muscles dilate the pupil to allow as much light to enter the eye as possible.
This is positioned just behind the iris. Its two main functions are to produce aqueous humour and to change the thickness of the lens by stretching or relaxing.
The round opening in the centre of the iris. It appears black and adjusts in size based on the light entering the eye. In bright conditions, the pupil constricts (becomes smaller) to limit the light that enters, protecting the sensitive retina. In low light conditions, the pupil dilates (becomes larger) to allow more light into the eye, enhancing visibility.
The vitreous humour makes up the vitreous body. It is a jelly-like substance that fills the vitreous cavity between the lens and the retina. It is transparent, which allows light to be focused onto the retina. The vitreous humour also helps the eye to maintain its shape.
This nerve is composed of over one million nerve fibres. It transmits information from the retina to the brain, where it is interpreted as visual information.
Fun fact: As the optic nerve is the pathway that sends the information out of the eye and is fairly thick (about the thickness of a pencil), this is why humans experience a ‘blind spot’ in our vision.
As you can see, although there are many parts that make up the eye, essentially, the eye is a camera. At the front of this camera, we have the lens and cornea that capture passing images and project them onto the retina at the back of the eye. There, photoreceptors convert them into electrical signals and send them along the optic nerve to the brain.
Watch: How the Eye Works Animation […] (3:22 minutes)
Mātakitaki, watch this animation that explains how the eye works and the disorders of near and far-sightedness and then complete the activity that follows to summarise your understanding of these disorders.
Tears
Tears are a clear, saline fluid produced by the lacrimal glands above each eye. Tears keep the eye moist and lubricated and clean the eye of debris. They also provide an antibacterial action and form a smooth, regular surface on the eye, preventing distortion of light.
In other parts of the body, the blood vessels transport oxygen via the blood, but as the cornea is transparent, it has no blood vessels to supply the oxygen. Instead, the cornea receives oxygen from the air that dissolves in tears.
Tears are continuously produced, and excess tears, along with debris and waste products, are drained through small openings called puncta located in the inner corners of the upper and lower eyelids. From the puncta, tears travel through the lacrimal canals into the lacrimal sac, into the nasolacrimal duct, and into the nasal cavity. A blockage can occur at any point in the tear drainage system. When that happens, tears do not drain properly. Symptoms may include watery eyes and increasing risk of eye infection and inflammation.
Fun/sad fact: As far as we can tell, humans are the only creatures that cry from feeling (emotional tears). We also don’t know why we cry from emotion, as there is no physiological benefit. (Bryson, 2019).
Here, you can see what is happening in the eye when the tear duct is blocked.
Journal post
Eye Disorders
Two disorders of the eye that you will be familiar with are:
- Conjunctivitis
- Dry eye
To revise and consolidate your previous learning, explore the anatomical structures, symptoms and treatments involved in these disorders.
- Download and complete this worksheet: Patient Care 2 - Eye Disorders - Worksheet.
- To deepen your comprehension of these specified eye disorders and gather extensive information for your worksheet, you can use trustworthy online resources to help you.
- Upload the completed worksheet to a new journal post titled ‘Eye Disorders’.
- Publish the post to ‘All course users’ for tutor feedback.
- Save the permalink to your Index of Journal Posts to make it easier to navigate back to.
Ears, Nose and Throat (ENT)
The ears, nose and throat are connected by the eustachian tube and therefore treated as one medical specialty known as ‘ENT’ (this may be another acronym to add to your glossary!).
The eustachian tube is located in the middle ear, connecting it to the nasopharynx, the upper part of the throat (pharynx) behind the nasal cavity.
Functions
The eustachian tube’s functions are to:
- Equalise air pressure on both sides of the eardrum. This is crucial for maintaining optimal conditions in the middle ear for hearing. Swallowing, yawning, or chewing helps open the eustachian tube, allowing air to flow in or out and equalise pressure.
- Drain off fluid from the middle ear to the throat. This drainage helps prevent fluid build-up, reducing the risk of ear infections.
- Prevent pathogens or fluid from entering the middle ear from the throat.
Now, let’s explore each component that makes up the ENT speciality. You will be familiar with much of this content from your previous learning.
Ears (Taringa)
- Scapha
- Helix
- Temporal muscle
- Temporal bone
- External acoustic meatus (Ear canal)
- Malieus
- Stapes
- Semicircular canals
- Cochlea
- Vestibular nerve
- Cochlear nerve
- Eustachian tube
- Tympanic cavity
- Incus
- Tympanic membrane (Eardrum)
- Cartilage
- Auricular lobule (Earlobe)
- Concha
- Antihelix
- Triangular fossa
The ear is the sensory organ responsible for hearing and maintaining balance. This amazing organ consists of three main parts: outer, middle and inner ear.
Let’s explore these three main parts and discover common disorders that can impact them.
Outer ear
The outer ear includes the visible portion called the pinna or auricle and the ear canal.
- The pinna helps collect sound waves and directs them into the ear canal.
- The ear canal is a tube that extends to the eardrum.
Fun fact: Although our outer ears all function in the same way, they are distinctive, like our fingerprints. They appear to be entirely unique to each person! (Bryson, 2019).
Common Disorder - Otitis Externa (Swimmer's Ear)
This infection or inflammation of the ear canal is often caused by water exposure, leading to pain, swelling, and sometimes discharge.
Middle ear
The middle ear is located behind the eardrum, the tympanic membrane. It contains three small bones called the ossicles:
- malleus (hammer)
- incus (anvil)
- stapes (stirrup).
These bones amplify and transmit sound vibrations from the eardrum to the inner ear.
The middle ear is connected to the back of the throat by the eustachian tube, which helps equalise air pressure.
Common Disorder - Otitis Media
This infection or inflammation of the middle ear is commonly seen in children. It can cause ear pain, fluid build-up, and potential hearing loss.
Inner ear
The inner ear consists of the cochlea and the vestibular system.
- The cochlea contains the nerves responsible for hearing and contains fluid-filled channels lined with hair cells that convert sound vibrations into electrical signals sent to the brain.
- The vestibular system, located in the inner ear, is essential for balance and spatial orientation.
Common Disorder - Meniere's Disease
A disorder of the inner ear characterised by vertigo, hearing loss, tinnitus (ringing in the ears), and a feeling of fullness or pressure.
Nose (Ihu)
The nose is the body’s primary organ of smell. It also functions as part of the body’s respiratory system. The nose consists of external and internal components.
As you read about the following components, refer to the illustrations to visualise their location and relation to the other components.
External components
- The nasal bone, cartilage, and fat define the shape of your nose and house the nostrils.
- Nostrils (nares) are the visible openings at the base of the nose through which air enters.
- The septum is a combination of bone and cartilage along the centre of the nose that divides it into two nasal cavities.
Internal components
- Each nostril leads to a nasal cavity. This is where breathed-in air is filtered by cilia, hair-like structures inside the nostrils, before entering your lungs. Each nasal cavity is lined with mucus membranes and respiratory (epithelium) cells.
- Nasal conchae (turbinates) are three bony shelves on each side of the nasal cavity that help filter, humidify, and direct airflow.
- The olfactory region is in the upper part of the nasal cavity, containing olfactory receptors for the sense of smell.
- The nasal sinuses are air-filled cavities within the bones surrounding the nasal cavity. These sinuses are:
- Frontal: Located in the forehead.
- Maxillary: Situated in the cheekbones.
- Ethmoid: Found between the eyes.
- Sphenoid: Located behind the ethmoid sinuses.
Functions
The key functions of the nose are:
- Breathing: The nose is the primary passage for inhaling and exhaling air. It filters, warms, and humidifies the air as it enters the respiratory system.
- Smelling (Olfaction): The olfactory region in the upper part of the nasal cavity contains olfactory receptors, allowing the nose to detect and identify various odours.
- Fun Fact: Although humans all have 350 – 400 types of receptors, only about half of these are common to all people. This means we don’t smell the same things (Bryson, 2019).
- Air filtration: Nose hairs and mucus help trap particles, dust, and pathogens in the air, preventing them from reaching the lungs.
- Humidification: The nasal mucous membranes add moisture to the air, preventing the respiratory tract from drying out and maintaining optimal conditions for lung function.
- Voice resonance: The nasal passages contribute to the resonance of the voice, influencing speech and sound production.
Common disorders
Common disorders of the nose include:
Deviated septum
A shift in the nasal septum (the cartilage dividing the nostrils) that can cause nasal congestion and difficulty breathing.
Allergic Rhinitis
An allergic reaction that causes sneezing, itching, congestion, and a runny nose.
Pharynx | throat (korokoro)
The throat, also known as the pharynx, is a muscular tube at the back of the mouth and nasal cavity, connecting it to the oesophagus and larynx. You will remember this image from previous content, as this is a crucial part of the digestive and respiratory systems.
Structure
The throat is divided into three parts:
- Nasopharynx
- Oropharynx
- Laryngopharynx (also known as hypopharynx).
Expand the labels to find out more about each of these parts.
- The upper part of the throat (pharynx), it is located behind the nasal cavity and is associated with the nose.
- Connects the nasal cavity to the rest of the pharynx. It serves as a passageway for air from the nasal cavity to the rest of the respiratory system.
- It contains the adenoids, a collection of lymphoid tissue that plays a role in immune function.
-
It is important for various functions, including the passage of air during breathing and the drainage of mucus from the nasal cavity.
- Located behind the mouth.
- Extends from the soft palate to the epiglottis.
- Contains the palatine tonsils on each side.
- Located below the oropharynx.
- Extends from the epiglottis to the oesophagus.
Functions
The functions of the pharynx are:
- Air passage: The pharynx acts as a common pathway for air, connecting the nasal cavity and mouth to the trachea. It allows air to pass from the upper respiratory system into the lower respiratory system.
- Swallowing: Muscles in the pharynx contract to propel food from the mouth into the oesophagus, preventing it from entering the windpipe (trachea).
- Speech and sound production: The pharynx contributes to speech and sound production by resonating and modifying the sound waves produced by the vocal cords in the larynx.
- Immune function: The tonsils, located in the pharynx, are part of the immune system. They help protect against infections by trapping and fighting bacteria and viruses.
Common disorders
Common disorders of the throat include:
Tonsillitis
Inflammation of the tonsils, often causing throat pain and difficulty swallowing.
Throat infections
Infections caused by bacteria or viruses lead to symptoms like pain, swelling, and difficulty swallowing.
Summary
Ka pai mai hoki, that’s fantastic! You've successfully delved into the study of the eye and ENT.
As a pharmacy technician, your role involves offering advice and care to patients with health issues connected to these body systems. A solid understanding of human anatomy, particularly in these areas, is crucial for your role in providing effective support and assistance to those seeking pharmaceutical guidance.
Self-directed learning activity
Eye & ENT
Your SDL for this week is to review the anatomy and key functions of the eye and ENT.
- Download this worksheet: Patient Care 2 – Eye and ENT – Worksheet. (Note: it is a ZIP file, so you will need to open it to find the worksheet.)
- Follow the instructions to complete the worksheet and save it to your device.
- Upload the completed worksheet to a new journal post titled ‘Eye & ENT’.
- Publish the post to ‘All course users’.
Another week of Patient Care 2 is now complete! Treat yourself to a well-deserved break before tackling this week’s Anatomy and Physiology.
Kia ora, welcome to this session where we pick up where we continue to explore the pancreas and the endocrine disorder of diabetes.
Diabetes
Understanding diabetes is essential for pharmacy technicians so that they can provide informed, safe and empathetic care. According to the Ministry of Health (2022), over 250,000 people in New Zealand have been diagnosed with diabetes, most with type 2.
Diabetes in Aotearoa
Take a look at this infographic from Diabetes New Zealand to see the extent to which diabetes impacts the Aotearoa New Zealand population.
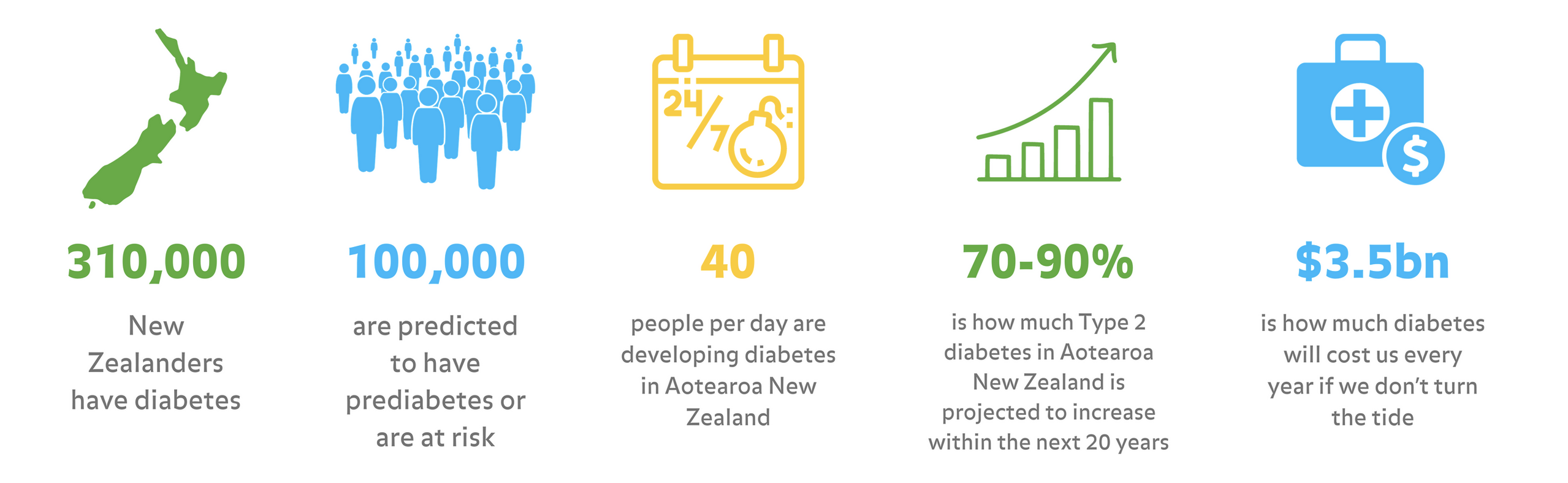
As you can see, the impact of diabetes on Kiwis is huge and set to keep rising.
Pancreas review
During previous learning of Anatomy and Physiology, our focus was on the endocrine function of the pancreas. Before delving into the discussion of diabetes disorders, it is highly recommended that you return to this section to refresh your knowledge.
Use this link to revisit last week's learning: Week 29. Use the keyboard shortcut CTRL + F | Command + F and search ‘Pancreas’ to find the content.
Important
It's essential that you establish a solid foundation of the normal structure and function of each body system before exploring disorders and their treatments. Should you have any questions regarding the pancreas, feel free to bring them to ask your tutor and pharmacy colleagues.
Types of diabetes
There are different types of diabetes, each with its own complications and ways to manage them, and generally different pathologies.
Journal post
Diabetes
In this tūmahi (activity), you will carry out your own research to answer questions about the different types of diabetes and share your findings in a journal post.
- Complete the following Documentation tool activity.
- Download and save the completed activity.
- Create a new journal post titled ‘Diabetes’.
- Upload the completed activity to the journal post and publish the post to ‘All course users.’
- Save the permalink to your Index of Journal Posts. Your tutor may review your answers and provide feedback, making it easier to check back!
Type 2 diabetes (Mate huka)
Let’s take a deeper dive into Type 2 diabetes.
Watch: 1a Diabetes – Overview & Symptoms (4:26 minutes)
Mātakitaki mai, watch here to see a simple overview of type 2 diabetes and hear people with diabetes talking about how the disorder has affected them.
Watch: Understanding Type 2 Diabetes (3:45 minutes)
Mātakitaki this video for a more in-depth look at the physiology of type 2 diabetes.
Journal post
Diabetes: Type 2
Your friend Talia has more questions about diabetes.
- Complete the following Documentation tool activity.
- Download and save the completed activity.
- Create a new journal post titled ‘Diabetes: Type 2’.
- Upload the completed activity to the journal post and publish the post to ‘All course users.’
- Save the permalink to your Index of Journal Posts. As your tutor may review your answers and provide feedback, this will make it easier to return to.
Monitoring and managing diabetes
Blood glucose monitoring
Monitoring blood glucose is a cornerstone of diabetes management. Blood glucose levels reflect the amount of sugar in the bloodstream, and maintaining these levels within a target range is crucial for people with diabetes.
As pharmacy technicians, you'll encounter various tools and devices for blood glucose monitoring, ranging from glucose meters to continuous glucose monitoring (CGM) systems. Patients rely on accurate readings to make real-time adjustments to their diabetes management plans.
HbA1c testing
As well as daily glucose monitoring, HbA1c testing provides a valuable long-term perspective on blood sugar control. Haemoglobin A1c (HbA1c) is a measure of average blood glucose levels over the past two to three months. This test is used to diagnose type 2 diabetes and to check the blood glucose levels of people with type 2 diabetes.
HbA1c results guide healthcare providers in adjusting treatment plans, setting blood sugar targets, and preventing the onset of diabetes-related complications.
Read this Healthify webpage on the HbA1c test: HbA1c test – monitoring type 2 diabetes.
Make sure to watch the video clip on the page that discusses the role of HbA1c testing in reducing complications from diabetes.
Oral hypoglycaemics
In the previous tūmahi (activity), you looked at lifestyle changes as the first line, no-pharmacological (non-medicine) treatment for type 2 diabetes. If this is not successful in reducing blood sugar levels, then pharmacological treatments will be introduced in addition to continuing with lifestyle changes.
Metformin
When it comes to pharmacological treatments, the first line of treatment is oral hypoglycaemic medications such as metformin. Metformin belongs to the class of medications known as biguanides.
It is the most prescribed oral hypoglycaemic. Its action is to lower blood glucose. It does this in two ways:
- Decreasing the amount of glucose released from the liver where it is stored.
- Making the cells more sensitive to the effects of the insulin the body produces, which enables more glucose to be absorbed into the cells from the bloodstream.
Metformin acts in the presence of naturally occurring insulin, so it is only effective if the pancreas is still producing some insulin.
Journal post
Metformin
Conduct research to learn about the use of metformin for type 2 diabetes.
- Create a journal post titled ‘Metformin’.
- Research to answer the questions below. You can use these helpful links to get you started:
- Healthify: Metformin for diabetes
- New Zealand Formulary: metformin hydrochloride
- Healthify: Medicines for type 2 diabetes
- Healthify: Metformin FAQ
- Publish the post to ‘All course users’.
- Save the permalink to your Index of Journal Posts, as this will be a useful resource to refer to later.
Questions
- What are the side effects that a patient taking metformin might experience, and what should they do about them?
- Does metformin cause weight gain?
- Metformin may reduce the absorption of what vitamin?
- What dose and frequency of metformin is typically prescribed for the treatment of type 2 diabetes?
- What CALs should be attached to metformin and explained to patients?
Gliclazide
Another oral hypoglycaemic medication is Gliclazide, which belongs to the class of medications known as sulfonylureas. They are currently considered third or fourth-line treatment options in the management of type 2 diabetes and are prescribed when symptoms persist despite the use of metformin with other blood-glucose-lowering therapy and attempts at dietary modification.
Sulfonylureas, like biguanides, act mainly by increasing insulin production and are, therefore, only effective when the pancreas is able to produce some insulin still. Over time, they can also increase insulin sensitivity.
Activity
- Read the following resources:
- Healthify: Gliclazide
- New Zealand Formulary: gliclazide
- Make your own notes on:
- The side effects and what to do about them.
- What CALs should be attached to gliclazide and explained to patients?
Sodium-glucose co-transporter 2 (SGLT2) inhibitors
Another class of oral hypoglycaemic that you may come across in the pharmacy are sodium-glucose co-transporter 2 (SGLT2) inhibitors.
These medications work by inhibiting the reabsorption of glucose in the kidneys, leading to increased urinary excretion of glucose and, consequently, lowering blood glucose levels.
An example of this class of medication is empagliflozin. It may be used on its own or in combination with other blood glucose-lowering treatments.
There are other classes of oral hypoglycaemics that you may wish to discuss with your pharmacy colleagues.
Hypoglycaemic attacks
Consider this - how might an oral hypoglycaemic medication cause a hypoglycaemic attack?
Challenge yourself to take a minute to reflect on your learnings before expanding the answer.
Oral hypoglycaemic medications, including drugs, work by either:
- stimulating the release of insulin from the pancreas or
- increasing the sensitivity of tissues to insulin.
While these medications are effective in lowering blood sugar levels, there is a risk of hypoglycaemia if the medication causes an excessive insulin response or if there is a mismatch between the medication dose, food intake, and physical activity.
How did you go? If your answer was incorrect, ask yourself if you understand the correct answer. If it’s not sinking in yet, no fear! Take a break to refresh your brain, and then test yourself to answer the question again.
Treatments for type 2 diabetes: Insulin
Patients with type 1 diabetes always need insulin therapy since their pancreas doesn't produce insulin due to an autoimmune reaction that destroys insulin-producing beta cells.
In certain instances, patients with type 2 diabetes may also need insulin therapy as their condition advances or if their pancreas's insulin production decreases over time.
The route of administration for insulin is subcutaneous, which means that insulin is injected into the fatty tissue just beneath the skin.
Insulin cannot be given in an oral form as it degrades in the stomach, making it ineffective.
Injection sites
The most common injection sites include the abdomen, thigh, and upper arm. The choice of injection site can depend on individual preferences, the specific insulin regimen, and recommendations from healthcare providers. It's important for individuals with diabetes to rotate injection sites to avoid developing lumps or changes in the fatty tissue under the skin.
Injection methods
Subcutaneous insulin injections can be delivered using various methods, providing flexibility and options for individuals managing diabetes.
Complete the next activity to view three of the most common methods.
Watch: What is an insulin pump? (2:30 minutes)
This video demonstrates how an insulin pump is attached and operates. As you watch, consider the benefits of this injection method and who it might be suitable for.
Journal post
Insulin storage
As a pharmacy technician, a crucial aspect of your role involves educating patients on proper insulin storage.
- Create a journal post titled ‘Insulin Storage’.
- Share your advice for patients on maintaining insulin effectiveness and safety. Make sure to include instructions for insulin in current use and unopened insulin.
- Publish your post to ‘All course users’.
- Save the permalink to your Index of Journal Posts, as this may be a helpful resource to refer to later in your studies and for assessment.
Types of insulin
There are different types of insulin, each with a different onset, peak and duration of action.
Click on the (+) symbol for a reminder of these terms.
The onset of action is the time it takes for a drug to become effective after administration. It also means the drug has reached its Minimum Effective Concentration (MEC).
In other words, how quickly insulin lowers blood sugar.
Peak is the maximum drug concentration in the blood after a single dose of the drug. It provides the maximum therapeutic effect in the body at this stage.
In other words, when insulin is at maximum strength.
This is how long the therapeutic effect lasts. The period starts when the drug reaches minimum effective concentration after administration and lasts until it is dropped down to minimum effective concentration after reaching peak effect/concentration.
In other words, how long insulin works to lower your blood sugar.
Let's look at five different categories of insulin. They are:
- Rapid-acting insulin
- Short-acting insulin
- Immediate-acting insulin
- Long-acting insulin
- Pre-mixed insulin
Hoake tatou, let’s go!
Rapid-acting insulin
This type of insulin is often used to manage mealtime spikes in blood sugar levels.
Onset: Rapid-acting insulin starts working quickly, typically within 15 minutes after injection.
Peak: Its peak effectiveness occurs about 1 to 2 hours after injection.
Duration: Its effects last for about 3 to 4 hours.
Dosing: The frequency of dosing may be multiple times per day, depending on the number of meals and snacks eaten.
Examples
| Product | Drug | Onset, peak, duration | Presentation | Appearance | |
|---|---|---|---|---|---|
| NovoRapid |  |
Insulin Aspart | Onset: 10 - 20 minutes Peak: 1 - 3 hours Duration: 3 - 5 hours Suitable: IV, SC infusion via pump, or injection. |
|
Clear |
| Apidra | 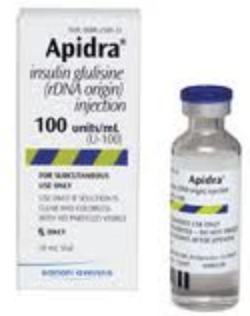 |
Insulin Glulisine | Onset: 15 minutes Peak: 60 minutes Duration: 2 - 4 hours Not suitable: IV Suitable: SC pump, or injection. |
|
Clear |
| Apidra Solostar | 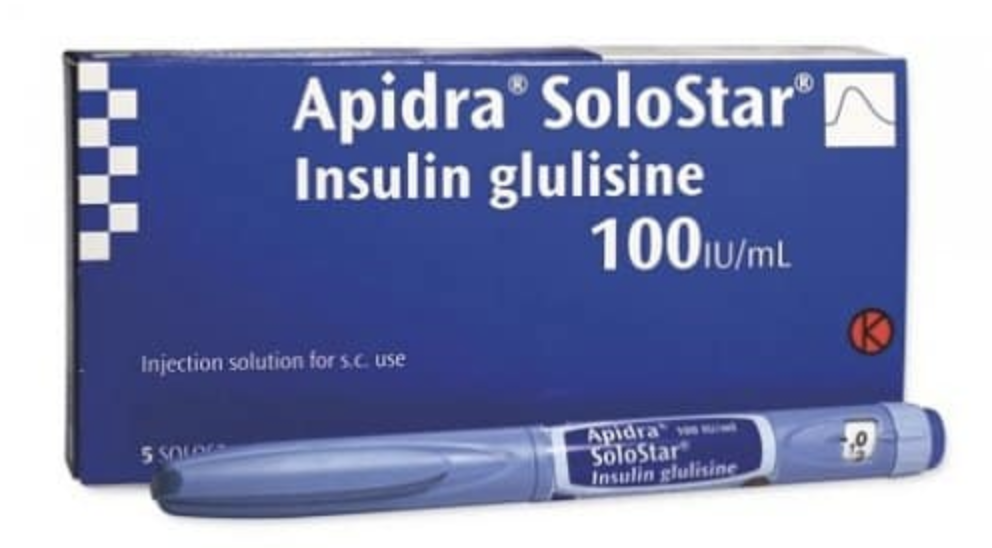 |
Prefilled disposable pen | Clear | ||
| Humalog |  |
Insuline Lispro | Onset: 15 minutes Peak: 30 - 70 minutes Duration: 2 - 5 hours Suitable: IV, infusion pump, or injection. |
|
Clear |
Short-acting insulin
Short-acting insulin is commonly used to cover blood sugar increases related to meals.
Onset: Short-acting insulin begins to work within 30 minutes after injection.
Peak: The peak effect occurs 2 to 3 hours later.
Duration: Its duration of action is around 3 to 6 hours.
Dosing: The frequency of dosing may be multiple times per day, often before main meals.
Examples
| Product | Drug | Onset, peak, duration | Presentation | Appearance | |
|---|---|---|---|---|---|
| Actripid |  |
Insulin Neutral (soluble) | Onset: ≤ ½ hour Peak: 1 - 3 hours Duration: 8 hours Suitable: IV, IMI, SC injection |
|
Clear |
| Humulin R |  |
Insulin Neutral (soluble) | Onset: 30 - 60 minutes Peak: 2 – 4 hours Duration: 8 - 12 hours Suitable: IV, SC injection |
|
Clear |
Intermediate-acting insulin
This type of insulin is often used to provide a basal (background) level of insulin over a more extended period.
Onset: Intermediate-acting insulin has a slower onset, usually starting within 2 to 4 hours after injection.
Peak: Occurs around 4 to 12 hours after injection.
Duration: It can last up to 18 hours or more.
Dosing: The frequency of dosing is typically once or twice a day, depending on the specific insulin regimen.
Examples
| Product | Drug | Onset, peak, duration | Presentation | Appearance | |
|---|---|---|---|---|---|
| Humulin NPH |  |
Insulin Isophane | Onset: 1-2 hours Peak: 4-12 hours Duration: 15-24 hours Not suitable: IV, IM infusion pump |
|
Cloudy suspension |
| Protophane |  |
Insulin Isophane | Onset: ≤ 1.5 hours Peak: 4 – 12 hours Duration: ≤ 24 hours Not suitable: IV, IM infusion pump |
|
Cloudy suspension |
Long-acting insulin
Long-acting insulin is used to maintain a consistent background level of insulin throughout the day and night.
Onset and duration: Slow and steady release, providing a basal level of insulin over an extended period, often up to 24 hours.
Peak: It typically doesn't have a pronounced peak.
Dosing: The frequency of dosing is usually once a day, although some individuals may require twice-daily dosing.
Examples
| Product | Drug | Onset, peak, duration | Presentation | Appearance | |
|---|---|---|---|---|---|
| Lantas |  |
Insulin Glargine | Onset: 1.1 hours Peak: None Duration: 24 hours Suitable: SC injection only Not suitable: IV, IM infusion pump |
|
Clear |
| Lantus Solostar |  |
SoloStar prefilled disposable pen | Clear | ||
| Levemir |  |
Insulin Detemir (rys) | Onset: ≤ 1.5 hours Peak: 4 – 12 hours Duration: ≤ 24 hours Not suitable: IV, IM infusion pump |
prefilled disposable device | Clear |
Pre-mixed insulin
Pre-mixed insulin contains a combination of short-acting or rapid-acting insulin with intermediate-acting insulin.
This type of insulin is convenient for some individuals, as it provides both mealtime coverage and a basal insulin component in one injection. Pre-mixed insulin is available in different ratios to accommodate individual insulin needs.
Dosing: The frequency of dosing can vary but is often once to three times per day, depending on the specific product and the individual's meal and insulin needs.
Examples:
- NovoMix 30 FlexPen
- PenMix 30, PenMix 40, PenMix 50
- Humulin 30/70
- Mixtard 30
- Humalog Mix 25, Humalog Mix 50
Test your knowledge
There was a bit to absorb there! Complete this four-question quiz to check (and aid) your retention.
Supporting patients
Pharmacy technicians play a crucial role in diabetes management by assisting patients in various aspects of their medication and overall care. They contribute to diabetes management in many ways, including accurate and timely dispensing of diabetes medications, including insulin and oral medications.
They also provide education and information to patients on proper medication usage, storage, potential side effects, adherence to prescribed treatment plans and support better understanding and self-management.
Self-directed learning activities
Activity 1
Although pharmacy technicians aren't directly responsible for instructing patients in insulin self-administration, it's important for you to understand the process to offer effective support and encouragement to patients undergoing insulin therapy.
Watch the following patient education videos demonstrating insulin administration through syringe and vial, as well as pen devices. As you watch, take notes for future reference or create a mind map, connecting the new information to what you’ve already learned this week. You might be impressed by how much you already know!
Watch: How to inject insulin as an adult […] (3:40 minutes)
Watch: How to Use insulin Bottle Injection for Diabetes (3:23 minutes)
Activity 2 - Optional
Consider how you would feel if you had recently been diagnosed with diabetes and were required to inject insulin. What could a pharmacy technician do to support you?
Activity 3
- Create a journal post titled ‘SDL - Insulin’.
- Find the answers to the following questions and record your answers in your journal.
- You can use these useful links to get you started:
- Healthify: Insulin syringes and needles
- Healthify: Insulin pens
- You can use these useful links to get you started:
Questions
- What size needles are available in NZ?
- What strength insulin is fully funded in NZ?
- Are insulin pens pre-fitted with needles?
- How many subsidised needles can a patient in NZ receive on prescription?
This completes our exploration of the endocrine system. You have now completed your Anatomy and Physiology learning for another week. Good work, he pukumahi koe, you are a hard worker for getting through!
