When your clients hire you, they trust that the programme you design, will not hurt them. They expect a safe training program. Knowledge of the skeletal system is critical to creating an injury-free fitness plan.
A sound understanding of the skeletal system helps you recognise structure and movement issues. It makes it easier to identify where an issue may arise and how to correct it.
In this topic, you will learn:
- Bone development
- Bone functions
- Bone shapes
- Bone identification
- The spine
- Bone mineral density
- Poor bone health
The images below show the skeleton from different perspectives. In this topic, we look at bones, what they do, how they grow, and how they all fit together to make up the skeleton (in other words, their 'structure and function').
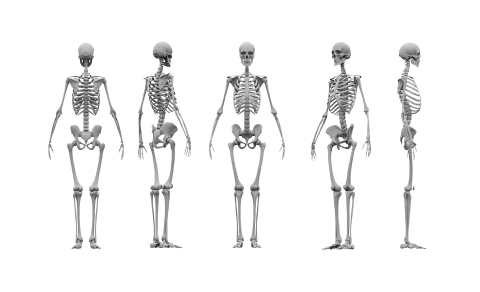
Welcome to your very first system of the human body, the skeletal system!
Bone anatomy
Bone is composed of several types of tissues working together. These are bone, cartilage, adipose, connective tissue, and nervous tissue. This is why each bone in your body is technically considered an organ.
Development
Bone is classified as a dynamic living tissue as it continues to perform a process called 'remodelling', which is the process of new bone-forming and the breaking down of old bone.
Bones determine your body's dimensions - your size and proportion. Our bones begin to form after just six weeks as a foetus and continue to grow until a person is approximately 25 years of age.
Research suggests peak bone mass may be considerably lower for females. Scientists think it is now important for young women to endeavour to build 'bone banks' while young to lay down as much bone as possible before they turn 20 years old. To do this, we must ensure adequate calcium in our diet and perform regular loaded exercise.
Watch
This video explains how bones grow naturally inside the body and considers how bones might be grown outside the body in the future. Watch the video and complete the summary.
The skeletal system is responsible for 6 main functions.
- Support
- Protection
- Movement (assistance in movement)
- Blood cell production
- Mineral storage and release
- Storage (adipose/fat storage)
You need to be familiar with these functions as this will support you in achieving a more complete understanding of the human body and medical conditions that affect the skeletal system. The skeletal system and its functions impact how you will design programmes.
Support
The skeleton provides a structural framework, like scaffolding, which provides a structure for our body. Without the skeleton, we would essentially be a 'blob'. It also provides an attachment site for muscles, ligaments, and tendons.
For example, the vertebrae supports the torso and head.
Protection
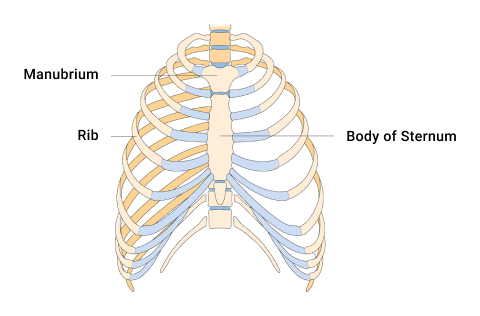
Bone is the hardest substance in your body. It is used in many places to protect the vulnerable organs underneath from outside forces. Examples include the ribs protecting the vital internal organs such as the heart and lungs, and the cranium protecting the brain. Remember, structure mirrors function. There is a reason we are built the way we are!
Movement (assistance in movement)
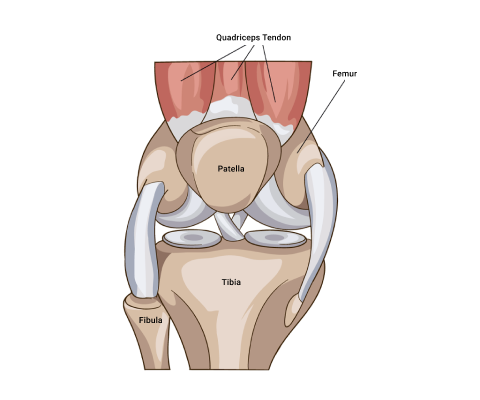
Bones provide attachment points for ligaments and tendons. Muscles are attached to bones via tendons. The bones act as rigid levers for movement to occur. This movement is articulated by joints. When a muscle contracts, it shortens and pulls on the bone it is attached to. As a result, movement occurs.
What are some everyday movements your body performs? Which bones make this movement possible?
Blood cell production
The soft, spongy material in the middle of bones is called bone marrow. It produces approximately 95% of the body's blood cells.
Both red and white blood cells are formed in the bone marrow. Red blood cells (erythrocytes) carry oxygen from the lungs to the rest of the body. White blood cells fight infections and help the immune system. Platelets are another type of blood cell that is formed in the bone marrow and helps to control bleeding (John Hopkins Medicine, n.d.).
The following picture shows the many blood components produced in the bone marrow.
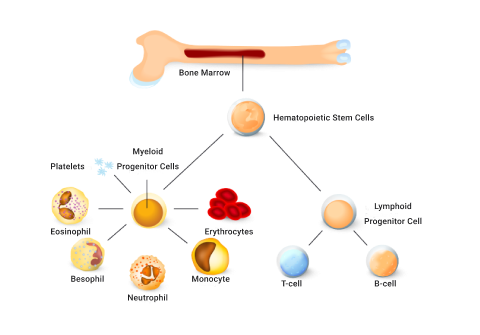
In children, blood cells are created in long bones like the femur. In adults, blood cells are mostly formed in the spine (vertebrae), hips, ribs, skull, and sternum.
Mineral storage and release
Bone is the body’s main storage of calcium. It stores around 99% of the body’s calcium and releases it when needed. Calcium is hugely important for bone growth and development and many other functions in the human body, such as muscle contraction.
Bones also store iron, potassium, and phosphorus and release them into the blood when the body needs to use them.
The pelvis, sternum, vertebrae, and clavicle are all important bones for mineral storage and release.
Storage (adipose/fat storage)
Fat tissue is also stored within the bone in the bone marrow. Bone marrow is primarily located in the ribs, vertebrae, sternum, and pelvic bones. This is additional energy storage and can be released when required to maintain physiological processes.
Watch
The following video provides a good overview of the major functions of bones.
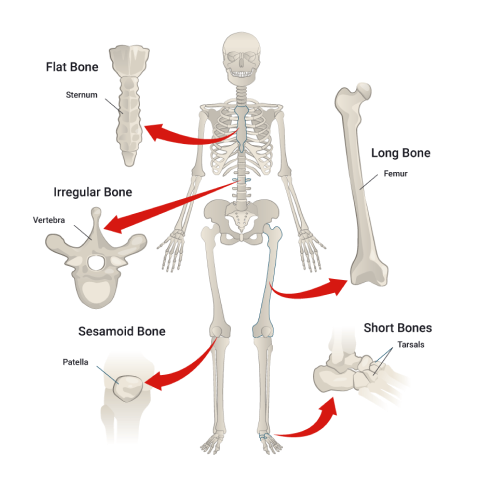
Bones come in different shapes and sizes. The shape and size depend on the role of the bone.
There are 5 different shapes of bone.
- Flat
- Long
- Short
- Irregular
- Sesamoid
The structure once again mirrors function. The shape of the bone provides a clue to the function of the bone. Let's take a closer look at bone shapes, structure, and function.
Flat bones
Flat bones offer protection and many sites for ligament and tendon attachment. They provide coverage of large areas. Examples include:
- Cranium
- Ribs
- Sternum
- Scapula
- Pelvis
Long bones
A long bone is typically longer than it is wide. Long bones can act as levers for muscles to act on. Examples include:
- Humerus
- Radius
- Ulna
- Femur
- Tibia
- Fibula
- Metacarpals and metatarsals
- Phalanges.
A typical long bone consists of the regions shown in the following diagram. To fully understand both the skeletal system and also its relationship with exercise, you must familiarise yourself with these regions and their components.
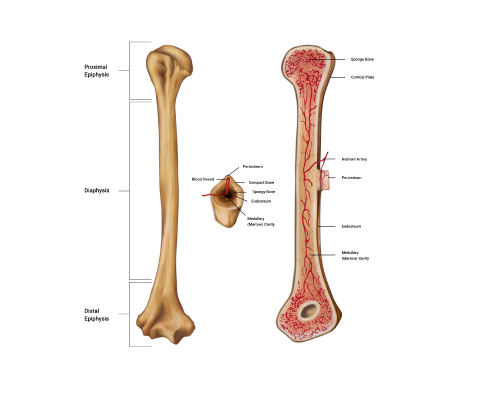
Regions of a long bone explained
The 3 main regions of a long bone are the proximal and distal epiphyses, the diaphysis, and the medullary cavity.
- The epiphyses (e-pif-i-seez): These are found at both the proximal and distal ends of a long bone and named accordingly. The singular is epiphysis. The regions are typically the widest regions of a long bone and are filled with spongy bone (houses red bone marrow) and covered with a shell of compact bone.
- The diaphysis (di- af-y-sis): Known as the 'bone shaft' or 'body', this is the middle section of a long bone. The diaphysis is long, cylindrical, and hollow. The diaphysis connects with both the proximal and distal epiphyses.
- The hollow region of the diaphysis is known as the medullary cavity. This is where we find yellow bone marrow and many blood vessels (in adult bones). The hollow design of a long bone enables great strength to be achieved whilst maintaining a long yet lightweight bone which is much easier for our muscles to help move than a heavy, dense structure.
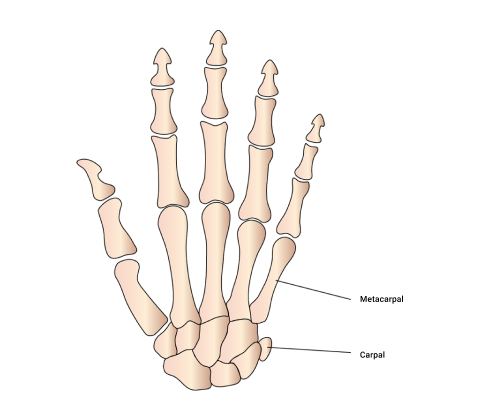
Short bones
These are equal in length and width. They cannot move much but can move in most directions a little. They provide stability and can facilitate some movements. Examples include:
- Carpals (wrist)
- Tarsals (feet)
- Talus (where the tibia meets the foot)
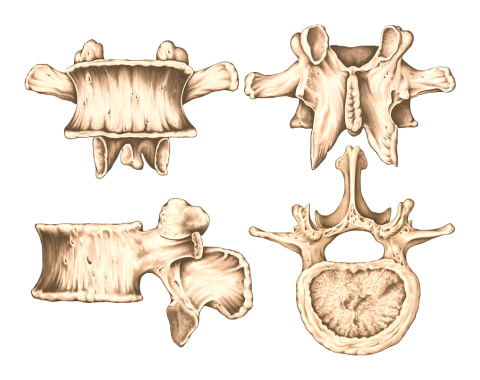
Irregular bones
These vary in shape and don't fit into any other category. They often have a complex shape which aids their role in protecting internal organs. Examples include:
- Vertebrae of the spine (protecting the spinal cord)
- Pelvic bones (ileum, ischium, and pubic, which protect our pelvic organs)
Sesamoid bones
Derived from the Latin sesamum meaning 'sesame seed' due to its typically small size. These bones are often embedded within a muscle or a tendon. They relieve tension within muscles and tendons, allowing for increased weight-bearing and tolerance by redistributing forces throughout a muscle or tendon. In doing so, the sesamoid bones protect the muscles and tendons from significant strain and injury. Examples include:
- In the patella (knee cap) - this is the most common sesamoid bone
- Others can be found in the hand and the foot
Watch
Enjoy the following video, which gives a colourful and simple summary of bone shapes, examples of their location, and the functions of each.
These are the main bones you should know the locations of. Study these carefully. If you are keeping a personalised vocabulary reference guide, add these bone names to it. You may also wish to create flashcards to practice your recall.
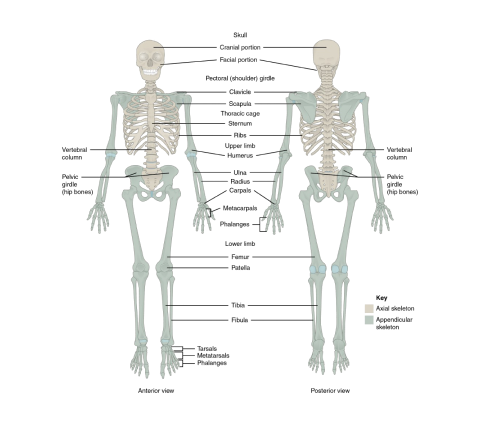
The adult human skeleton is comprised of 206 named bones. Most of these are paired, that is, they have a 'friend' on the other side of the body. What’s on the left is typically on the right also. The skeletons of infants and children have more bones than the adult human skeleton. This is because, as our skeletons develop, our bones fuse together (e.g., bones of the skull) and therefore, the total number of bones decreases.
Bones are anatomically grouped into two different divisions. This enables speedy identification and provides an idea of their role in the skeleton.
Divisions of the skeleton:
- Axial skeleton
- Appendicular skeleton
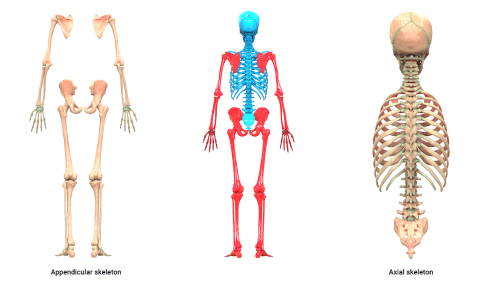
Axial skeleton
The axial skeleton is represented in blue in the preceding image. Eighty (80) bones exist within the axial skeleton. The term axial implies axis. So you can figure out that structures down the body's midline (the spine is our imaginary midline) form the axial skeleton.
- Skull
- Face
- Auditory bones (ossicles)
- Vertebral column
- Sternum and ribs
Appendicular skeleton
The appendicular skeleton is represented in red in the preceding image. These bones include everything that 'hangs off' the axial skeleton - the appendages. The appendicular skeleton consists of 126 bones. This includes the bones of the:
- Arms and legs
- Pelvis
- Hands and feet
Can you name all the bones in the image below? Additional research may be needed.
The spine makes up approximately two-fifths of your total height.
The spine is both strong and flexible. It is strong enough to support the head, neck, and body whilst being flexible enough to facilitate movement. It also protects the spinal cord, a very delicate and fragile structure that runs down the hollow passages of the vertebral column.
Vertebrae
The spinal column is composed of 33 independent bones referred to as vertebrae. These vertebrae are divided into 5 sections where the structure of each vertebra is slightly different due to the functions each performs. The vertebrae are held together by a strong network of ligaments and cushioned by vertebral disks.
Each of the following regions of the vertebral column has a specific number of vertebrae.
The cervical
This has 7 cervical vertebrae in the neck region. From the topic vertebrae to the bottom vertebrae in this region, these are named C1- C7.
The Thoracic
This has 12 thoracic vertebrae in the chest/thorax region. From the topic vertebrae to the bottom vertebrae in this region, these are named Th1-Th12.
The Lumbar
This has 5 lumbar vertebrae in the lower back region. From the topic vertebrae to the bottom vertebrae in this region, these are named L1-L5.
The Saccrum
There is 1 sacrum, which consists of 5 fused sacral vertebrae. This is referred to as the S1.
The Coccyx
There is 1 coccyx, which consists of 4 fused coccygeal vertebrae. This is referred to as the S2.
This amounts to having 33 irregular independent bones in total.
You need to know:
- the regions
- their order
- the names of each vertebrae. (C1-C7), (Th1-Th12), (L1-L5), (S1), (S2).
- the bones in each region
- the structural changes between the vertebrae of each region
This knowledge may not be called upon daily, but it underpins the rest of your anatomy, physiology, and exercise-based knowledge.
Here is a handy mnemonic to remember the regions and the number of vertebrae:
You have Cereal at 7, Tea (cuppa) at 12, Lunch at 5 (ok, it’s a late lunch) and then a Cuddle on the Sofa at 11 (11 = 1 + 1 of the sacrum and coccyx)
Try it out
Imagine you have a client that, in pre-screening, reveals they have back pain. They share with you a referral from their sports physician to their physio. The referral includes the following:
MRI showing mild loss of disc height in T10-T11 and T11-T12 and also minor loss of disc height in T2-T3 but no changes seen in the T7 area.
Vertebral joints
Each region of the spine has varying degrees of movement due to structural differences and the presence of ribs in the thoracic region.
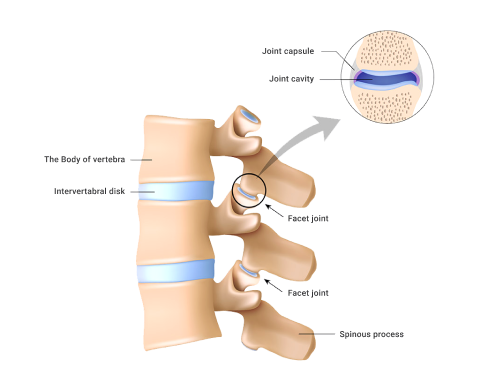
Facet joints
Located between the superior facet of one vertebra and the inferior facet of the vertebrae (refer to the preceding image). Approximately 16% of the body's load is absorbed by these joints. If they are poorly aligned, or under chronic extra stress, they can be the location of common back pain.
Intervertebral joints
Intervertebral joint ( inter~ in between, vetebral~vertebra): This joint is found between the vertebral bodies of the vertebrae. 84% of the body's load should be absorbed here if well aligned.
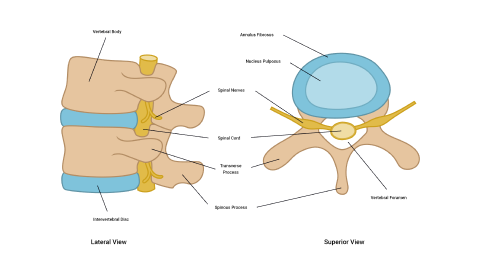
Intervertebral discs
There are 3 joints between each vertebra - 2 facet joints and 1 inter-vertebral joint. Each intervertebral joint is separated by an intervertebral disc. Together as a team, the intervertebral discs and the vertebra form the vertebral column.
The intervertebral discs are comprised of 2 main components:
- The annulus fibrosus: The annulus fibrosus are tough fibro-cartilage rings. These are very strong under compression, but susceptible to torsional (twisting) stress.
- The nucleus pulposus: The nucleus pulposus is mainly made up of water (90%) and provides shock absorption like water-filled cushions.
Did you know?
Disc height changes over the course of a day due to axial loading. This results in us being taller in the morning than at night!
Watch
Enjoy this short yet stunning 3D video of the human skeleton looking at the different regions of the spine.
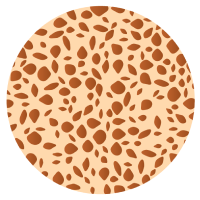
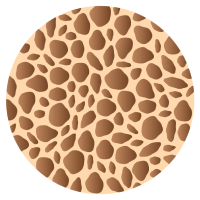
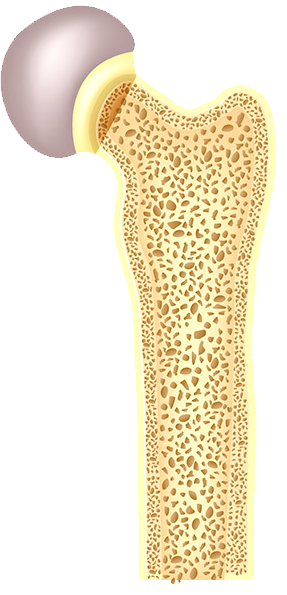
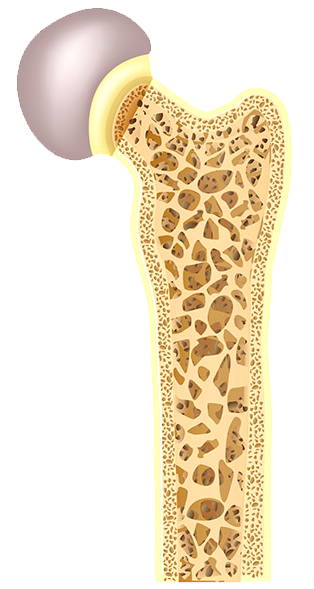
The term 'bone mineral density' refers to the amount of bone mineral (mainly calcium) present in a bone. Bones with high mineral density are stronger, can withstand greater forces, and are less likely to fracture. Bones with low mineral density are weaker and more prone to fracture under stress.
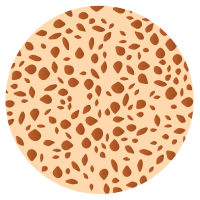
Normal bone
Osteopenia
Osteoporosis
Severe Osteoporosis
Factors contributing to bone density
3 factors are critical in developing bone mineral density:
- Sex hormones: Testosterone and estrogen hormones (among others) stimulate bone deposits.
- Nutrition: Adequate food intake, including regular consumption of calcium.
- Loaded exercise: This refers to exercise that places repetitive stress on bones to encourage bones to adapt (strengthen).
How to enhance bone mineral density
We want to use exercise to improve bone strength via increasing bone mineral density.

Research has clearly shown a direct relationship between exercise and bone health. But not all exercise affects bone the same when it comes to building strong, healthy bones or preventing poor bone health, such as osteoporosis.
Loaded exercise is the key to maintaining bone mineral density and bone health.
Loaded exercise
The term 'loaded' refers to an activity that places at least body weight on bones, such as running, dancing, low-impact aerobics, or skipping. These are weight-bearing aerobic activities on your feet, where bones are supporting your weight.
When placed under mechanical stress, bone tissue becomes stronger. This is due to an increased rate of bone production, which occurs quicker than the bone reabsorption (breakdown) phase of the bone remodelling process. Activities such as jumping and running stimulate the process of bone remodelling more effectively and efficiently than activities such as low-weight-bearing activities (e.g., cycling and water-based activities) because these do not elicit the same response in terms of bone density.
To stimulate bone growth, the exercise must create stress on the bone.
People who do regular loaded physical activity produce denser and more mineralised bones when compared with sedentary individuals.
Occupations and sports that are predominantly one-arm dominant (e.g., tennis players, baseball pitchers, or cricket bowlers) result in more mineralised bones on the dominant side.
Resistance exercises can also strengthen bones, e.g. weightlifting, free weights, body weight, and exercises with resistance bands.
It is also important to include exercises for stability and balance. Improved stability and balance will help prevent falls, and help muscles work together to keep the body stable.
Nutrition
The other key factor in bone health is nutrition. You must provide your body with enough essential minerals to support bone growth and maintenance.
Watch
Dr Jen Gunter explains what you can do for strong, healthy bones in this short video.
Factors to consider when selecting exercises for bone mineral density
3 characteristics of exercises that have the largest impact on increased bone density are:
- Strain magnitude
- Strain rate
- Strain frequency
Strain magnitude
The amount of stress placed on the bones.
This is higher in exercises such as gymnastics and weightlifting, where the force or impact of the exercise is greatest.
Strain rate
This is the velocity over which the strain is placed on the bones.
This is higher in exercises such as jumping or plyometrics, where the rate at which the impact is felt is high.
Strain frequency
This is how often strain is placed on bones during the course of an activity.
This is higher in exercises such as running, where the impact on the bones frequently occurs during the exercise session.
Order of importance
Strain magnitude is the most important of the three factors for bone density. Velocity is the next most important factor, followed by frequency.
- Strain magnitude
- Strain rate (velocity)
- Strain frequency
Cross-training
Athletes involved in sports that have low strain magnitude (such as water-based sports and cycling) would benefit from a form of cross-training that is higher in strain magnitude. E.g., a water polo player may benefit from doing some weight training to ensure their bone density is maintained.
Cross-training is a form of training that typically incorporates multiple training systems through various exercises to develop and enhance overall performance.
It is important to have the correct balance of these when designing training programmes. Consider a thorough pre-screening session when working with new and existing clients.
It’s important in developing a safe and effective exercise programme design, to take the time to sit down with your client, take them through a pre-screening questionnaire and consider providing an example. Break the ice with the client to gain a thorough (but not intrusive) medical history to ensure you are aware of any potential risks you can avoid, by selecting the correct exercise and exercise frequency. This comes under the mindset of programme design and pre-screening. We'll look at this in greater detail in future modules.
If only little stress is placed on bones, bones will demineralise.
Use it or lose it!
Bone demineralisation can happen for a variety of reasons:
- Sedentary lifestyle
- Low-impact endurance exercise
- Becoming bedridden
Nutritional deficiency can also contribute.
Normal bone
Osteopenia
Bone wasting conditions
Bone growth is dependent on sex hormones. As the levels of these hormones reduce with age, bone mineralisation decreases, and bone atrophy (wasting) can start to occur.
All of us will eventually suffer from osteopenia which is a natural de-mineralisation of bones as we get older.
If this gets to the point where daily living is compromised, it is known as osteoporosis.
Osteoporosis is a disease where new bone generation does not keep up with old bone removal. The bones become weak and brittle and more at risk of breaking. Risk factors for developing osteoporosis include:
- being over the age of 50.
- being physically inactive.
- having low levels of micronutrients such as calcium and vitamin D.
