As you observe your client's functional movement patterns, proceed along standard guidelines while seeking to identify possible joint mobility or movement restrictions in dynamic posture.
There are two types of variances that can affect posture:
-
Structural - Relates to the various components of the human body, otherwise known as anatomy. It is concerned with asking questions such as "What is that?" and "Where is it located?"
-
Functional - Relates to the correct operation or purpose of particular body parts, otherwise known as physiology. It is concerned with asking questions such as "What does it do?"
Poor posture triggers certain muscle imbalances that produce weak areas in the body, affecting functional movement (movement efficiency) and possibly causing pain, stiffness, and discomfort. It also increases the risk of falls and injury due to a reduction in core stability if local muscles are imbalanced. Early identification of posture-related structural and/or functional variances will help prevent client injury and enable the start of corrective applications.
Some common types of posture-related variances are outlined below.
Muscle tone is defined as the unconscious low-level contraction of muscles whilst in a state of rest. Essentially it is the retaining of firmness while in the relaxed state. Certain muscles create recognisable characteristics whilst in this formation for example the pectoral muscles (pecs), abdominal muscles (abs/six-pack), and the biceps.
As a general rule the human body is supposed to be symmetrical, and this also applies to the development of muscle tone. Balanced muscle tone helps to maintain balance and thus prevent injury, aids in maintaining good posture, and it is also more visually appealing.
Asymmetrical muscle tone is when certain muscles are overdeveloped at the expense of others, this can occur on two levels:
-
Micro-level - Between opposing muscles. For example the hamstring and the quadriceps, or the bicep and the tricep.
-
Macro-level - Between larger muscle groups. For example when a person focusses on their upper body muscles at the expense of their lower body muscles.
Side-effects of asymmetrical muscle tone can include:
-
Stiffness and difficulty moving.
-
Uneven muscle appearance (ie. crooked or misaligned abdominal muscles).
-
Improper alignment of the spine causing one side of the body to be higher than the other. Most often recognised by one shoulder being higher than the other.
-
Limited flexibility because of a problem with the joint, stiffness of the muscle, and swelling of tissue around the joint. Muscle hypertrophy and tissue degeneration are consequences if causes are not addressed.
-
Limited function occurring when a muscle doesn't work or move normally. With decreased muscle function, wasting away of the muscle occurs creating weakness. Limited functionality is often temporary, associated with short-term disabling conditions such as broken bones or dislocations, however, it can result from more long-term neurological conditions such as neuropathy, polio, paralysis, and stroke.
-
Increased risk of falls and injury due to a reduction of core stability from the local muscles.
Asymmetrical muscle tone can be caused by:
-
Prior injury.
-
Poor exercise form.
-
Isolation exercises.
-
Some types of muscle tone conditions such as Hypertonia (increased muscle tone).
One method to avoid non-genetic asymmetrical muscle tone is to focus on whole-body conditioning, the concept of 'leg days' and 'arm days' is not recommended as it trains these muscles to act in isolation.
In the case of genetic or acquired muscle tone conditions that are unrelated to the amount of exercise or techniques other treatments may be required such as muscle relaxing medications and physiotherapy. A referral to an appropriate medical professional will be required or if the condition has already been diagnosed then any exercise must be coordinated with the recommendations of the client's treating practicioner.
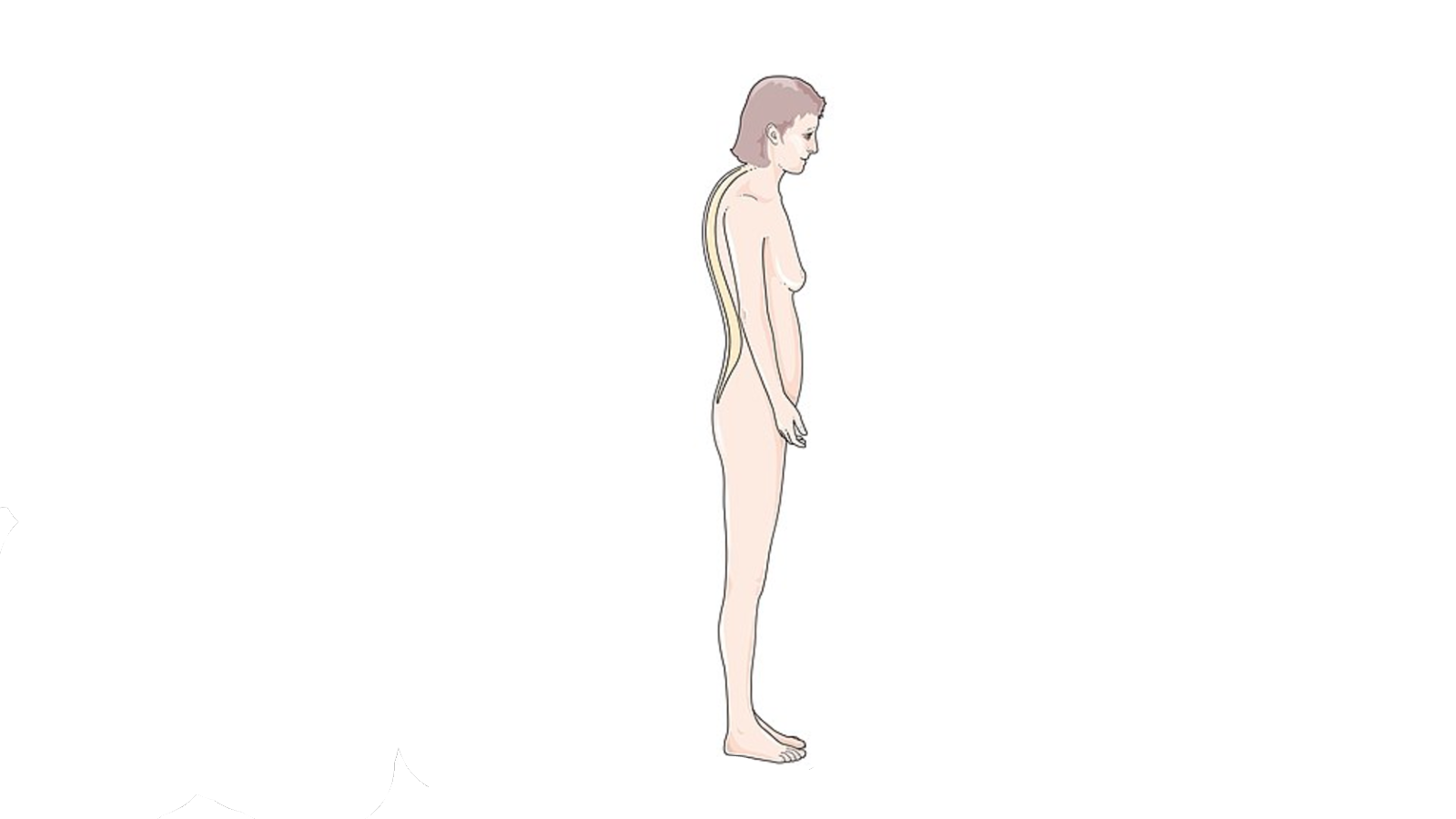
In keeping with the line of gravity, the head forms part of the imaginary plumb line which runs down the body, intersecting several key joints and other body reference points. The intersecting points include the earlobe before the line travels downward towards the shoulder joint and beyond. Therefore if the head is misaligned it disrupts this plumb line and causes various posture-related conditions and pain.
The two main conditions associated with incorrect head alignment are:
This condition is part of a larger condition known as Cervical Dystonia, it is observed by a visible tilting and/or spasmodic flexions of the head in a variety of positions or a combination of one or more of the positions:
-
Lateralcollis - The head is tilted laterally (toward the side) toward either shoulder.
-
Rotational torticollis - The head and subsequently the face, is naturally positioned or faces in a direction away from the midline (either to the left or the right). The person is usually able to move their head into the other positions however their comfortable resting state is in the rotated state.
-
Antercollis - Forward flexions of the head and neck.
-
Retrocollis - Hyperextension of the head and neck backward.
Lateralcollis can cause physical pain and discomfort including headaches and neck pain.
The broader condition of Cervical Dystonia is usually congenital (present from birth) and thus is diagnosed during infancy or childhood. It can also be acquired as a result of trauma, muscle imbalance, other conditions and infections, or as a side effect from certain drugs.
The acquired variety, particularly Lateralcollis, sometimes rectifies itself with little or no treatment or through changes to posture-related activities such as computer use or sleeping position. Physiotherapy and pain-relieving medications can also help to alleviate the symptoms of both congenital and acquired Lateralcollis.
The chin is angled forward and the ears are positioned forward of the shoulders.

Can also be caused by spending too much time looking down at hand-held devices or poorly placed computer screens.
Symptoms include:
-
A visibly forward placed head that is out of alignment with the rest of the body.
-
The client may complain of a heavy head (they may describe this as being similar to the weight of a bowling ball).
-
Tight back muscles.
-
Herniated spinal discs and other joint problems.
To observe forward head posture position the client against a wall then check their posture for the following:
-
The head, upper back and buttocks should all touch the wall.
-
The client’s ear lobes should be positioned above / inline with the clavicle (collarbone).
-
The chin should be pulled in, with the client looking straight ahead, and not up.
-
The shoulders should be back and not rounded.
If any of these observations deviate from the ideal positioning, your client may need corrective exercises for posture adjustment.
Examples of corrective exercises include:
-
Chin tucks - Reverse motion of the chin and subsequently the head. Using two fingers on the chin the client should gently push the head backwards. This can be a difficult and awkward exercise for some people especially initially if the movement causes pain then it should be avoided.
-
W exercise - From a starting position of having the arms bent at the elbows and the forearm facing outward (to form a W shape) have the client gently squeeze their shoulder blades together and down. Complete five repetitions holding each one five seconds.
-
YWLT exercise - Starting position should assume a Y position by placing the arms up, pull the arms back as far as possible and hold for two deep breaths. Move arms down into the W position as per the previous exercise, pull the arms back as far as possible and hold for two deep breaths. Then move the arms down so the elbows are at right angles forming an L shape, pull the arms back as far as possible so that the shoulder blades are squeezed. Finally, straighten elbows and extend arms into a T position, hold arms back as far as possible and hold for two breaths.
The forward head corrective exercises are demonstrated in the below video:
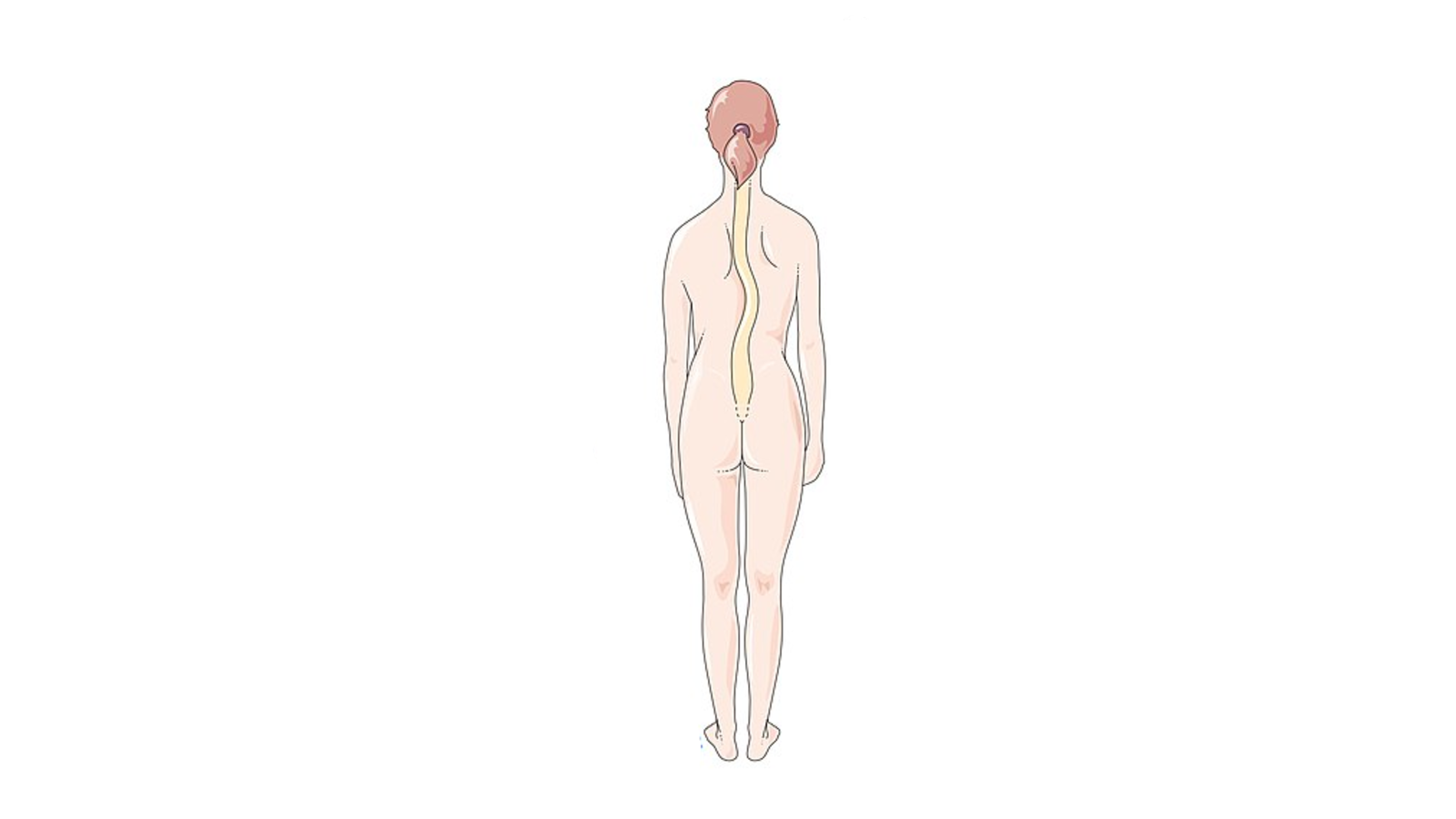
The spine naturally curves in a gentle S shape from the top to the bottom, however, these curves can present in a distored state in some people.
Misalignments of the spinal curvature can place undue pressure on supporting neck and back muscles, predisposing the individual to pain and a higher likelihood of:
-
Muscle strain.
-
Joint degeneration.
-
Broken bones and other fall-related injuries.
Three common types of spinal curvature are:
Unusually large, inward arch of the lower back just above the buttocks. This condition, also known as swayback, can cause lower back pain. Lordosis can also present in a decreased state whereby the lower spine loses some of its normal curvature, this is known as flatback syndrome.
Treatment options include:
-
Physical therapy.
-
Weight loss (if applicable).
-
Braces, often used in children and teenagers as they are most effective when the spine is still growing.
-
Surgery (for extreme circumstancess).
-
Medication and vitamin supplements.
.png)
Excessive outward curvature of the thoracic spine although it can also affect the cervical spine. This condition, also known as hunch-back, can cause severe deformity, nerve problems, and chronic pain.
Treatment options include:
-
Physical therapy.
-
Braces, often used in children and teenagers as they are most effective when the spine is still growing.
-
Surgery (for extreme circumstances).
-
Medication.
A sideways curvature of the spine, mostly occurring during the growth spurt just before puberty. Severe cases of this condition can be very disabling, reducing the chest cavity and making it difficult for the lungs to function properly. It also results in an asymmetrical posture.
Treatment options include:
-
Braces, often used in children and teenagers as they are most effective when the spine is still growing.
-
Surgery (for extreme circumstances).
The scapula, also known as the shoulder blade, is triangular in shape and provides a joining force between the clavicle (collarbone) and the humerus (upper arm bone). These three bones form the shoulder.
The body has two scapulas, one on the left side of the body and the other on the right side. The purpose of the scapula is to provide a stabilising force for other bones in the shoulder area and also to assist with the movement of the pectoral girdle and chest muscles.

There are four joints associated with the shoulder and therefore the scapula:
-
Scapulothoracic Joint (ST) - Where the scapula joins the thorax (collectively the thoracic spine, ribcage, and the sternum). Not a true joint because it is not connected by ligaments.
-
Acromioclavicular Joint (AC) - Where the scapula joins the clavicle via the acromion process. It is a gliding synovial joint, allowing bones to move from side to side. This joint helps facilitate raising the arm over the head.
-
Glenohumeral Joint - Where the scapula joins the humerus. It is a ball and socket style joint, allowing rotation. This is considered to be the main joint of the shoulder allowing for circular movement of the arm.
-
Sternoclavicular Joint (SC) - Where the clavicle joins the sternum. Together with the AC & ST joints it helps provide movement to the scapula. It is a gliding synovial joint, allowing bones to move from side to side. This joint helps facilitate the action of shrugging, extending the arm behind the body, and moving the shoulders forward or backward.
There are six types of movements of the scapula, grouped into pairs:
-
Elevation & Depression - Raising (elevation) and lowering (depression) of the scapular. The action of shrugging the shoulders utilises elevation and depression.
-
Protraction & Retraction - Movement of the scapula away from the midline of the body (protraction) and toward the midline of the body (retraction). The action of throwing the shoulder back and pinching the shoulder blades together utilises protraction and retraction.
-
Downward & Upward Rotation - Rotating movement of the humerus (upper arm). The action of extending / raising the arm outward from the body (upward rotation) and then lowering it (downward rotation).
The following video provides an excellent animation of the various movements of the scapula.
There are certain conditions which affect the scapula from a postural perspective:
The scapula normally sits flat against the back of the chest wall. In the case of a winged scapula it is visibly protruding out on one side and the client may have a drooping shoulder.
This condition causes a significant amount of pain and results in weakness and reduced mobility of the shoulder joint particularly in pressing motions. This weakness can lead to other injuries if the client attempts to rely upon the weakened scapula and it fails.
Often caused by nerve damage to one of three nerves that control the muscles of the arms, back, and neck:
-
Long Thoracic Nerve - Which controls the Serratus Anterior Muscle. This results in Medial Winging and is the more common variety of this condition.
-
Dorsal Scapular Nerve - Which controls the Rhomboid Muscle.
-
Spinal Accessory Nerve - Which controls the Trapezius Muscle
Nerve damage can be the result of an injury, traumatic or repetitive strain, or in some cases surgery such as rib resections or a mastectomy. Treatment options vary depending on which nerve has been damaged thus causing the condition, however most treatments are nonsurgical and involve regular physical therapy or targetted corrective exercises such as:
-
Wall scapula press - Both arms are pressed against a wall and with straight elbows the shoulder and back muscles are used to move the upper body towards the wall.
-
One-armed wall scapular press - A progression of the wall scapula press whereby one arm is held behind the back and the pressing is done using one arm and then alternated to the other arm.
-
Floor scapular press - Positioned on knees and hands the body is gently lowered toward the floor and raised again.
-
Four-point and isometric holds - A progression of the floor scapular press whereby one arm is extended in front of the body and the lowering is done using one arm and then alternated to the other arm.
The following video provides a demonstration of these corrective exercises.
Tipping is a normal motion of the shoulder / scapula, occurring when a person raises or lowers their arm. However, in some people the scapula is tipped or tilted forward (anterior tipping/tilting), this creates a block to the action of the acromioclavicular joint and preventing full verticle alignment of the raised arm and causing pain.
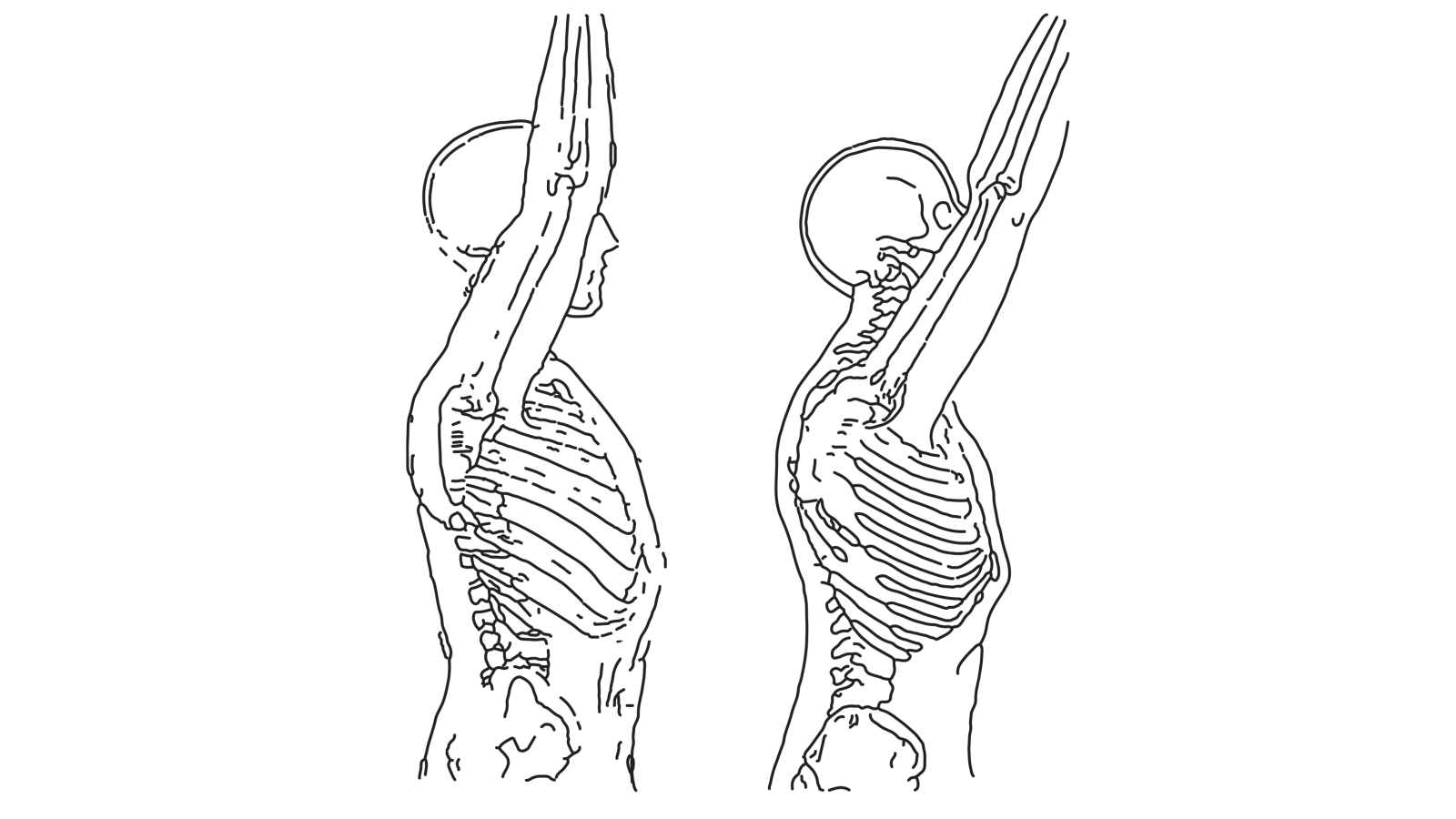
This condition, which is also known as Scapula Dyskinesia or SICK Scapular Syndrome, is an overuse or repetitive strain syndrome caused by a weak lower trapezius muscle and a tight pectoralis minor muscle.
Treatment options usually involve targetted physical therapy exercises focussing on raising and lowering the arm or overhead pulls.
Another common postural condition that affects the shoulder region is known as rounded shoulders. According to the NHS website (a united kingdom site), this condition is typically caused by incorrect posture, muscle imbalances, or too much emphasis on certain exercises such as the chest area whilst neglecting the upper back.
This condition can be improved or even fully corrected by the application of specific exercises targetting the muscle imbalance:
-
Thoracic extensions.
-
Band over-and-backs.
-
Band pull-apart.
-
Banded Y-raise.
-
Push-up plus.
For information on rounded shoulders including corrective exercises instructions and images, refer to this Built With Science article which explores this topic in detail.
The pelvis is a basin shaped structure that supports the spinal column and protects the abdominal and reproductive organs. It supports the upper body when sitting and transfers this weight to the lower limbs when standing.
Whilst the male and female pelvis structurs consist of the same bones and joints they differ slightly in size and shape, owing to the difference in reproductive organs and their function.
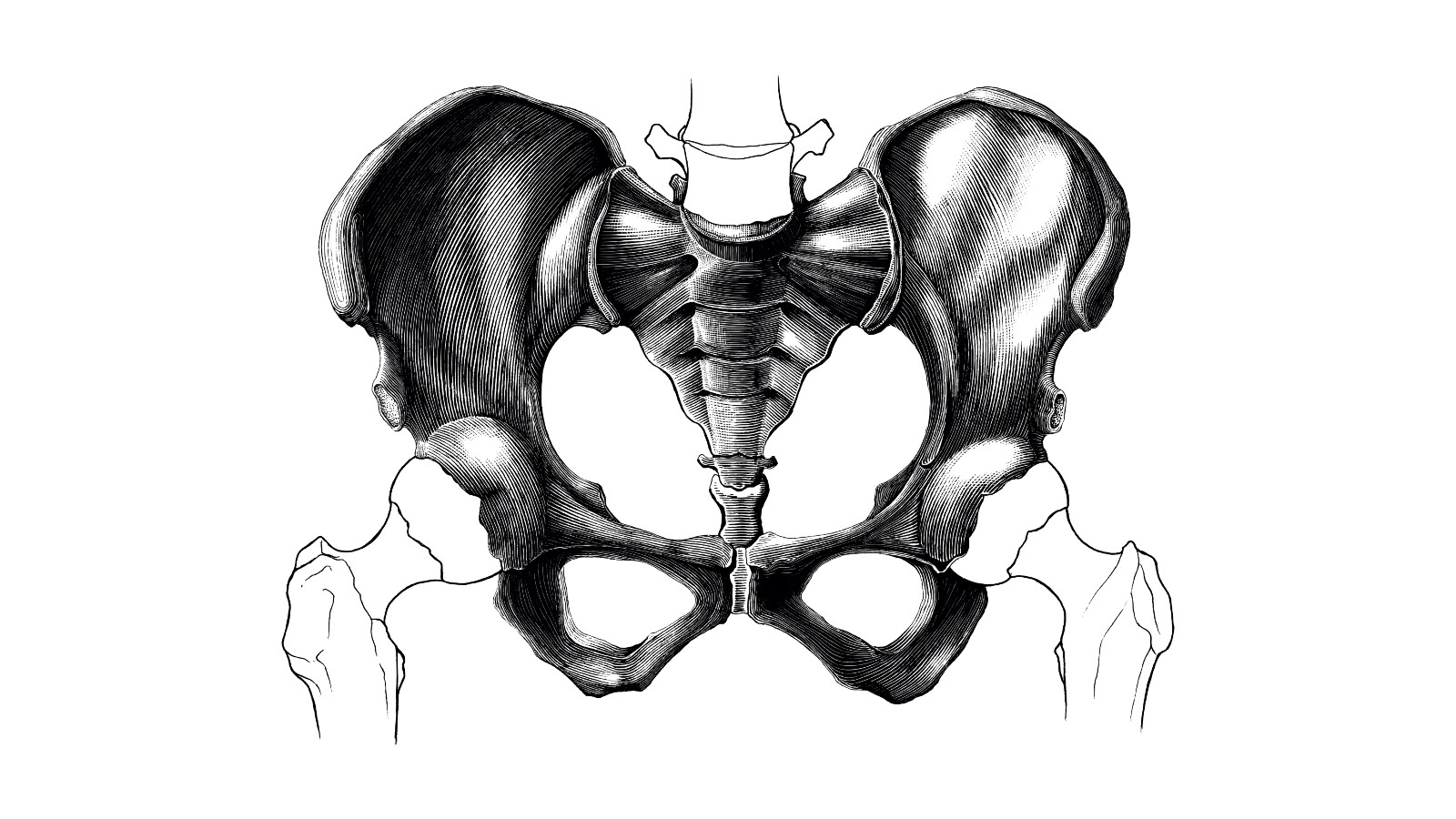
There are certain conditions which affect the pelvis from a postural perspective:
The pelvis can become misaligned, tilted / rotated, for a number of reasons, most commonly due to:
-
Spending an excessive amount of time in a sitting position because the hips are in an extended state of flexion.
-
Certain activities which favour one side of the body over the other.
There are three types of misalignments:
The pelvis is tilted/rotated forward forcing the spine to curve.
Inactivity and sedentatry lifestyles are the predominant causes, causing weakened hip flexors and weakened abdominal, gluteal, hamstrings and quadricep muscles. Genetics can also play a part, especially in regards to inherited bone structure issues.
Symptoms include:
-
Lower back pain, can be experienced as an acute injury or as a more chronic ache.
-
Hip and knee pain.
-
Forced inward leg and knee rotations.
The front of the pelvis tilts/rotates up and back, while the bottom of the pelvis tilts/rotates under the body. Essentially the opposite of the anterior tilt.
Incorrect sitting position, ie. slouching, is one of the most common causes. Tight hamstring and gluteal muscles can also be a cause as they pull the pelvis out of its normal alignment.
Symptoms include:
-
Disc problems.
-
Sciatica.
-
Constant lower back pain.
-
Knee, hip and ankle problems.
-
Headaches.
-
Neck problems.
-
Feet may appear to splay outward.
-
The lower back will be flat and without an arch.
-
The upper body will have a bigger hunch than a person with an anterior tilt because the spine compensates.
Where the pelvis tilts/rotates sideways causing one hip to be aligned higher than the other.
Conditions such as scoliosis and leg length discrepency. Athletes that perform asymmetrical sports such as tennis, golf, baseball and cricket may also develop lateral pelvic tilt/rotation over time as the muscles in their favoured or active side become more developed.
Symptoms include:
-
Pain.
-
Balance issues.
-
Noticeably misaligned hip bones with one higher than the other.
There are a variety of stretches and specific exercises that can help to correct pelvic tilts and rotations, including:
-
Glute Bridge - Client lays on the floor, with their knees bent and feet flat on the ground. Hips are then lifted off the ground until the knees, hips, and shoulders form a straight line. Glutes are then squeezed hard and abdominal muscles are tensed so tha the back is not overextended.
-
Lunge - Client takes a big step forward (can also be backward or to the side) with the right leg shifting their weight forward so the heel hits the floor first. They then lower their body until the right thigh is parallel to the floor and the right shin is vertical. They should press into the right heel to return to the starting position and then repeat on the other side.
-
Spit squat - Similar to a standard lunge except that the feet are static during the movement rather than performing an active stepping motion with each repetition.
-
Hip adduction and abduction - Hip adduction is the movement of the leg towards the midline of the body and hip abduction is the movement of the leg away from the midline. Side lying leg lifts are an example of exercises that are working the hip abductors. Hip drops using a raised step can also benefit a weak hip abductor.
-
Proper Plank - Performed on the hands or elbows, the focus is to keep the abdominal muscles braced. See video below for a detailed demonstration.
However in extreme cases (ie. when the tilt or rotation is caused by other spinal or structural conditions) intervention may be required in the form of braces or surgery.
A normally aligned knee has a load-bearing axis on a line that runs down the middle of the leg, through the hip, knee and ankle.
When the knee is not perfectly aligned, it is known as either Genu Valgum (knock-knee) or Genus Varum (bow-leg) alignment. There is a link between knee malalignment and knee osteoarthritis.
.png)
- Genu Valgum alignment (knock knee) shifts the load-bearing axis to the outside causing a large gap between the feet when the client is standing with their knees together. Common amongst younger children, although it usually corrects itself. Whilst it doesn't usually cause other problems it can cause knee pain, a limp or difficulty walking if the occurrence is severe enough.
-
Genu Varum alignment (bowlegs) evident by the knees staying wide apart even when the client is standing with their feet and ankles together. The client is at risk of knee osteoarthritis, muscular imbalance, poor posture, as well as difficulty with walking and running. Overweight clients are substantially at risk.
These types of structural deformaties often require surgery to correct.
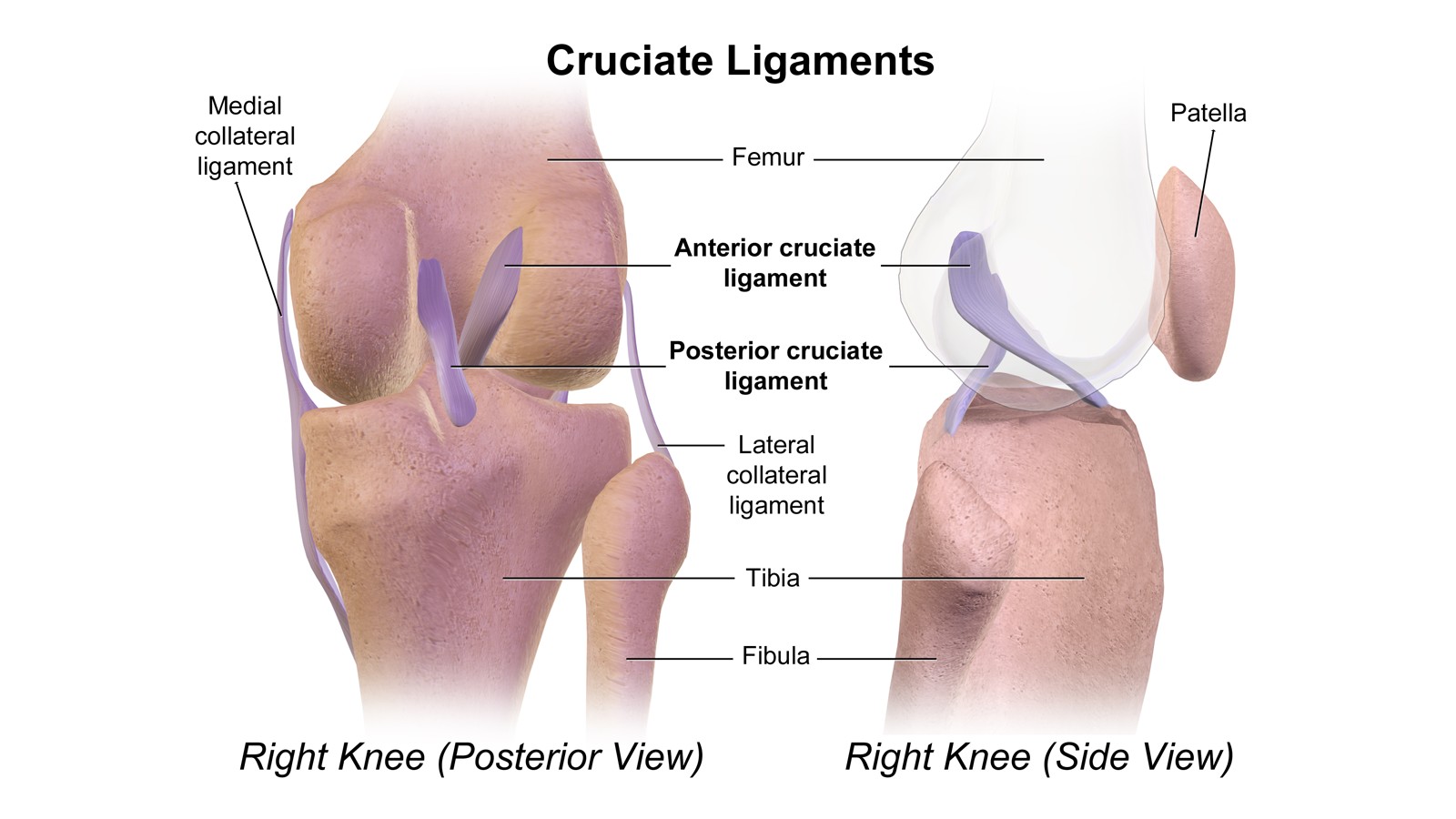
The knee joint is a hinge joint and it can be injured if forced to extend beyond its normal range of motion, this type of injury is known as Hyperextension of the knee/s. The four major ligaments of the knee joint, operating in pairs to minimise certain movements and provide stability:
-
Medial collateral ligament (MCL) & Lateral collateral ligament (LCL) - Located on the inside of the knee (MCL) and the outside (LCL). The MCL connects the femur (thighbone) to the tibia (shin bone) while the LCL connects the femur to the fibula (a slim bone that runs down the outside of the calf muscle), Their main function is to minimise side-to-side movement of the knee joint.
-
Anterior cruciate ligament (ACL) & Posterior cruciate ligament (PCL) - Attach the knee to the femur (thigh bone) to the tibia (shin bone) crisscrossing diagonally over each other. Their main function is to stabilise the knee joint, especially during movement that involves sudden change of motion or impact.
If either of these ligaments is hyperextended the resulting symptoms will include swelling, reduced range of motion, sharp localised pain, and instability on the affected leg.
These ligaments, along with certain tendons, also help to maintain the natural position of the patella (kneecap). The patella can become misaligned or rotated most commonly as a result of trauma (severe blow to the knee), incorrect posture, or muscle imbalance. This condition is known as Patellar Tracking Disorder or in severe cases it results in a full dislocation.
Apart from trauma other causes of Patellar Tracking Disorder include:
-
Improper footwear.
-
Being overweight.
-
Weak quadricep muscles.
-
Improper form or techniques whilst exercising resulting in the outer region of the thigh being stronger than the inner thigh.
-
Sports that require excessive knee bending, jumping, or squatting.
-
Running, especially on hills.
Misalignment of the kneecap usually results in pain and discomfort as well as audible sensations such as popping, catching, or grinding noises when the leg is straightened or bent. Treatment options include the application of ice to relieve acute pain and swelling, over the counter pain medication, and knee support aids.
There are six types of movements of the ankle joint, grouped into pairs:
-
Dorsiflexion and Plantarflexion - Lifting the forward portion of the foot upwards (dorsiflexion) and lowering it downwards (plantarflexion).
-
Inversion and Eversion - Rolling the sole of the foot to face medially (inversion) and laterally (eversion).
-
Medial and Lateral Rotation - Pivotting of the foot medially (internal rotation) and laterally (external rotation)
Internal rotation of the leg produces a pronated foot (leaning inward). External rotation of the leg produces supination (leaning outward) of the foot.
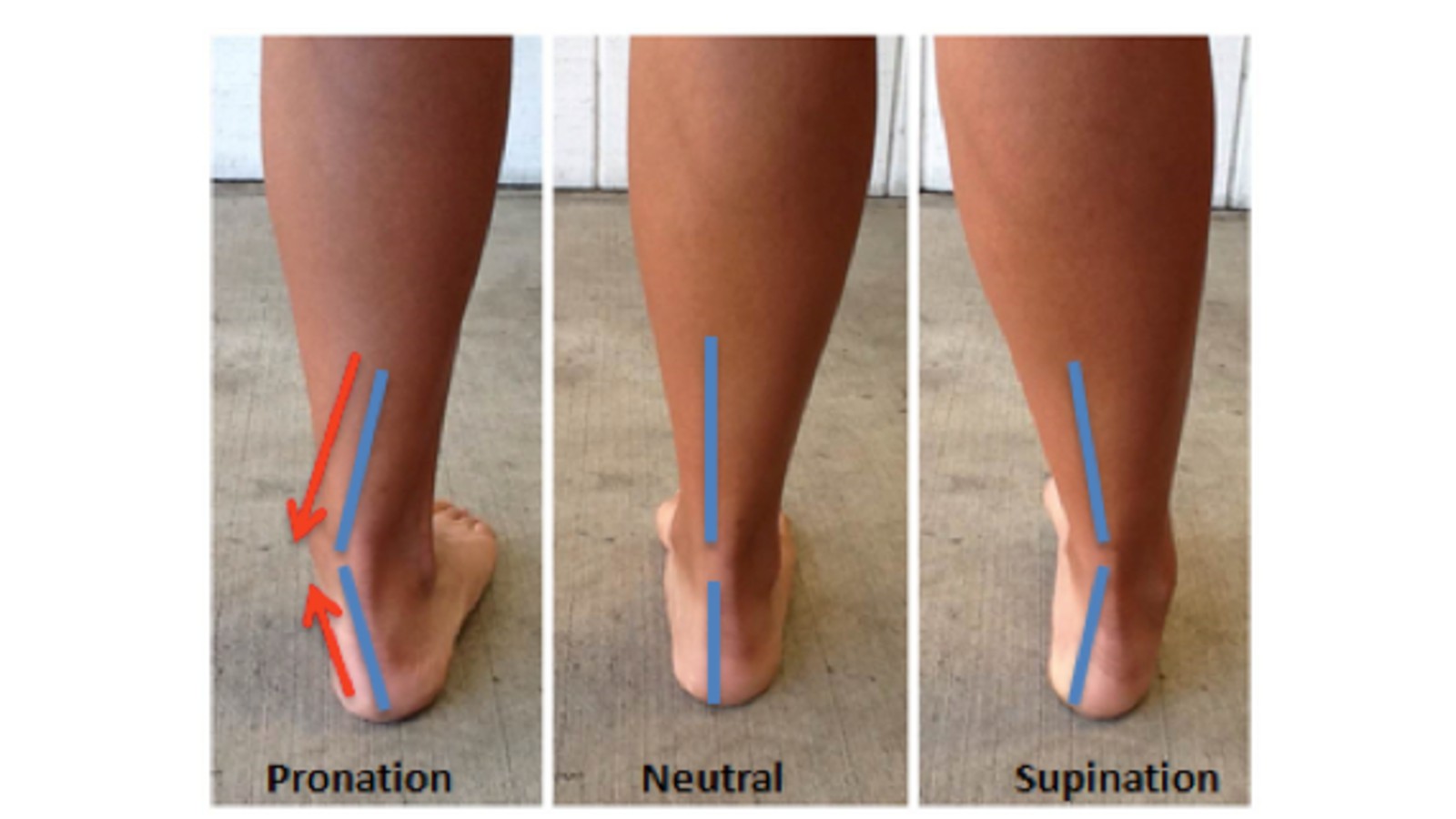
Pronation of the foot can result in injuries or conditions such as:
-
Shin splints.
-
Bunions.
-
Heel pain.
Supination of the foot can result in injuries or conditions such as:
-
Ankle sprains (from falls).
-
Calluses or bunions.
-
Hammertoes or clawed toes.
-
Plantar fasciitis.
-
Shin splints.
-
Stress fractures.
-
A general weakness in the foot or ankle that worsens when running, walking or standing for long periods.
Both of these conditions can be corrected by the use of orthotics (specailised foot wear or shoe inserts) and can be prescribed/recommended by a medical professional or a podiatrist.
These conditions and variances can sometimes be observed or preliminarily diagnosed through a variety of assessments. Two common types of assessments include:
During the examination, measure how long it takes the client to rise to a standing position from the supine (laying down) position on a mat.
Observe the degree to which the hands are used from supine to the sitting position and then onto standing. Excessive reliance upon the hands to maintain stability, balance, and coordination may indicate potentially weak knees or weak hip extensors.
Gait assessments can vary depending on who is undertaking them and for what purpose. There are different types of assessment for improving posture and fitness related gait issues vs. diagnosing more serious types of functional disorders.
Basic fitness gait assessments can include observation of:
-
Feet - Do they rotate internally or externally when walking?
-
Weight - Is body weight evenly distributed?
-
Arm swing - Is it consistant from side to side?
-
Gait speed - Is the walking pace typical?
-
Direction and Balance - Do they require assistance to walk in a straight line or to maintain balance?
-
Recognisable gait disorders - You do not need to be an expert in the various gait disorders but should be able to recognise when something is not quite right. Things to look for include: Shuffling; Stooped head; Stumbling/staggering gait; Waddling; Dragging legs/feet. (Note: these signs will not all occur simultaneously as they are symptoms of different types of disorders).
-
Jogging / Running on a treadmill - Ankle and knee rotation, foot placement and landing technique.
More complex gait assessments will ask the client or patient to walk on their toes, heels, a straight line (toe to heel), and to stand with their feet together and eyes closed. This type of assessment, usually conducted by a medical or allied health professional such as an osteopath, physiotherapist, or podiatrist, is looking for gait impairment caused by neurological impairments which may affect gait and balance.
It is important to note that gait can change depending on shoe choice, surface, and the speed at which the gait is undertaken. If these factors have been taken into consideration and you still suspect a problem with a client's gait then referral to a medical or allied health professional is the best course of action. Physical therapy and other corrections such as shoe inserts can improve basic gait disorders.

