In this section you will learn to: Receive, interpret, and document written and oral instructions using medical terminology, interpret abbreviations for specialised medical terminology and interpret and adhere to the policies and procedures of the workplace.
Supplementary materials relevant to this section:
- Reading A: Building Medical Terms from Word Parts
- Reading B: Abbreviations in a Healthcare Facility
- Reading C: Health Conditions Prevalence
- Reading D: How Health Insurance Works

Words
When working in a medical environment, it is vital that you are familiar with medical terminology, including being able to understand, interpret, and use them appropriately. Medical terminologies are usually the words or terms that describes body organs, systems, functions, body locations, diseases, diagnostic imaging, clinical procedures, and more. It is important that as a practice manager, you have a good command of the medical terminology to communicate effectively and accurately between patients, fellow workers, and health professionals.
Depending on the specific medical environment you work in, there may be additional industry-specific terminology that would be too vast to be covered in this module. Take note that throughout this module, we will be using the term ‘patients’ to refer to service users, though keep in mind that it can be used interchangeably with other terms such as ‘clients’ and ‘consumers’. When reading this module, keep in mind that your role description may not include some of the tasks or procedures mentioned. However, it is still good practice for you to be familiar with them, as you may need to take over these responsibilities during a busy day or when someone’s away.
Word parts
In this section, we will look at general terminology universal to the healthcare and medical industries. Before diving into the medical terminology, let us first look at how to understand and interpret most of the words. While these words may appear scary initially due to its high technicality and complexity, when you understand the word parts and how the word is formed, you will be able to interpret and understand the word better. Typically, medical terminology is usually made up of the following three components (Brown, 2016; Gow & Christensen, 2023):
- Word root – the foundation of a word and usually consists of the core meaning behind any term. Typically attached with a prefix and/or a suffix to give the term the exact meaning. Word roots are usually derived from Greek or Latin and may be used for a particular cell, tissue, or organ. E.g., the word root nephr means kidney and is derived from nephros, which is kidney in Greek.
- Prefix – usually used before the word root to convey a certain condition to enhance the meaning of the word. E.g., a- means without or lack of, and asymptomatic means without or lack of any symptoms
- Suffix – usually attached to the end of a wood root with a combining vowel. It is usually used to provide further information, such as a procedure or disease. E.g., -ectomy has a meaning of surgical removal, hence nephrectomy means the surgical removal of a kidney.
The way to decipher and understand medical terminology is to break the term into different word parts. You would first look at the suffix and the prefix, and then the word root. While most medical terminologies have all three-word parts, some of the terms might not; some terms may lack a prefix, or a suffix while some terms may have two-word roots. If any part of a word changes, the meaning of the term would be changed too. In addition to the spelling, the pronunciation of the word is also crucial to convey the accurate information, as some words are spelled differently but sound alike. For example, phasia (fay-zee-ah) means speech while phagia (fay-jee-ah), means eating or swallowing (Cross & McWay, 2020, p.10). Refer to the table below to look at how different word parts can be combined to become a medical term (Cross & McWay, 2020, p.12):
Table 2-1 Parts of Medical Term
| Word Parts | Examples | Medical Terms |
|---|---|---|
| prefix + word root | anti- (prefix meaning against) + thyroid (root word for thyroid gland) |
antithyroid
|
| word root + suffix | gastr (word root for stomach) + -ic (suffix meaning pertaining to) |
gastric
|
| combining form (word root + combining vowel) + suffix | cardi (root word for heart) + /o (a combining vowel) + -logy (suffix meaning study of) |
cardiology
|
| prefix + suffix | an- (prefix meaning no, without) + -emia (suffix meaning blood) |
anemia
|
| prefix + root word + suffix | epi- (prefix meaning above, over) + gastr (root word for stomach) + -algia (suffix meaning pain) |
epigastralgia
|
| compound word + suffix | ot/o (root word for ear) + rhin/o (root word for nose) + laryng/o (root word for throat or larynx) + -logy (suffix meaning study of) |
otorhinolaryngology
|
*Two or more root words connected with a combining vowel.
Now that you have a better idea of the different word parts, let us look at some common root words, suffixes, and prefixes that you would most likely come across when working in a medical environment (adapted from Nath & Lindsley, 2019; pp. 6-8; Wingerd, 2019, p. 15).
| Word root/Combining Vowel | Definition |
|---|---|
| append/o, appendic/o | appendix |
| arthr/o | joint |
| cardi/o | heart |
| cerebr/o | brain, cerebrum |
| dermo/o/ato | skin |
| gastr/o | stomach |
| gen/o | origin, cause, formation |
| ger/o/onto | old age |
| hem/a/ato | blood |
| muscul/o | muscle |
| natal | birth; born |
| neur/o | nerve |
| os/teo | bone |
| path/o | disease |
| ped/ia | child |
| proct/o | rectum; anus |
| psych/o | mind |
| rhin/o | nose |
| skelet/o | skeleton |
| vas/o | vessels |
Prefix Definition anti- against, opposite of brady- slow endo- within epi- upon, over, above, on top micro- small neo- new peri- around post- after pre- to come before
| Suffixes | Definition |
|---|---|
| -al | adjective suffix; pertaining to |
| -algia | pain |
| -dynia | pain |
| -ectomy | surgical excision, removal |
| -emia | condition of blood |
| -gen, -genesisa | origin, cause, formation |
| -gram | a record or image |
| -ia | condition of |
| -iatry | treatment, specialty |
| -ic | adjective suffix; pertaining to |
| -itis | inflammation |
| -logist | one who studies |
| -logy | study of |
| -pathy | disease |
| -scope | viewing, an instrument used for viewing |
| -tic | adjective suffix; pertaining to |
Do note that the lists above are not exhaustive and depending on the specific medical setting you are working in, there are a set of more specified terms that you will come across frequently. Also, you should keep in mind that the resources you come across, including the readings in the Readings section of the module, may be in American spelling. You should use the correct spelling, i.e., the Australian/English spelling, especially when you are preparing and maintaining medical documents for work.
Reading A – Building Medical Terms from Word Parts
Reading A provides an introduction to how medical terminologies were formed, including its word roots, prefixes, and suffixes. The reading also looks at the pronunciation and spelling of these terms.
Abbreviations

Shortened words or initials can save time in writing medical. Shortened words or initials can save time in writing medical reports and case histories. We commonly use TV for television, Jr. for junior, F for Fahrenheit temperature readings, UV for ultraviolet, and Dr. for doctor. A few of the many medical abbreviations are mL for the metric measurement milliliter; dB for decibels, units of sound intensity; CA for cancer; hgb for hemoglobin; and ECG for electrocardiogram.
(Cohen & Jones, 2021, p. 8)
You will learn to realise that workers in a medical setting often use abbreviations when communicating information with others, especially with other workers. Using abbreviations can help convey information in a succinct manner while maintaining or increasing work efficiency. However, the downside of using abbreviations is that there is a risk of workers miscommunicating or getting confused about the information. This is because some medical workers are unfamiliar with and/or do not follow the standardised abbreviations used by most in the field. Therefore, it is vital that you familiarise yourself with the commonly used abbreviations in the field as well as ensure that the abbreviations you use are the standard ones or universally acceptable. Otherwise, the confusion may lead to slower work efficiency or may result in issues with insurance records and processing.
There are two types of abbreviations frequently used in the medical setting: phrase abbreviations and symbols. Phrase abbreviations, or more commonly called acronyms, are usually formed from the first letter of each word in a phrase. For example, BP stands for blood pressure and CNS stands for the central nervous system. On the other hand, symbols are more frequently used in case histories or medical records. For example, an upward arrow, ‘↑’ represents increase while the downward arrow ‘↓’ represents decrease. The table below shows a list of abbreviation and symbols that you may come across when working.
| Abbreviation/Symbol | Meaning |
|---|---|
| Ca/CA | Cancer |
| DOA | Date of admission/date of accident/dead on arrival |
| O/E | On examination |
| LA | Local Anaesthetic |
| GA | General Anaesthetic |
| ICU | Intensive Care Unit |
| STAT | Immediately |
| E&R | Examination and review (second opinion) |
| PD | Provisional diagnosis |
| CXR | Chest x-ray |
| S&S | Signs and symptoms |
| BCG | Bacille Calmette-Guérin (tuberculosis vaccine) |
| HRT | Hormone replacement theory |
| IVP | Intravenous pyelography |
| ung | Ointment |
| Ⓛ | Left |
| Ⓡ | Right |
| ♂ | Male |
| ♀ | Female |
Another important note to keep in mind is that when you are interpreting abbreviations, you should take into account the context, as there may be identical abbreviations but distinct meanings. For example, ED is usually used as an abbreviation for emergency department or erectile dysfunction. Similar to the word parts, it is impossible to list every single abbreviation here. Your workplace should have a handy list that includes the commonly used abbreviation in the workplace; make sure you familiarise yourself with the list and keep it nearby so you could interpret and understand these abbreviations quickly.
Reading B – Abbreviations in a Healthcare Facility
Reading B includes various abbreviations that are commonly used for the services in a healthcare facility. While you may not use all the abbreviations, it is still a good practice to familiarise yourself with them.
Common Medical Conditions

When working in a healthcare or medical setting, you will come across some common words when interacting with different people, e.g., with patients or your fellow workers. Most of the words listed below are relevant to the description of onset and/or nature of disease.
| Common Words | Meaning |
|---|---|
| Acute | Quick onset, short duration |
| Aetiology | Cause |
| Asymptomatic | No symptoms of disease |
| Benign | Not cancerous |
| Chronic | Long term |
| Congenital | Born with |
| Contagious | Easily transmitted from person to person |
| Epidemic | Outbreak of disease in particular region |
| Familial | Occurs frequently in families |
| Genetics | The science |
| Hereditary | Passed down from parents to children |
| Idiopathic | Unknown cause |
| Malignant | Cancerous |
| Oedema | Swelling |
| Pandemic | A disease or illness occurring worldwide |
| Prognosis | Likely outcome |
| Remission | No signs or symptoms of disease |
| Sign | Health issue that can be observed |
| Symptom | Subjective experience of a potential health issue |
| Syndrome | A set of signs and symptoms specific to a particular disease or disorder |
With a better understanding of these medical terminologies used to describe onset and nature of disease, we will look at some common medical conditions in Australia. According to the Australian Bureau of Statistics (ABS; 2022), nearly half of the people (46.6%) in Australia had at least one chronic condition, and over three quarters of Australians (78.6%) had at least on long-term health condition in 2020-2021. These figures reflect the fact that many Australians are experiencing at least one chronic condition and being familiar with the common chronic conditions in Australia is helpful in your role. According to the National Health Survey 2020-21, the ten most common chronic conditions are (ABS; 2022):
Injuries
Other than chronic health conditions, injuries are also a major health care concern in the country. According to Australian Institute of Health and Welfare (2022b), injury is the leading cause of death for those between 1 – 44 years old. Among the causes of injuries, falls are the most common cause of hospitalisations and deaths from injuries, followed by contact with sharp or blunt objects, and transport accidents. Other non-fatal injuries that you may observed from patients include bumps and bruises, knee injuries, wounds and cuts, and more.
Find Out More
If you are interested to learn more about injury in Australia, you can visit the Australian Institute of Health and Welfare’s website. This resource includes an overview of injury and provides figures on the different causes of injuries.
Medical Procedures and Equipment

Medical procedures are generally categorised into two main ones: diagnostic and surgical. Diagnostic procedures are usually performed to monitor and investigate the patient’s conditions so that a medical diagnosis (sometimes abbreviated as ‘Dx’) can be established to commence treatment. On the other hand, surgical procedures usually involve the process of cutting or penetrating the body tissues to treat a medical issue after the diagnosis has been made. That said, surgical procedures are sometimes performed for diagnostic purposes, such as a biopsy to investigate the condition further before establishing a diagnosis.
Before looking at the specific medical procedures, we will look at some word parts that are relevant to medical procedures.
| Suffixes | Meaning |
|---|---|
| gram | a record/tracing |
| graph | an instrument that records |
| ostomy | surgical opening |
| oscopy | looking at/examining |
| ectomy | removal of |
| otomy | surgical incision |
| plasty | repair |
Now that you have a better idea of the suffixes related to the medical procedures, we will briefly look at some common diagnostic tests that you may come across (Healthdirect, n.d.):
- Electrocardiogram (ECG): it is a graph of the heart’s electrical activity. ECG is administered if the patient has heart problems such as a racing heart or chest pain. It can show whether the patient is having or have had a heart attack, a stressed heart muscle, irregular heart rhythms, and more.
- Biopsy: the process of taking a small piece of tissue from the patient’s body to test it and helps diagnose disease. Depending on the part of body being looked at, it may involve the doctor cutting the skin to remove a small part of tissue or organ; or a needle is used to draw out some tissue.
- Gastroscopy: it is sometimes known as upper endoscopy, and a procedure that involves a gastroscope (a type of endoscope), a flexible tube, to examine the patient’s upper digestive tract. The endoscope is inserted into the mouth and travels down the oesophagus and then into the stomach and the first part of the small intestines. It is usually performed to investigate indigestion or nausea; sometimes it is performed to treat conditions such as bleeding ulcers or to remove a foreign body.
- Colonoscopy: a procedure that involves a colonoscope, a flexible tube, inserted into the patient’s anus and through the rectum. This allows the doctor to see the inside of their large bowel, i.e., their colon. This procedure is usually done to allow the doctor to investigate changes in the patient’s bowel habits to treat gut problems.
- Magnetic resonance imaging (MRI) scan: it is a procedure that takes detailed pictures of the inside of the body with the patient lying on a table that slides through a tunnel in the middle of the MRI scanner. It can produce highly detailed pictures and usually used to investigate and diagnose the patient’s condition.
- X-ray: a process that uses radiation to create a picture of the inside of the body. X-ray imaging is also known as radiography. When x-ray beams pass through the body, they are absorbed differently by various structures in the body such as bones and soft tissues, which is then used to create an image. There are different types of x-rays, e.g., mammography is an x-ray of the breasts and angiography is the x-ray of the blood vessels.
- CT scan: a type of x-ray that can create 3-dimensional images of the patient’s body, which provides different views and greater details than a 2-dimensional x-ray. CT scan is usually used over an x-ray to see the patient’s soft tissues.
- Ultrasound: it is a process used for screening and diagnosis of the patient’s conditions by using sound waves to capture a real-time picture of the inside of the body. It is a non-invasive procedure and does not use radiation. Ultrasound is also commonly used in pregnancy.
Other than the above-mentioned diagnostic procedures, it is highly likely that you will come across patients who needs pathology tests to have more information for diagnosis and treatment of diseases and other conditions. One of the most common pathology tests is blood test which can be used to assess the patient’s general health and help the doctor diagnose or monitor a range of conditions. Some common blood tests include:
- Fe blood test: some patients may have low iron levels which can lead to anaemia, resulting in fatigue and lack of energy. Too much iron can also increase the risk of patient experiencing severe medical conditions such as liver disease, heart failure, and diabetes.
- Liver function tests (LFT): a group of blood tests to measure protein and enzymes produced or secreted by the liver.
- Full blood count (FBC): a widely used blood test to diagnose a wide range of illnesses, infections, and diseases, including blood cancers and anemia.
Other common pathology tests include urinalysis whereby a sample of the patient’s urine is collected to investigate for any disorders such as diabetes or urinary tract infections.
Find Out More
There are many medical procedures being performed in Australia. If you are interested in learning more and/or have good idea of the field you are working in/wish to work in, you can visit Healthdirect’s website. It has a long list of medical procedures which you could read up more about.
Other than the medical procedures, you should also familiarise yourself with the names of some medical equipment. There are many types of medical equipment and usually each field has its own specific range of medical instruments. For example, you learned about endoscopes, which are a type of flexible plastic tube that allows examination of inside of the body. However, the endoscope for gastroscopy is called gastroscope while the one used for colonoscopy is called colonoscope. There is a wide range of medical equipment and procedure available, and it is impossible to cover the entire range in this Study Guide. Hence, it is important for you to constantly update yourself with the latest medical procedure and equipment relevant and specific to the medical setting you are working in.
Medications and Prescriptions

Depending on the setting you are working in, your role may involve the handling of prescriptions and/or medications. Medications can help patients relieve or cure the symptoms or conditions they are experiencing. Some medications can also prevent further complications in current medical conditions or prolong the onset of disease. While it is understood that you do not have to be an expert in pharmacology, it is still good practice for you to have a good idea of prescribed drugs. Read the extract below that provides a brief overview of drug names.
All drugs are chemicals. The chemical name describes the chemical formula or molecular structure of a particular drug. For example, the chemical name for ibuprofen, an over-the-counter pain medication, is 2-p-isobutylphenyl propionic acid. Just as in this case, chemical names are usually very long, so a shorter name is given to the drug. This name is the generic or nonproprietary name, and it is recognized and accepted as the official name for a drug.
Each drug has only one generic name, such as ibuprofen, and this name is not subject to copyright protection, so any pharmaceutical manufacturer may use it. However, the pharmaceutical company that originally developed the drug has exclusive rights to produce it for 20 years. After that time, any manufacturer may produce and sell the drug. When a company manufactures a drug for sale, it must choose a brand name, or proprietary name, for its product. This is the company’s trademark for the drug. For example, ibuprofen is known by several brand names, including Motrin™, Advil™, and Nuprin™. All three contain the same ibuprofen; they are just marketed by different pharmaceutical companies.
(Fremgen & Frucht, 2019, p. 16)
To help keep the cost of medicines affordable and accessible to Australians, the Pharmaceutical Benefits Scheme (PBS) was established. The cost of medications for most medical conditions are subsidised by the government under the scheme. The list of subsidised medicines is available on the PBS Schedule. The schedule also includes what patients can expect to pay for medicines, i.e., the co-payment to be made by the patients when purchasing the medicines, which is explained further in the extract below.
Find Out More
If you wish to learn more about PBS such as who is eligible for PBS and how are current patient charged, take a few minutes to read through the overview provided by PBS and watch a short clip that explains the scheme.
Medical Specialties

When working in a medical setting, it is important that you are familiar with the different medical specialities as well as the different departments or sections in a hospital. Even though you may be working in a specialised medical setting or not working in a hospital, you are bound to deal with work related to these settings as a manager and will need this information when corresponding with them. For example, you may be tasked to handle referral records to and from other practices/departments or communicate with fellow workers from these settings.
Before we look at the list of departments in a hospital or a health care setting, you should keep in mind that some hospitals may not have all departments available, depending on its size and type. A hospital might include the following departments:
- Inpatient service
- Outpatient department
- Audiology department
- Emergency department
- Urology department
- Orthopaedics
- Radiology department
- Intensive-care unit
- Oncology department
- Paediatric and paediatric-intensive unit
- Haematology department
- Ophthalmology department
- Neurology department
- Trauma unit
- Social work
- Speech pathology
Other than public and private hospitals, you may also have correspondences with other medical settings such as blood banks, hospices, pathology labs, maternity hospitals, and more. In these different settings, other than fellow workers, you will most likely interact and work with different medical specialists, i.e., doctors who are working in specialist fields. Hence, you should get familiar with the names of these medical specialties, as listed in the table below (adapted from Cross & McWay, 2020, pp. 64-65).
| Medical Specialists | Definition |
|---|---|
| Cardiologist | Doctor skilled in the diagnosis and treatment of heart disease |
| Dermatologist | A doctor who specialises in the treatment of infections, growths, and injuries related to the skin |
| Anaesthesiologist | A doctor who specialises in anaesthesiology; an anaesthesiologist administers anaesthetics, of which there are two types: general anaesthetics, which produce sleep, and regional anaesthetics, which render a specific area insensible to pain |
| Endocrinologist | A doctor skilled in the diagnosis and treatment of disorders of the glands of internal secretion |
| Gastroenterologist | A doctor who specialises in the study of the stomach and intestines and their diseases |
| Geriatrician | A doctor who specialises in the diagnosis and treatment of the diseases of the aging and elderly |
| Gynaecologist | A doctor who specialises in the diseases of the genital tract in women |
| Haematologist | A doctor who specialises in the science of blood and blood-forming tissues |
| Immunologist | A doctor who specialises in addressing allergic reactions and immunologic disorders |
| Nephrologist | A doctor who specialises in the science of the kidneys |
| Neurologist | A doctor who specialises in the science of the central nervous system |
| Obstetrician | A doctor who specialises in pregnancy, labour, and the puerperium |
| Oncologist | A doctor who specialises in the study of tumours |
| Orthopaedist | A surgeon who specialises in the preservation and restoration of the function of the skeletal system, its articulation, and associated structures |
| Ophthalmologist | A doctor who specialises in diagnosing and prescribing treatment for defects, injuries, and diseases of the eye |
| Otorhinolaryngologist | A doctor who specialises in the diseases of the ear, nose, and throat |
| Pathologist | A doctor who specialises in diagnosing changes in body tissues and organs that cause or are caused by disease |
| Paediatrician | A doctor who specialises in the diagnosis and treatment of children’s diseases |
| Proctologist | A doctor who specialises in the diagnosis and treatment of diseases of the rectum and anus |
| Psychiatrist | A doctor who specialises in the diagnosis and treatment of mental disorders |
| Radiologist | A doctor who specialises in the interpretation of X-rays and other radioactive substances used for diagnostic purposes |
Other than the specialists, there are also other health professions that you may come across when working in a medical setting, including (adapted from Cross & McWay, 2020, pp. 66-69):
- Dentist: doctor who is concerned with the teeth and associated structures
- Dietician: a specialist who is trained in the use of proper diet for the promotion of health, prevention of disease, and therapy for treatment of disease
- Psychologist: an individual who specialises in treatment of mental health issues and abnormal behaviour
- Nurse: a specialist working directly with patients and administering treatments following instructions by doctors
- Occupational therapist: a professional who aids patients with the rehabilitation of fine motor skills
- Radiographer/radiologic technician: an individual who is trained to produce x-ray images of the human body for use in diagnosing medial problems
Ultimately, the terminology you should know boils down to the specific setting you are working at, and who you need to communicate with. Your workplace would most likely provide training to ensure that you are proficient in the knowledge required. Otherwise, there are different sources of information that you could seek clarification from, which we will discuss in the later part of this section.

As a medical worker, it is essential that you have a sound knowledge and understanding of the health care system in Australia, specifically the health insurance system. Your role may require you to process and manage insurance claims, keep claim records, as well as answering any fees and insurance enquiry from the patients. Health insurance is usually taken out to help reduce or waive the cost of health care services and treatment to ease the burden of the patients. We will first look at Medicare, the national public health insurance then the private health insurance system.
In Australia, the national health care funding system provides eligible Australian residents the opportunity to access health care at an affordable cost or no cost. This is achieved by the implementation of the national public health insurance scheme, Medicare, whereby patients are processed and treated as public patients in the health care system. Medicare covers the cost of treatment in public hospitals for eligible residents and subsidises the cost of most health services and treatments such as specialists, dentists, and other allied health professionals.
Eligibility for Medicare is automatic for Australian citizens, New Zealand citizens living in Australia and most permanent residents of Australia. Overseas visitor from countries that has agreement with Australia’s Reciprocal Health Care Agreements are also eligible for Medicare, including countries like Italy, Ireland, Finland, New Zealand, Slovenia, United Kingdom, and more. Do note that if you have patients from these countries, it is important that you find out what services and treatments they are covered for as each country has different arrangement with the Australian Government.
For those who are eligible for Medicare, they will receive a Medicare card, or have their name added to their parent or guardian’s Medicare card (see image below; Healthdirect, 2022).

When they access the Medicare system, they need to present their Medicare card. Some services that are fully or partially covered by Medicare incudes doctors’ and specialists’ fees, blood tests, eye tests, and more. However, it is important to note that Medicare does not cover some services such as ambulance transport, contact lenses or glasses, and most allied health services. While the full list is too long to be included here, it is important for you to learn and remember the services offered by your workplace and whether they are covered by Medicare; if so, how much of each service’s fee is covered.
Broadly speaking, the Medicare system is made up of three main components:
- Hospital treatments – treated by a doctor as a public patient in a public hospital
- Medical services – visiting a health professional outside of a hospital
- Pharmaceutical – prescription medicines purchased at pharmacies
Medical Benefits Schedule (MBS)
Each consultation and procedure that is provided by a health professional is considered an item number. For each item number, the MBS will assign a schedule fee to it and the amount is what the government considered appropriate for these services. This schedule fee is the amount that Medicare will pay when a claim is submitted (also referred to as the Medicare rebate). That said, health professionals are allowed to charge whatever amount they wish for their services, i.e., the private billing fee. In Australia, most health professionals would charge more than the schedule fee, which is more than the Medicare rebate. This means that patients have to pay the excess amount, more often referred to as the out-of-pocket cost or gap.
Some healthcare providers offer bulk-billing, which essentially means that they accept the Medicare benefit as the full payment for their services. When visiting these providers, Medicare card holders only need to present their Medicare card and do not have to pay any fees. However, it is worth noting that some providers only bulk-bill on certain days or certain hours of the day, and this can be confusing for some patients. If you are working in a practice that bulk-bills (or don’t), make sure you convey accurate information to your client so that they do not have any unexpected costs. Generally speaking, if an out of hospital service is on the MBS, Medicare will pay the following (Healthdirect, 2022):
- the full schedule fee for general practitioner services
- 85% of the schedule fee for a specialist
- 75% of the schedule fee for in hospital services (but if you have private hospital insurance cover for the medical service, your insurer may pay the gap of 25% of the MBS fee.)
Let us look at an example. The MBS schedule fee for a General Practitioner consultation (MBS item 23) is $39.75. Jocelyn is a GP who bulk-bills only on weekdays; her consultation fees are $80.00 on weekends. Hence, her patients who are eligible for Medicare only need to present their Medicare card and do not have to pay anything on weekdays while her patients on weekend have pay a gap of $40.25.
Prior to claiming Medicare benefits, health practitioner will first need to get a Medicare provider number, which allows easy identification of the practitioner and their eligibility for Medicare benefits. A Medicare provider number also allows the practitioner to refer patients to specialists, imaging or pathology services, and claim or bill Medicare services. The number consist of a 3 to 6 digit that identifies the doctor with 2 additional characters that identify their practice location, e.g., 12345AZ. Note that the provider number is location specific, i.e., if the practitioner is practising at more than one location, they would need a provider number for each location.
While Medicare waives or reduces most medical costs for Australians accessing the public health care system, there are still some procedures or treatments that are not covered by Medicare., such as physiotherapy and some dental services. In these instances, Australians are able to take on private health insurances to receive treatment as a private patient as well as help pay for costs not covered by Medicare. In addition, private health insurance might help patient gain quicker access to some hospital services such as shorter waiting time as well as having the option to choose their hospital, doctor, and specialist (Department of Health and Aged Care, 2021). Depending on the work setting you are in, you may come across patients who have private health insurance and are receiving services and treatment as a private patient. You would also need to familiarise yourself with your workplace’s private health insurance claim policy as some practices process private insurance claims on the spot while others do not.
Reading D – How Health Insurance Works
This reading will provide an overview of the health system in Australia by looking into Medicare and private health insurance individually, as well as comparing the differences between them.
Self Reflection
Before proceeding further, take some time to reflect the medical terminologies that you just learned. Are there any of them that you would like to learn more about? Or are there any terminologies that are more relevant to your work setting?

Now that you have a good understanding of the common medical terminologies, we will look at how you could respond to instructions that contain medical terminology. The instructions and documents you come across will depend on your work setting and the specific role you are in. For example, if you are working in a skin clinic, most of the referral documents you receive would be relevant to skin checks; if you work in a psychology practice you may come across many mental health care plans.
Regardless, it is important that you become familiar with the medical terminology relevant to these instructions, including the abbreviations of these terms. Otherwise, you might reduce work efficiency and put the patients at inconvenience or at risk. For instance, if you process the patient’s claims incorrectly, they may have to pay a higher gap, or if wrong postoperative instructions are given, patients might develop complications for their health conditions. We will have a brief look at what are some common written and oral instructions that you would need to interpret and/or document. Remember, this list is not exhaustive, and you should take note of the specific ones relevant to your workplace.
Patient notes
Patient notes are one of the most commonly used documents to record and communicate a patient’s progress. It typically consists of the patient’s details, relevant clinical findings, any medical decisions and actions made and agreed (including who made them), information given to patients, any drugs prescribed. While it is the doctor or health practitioner’s responsibility to fill in the patients notes, it is important that you are able to interpret and understand the terminology used. Depending on your specific role, you may need to communicate this information to fellow workers or other health practitioners.
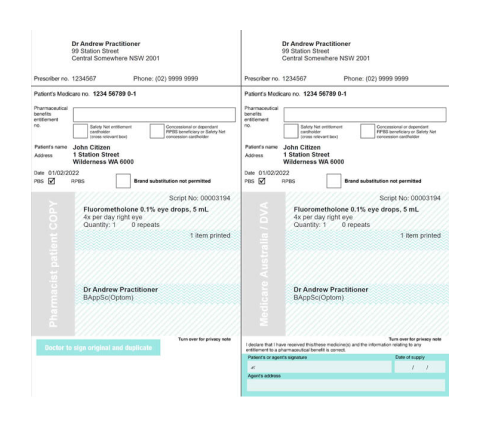
Prescriptions (often abbreviated as ‘Rx’)
You may be required to read prescriptions in your role. A prescription would usually include the patient and practitioner’s details, as well as the prescribed drugs details, including the drug name, administration instructions, intervals, and whether a substitute drug can be dispensed. The prescription will also indicate whether it is a repeat, i.e., the patient can obtain the prescribed drug in a set interval without having to see the practitioner every time. While some prescriptions are digitally printed, some practitioners still prefer to write it by hand. If you are unsure about what is written, always check and clarify with the prescriber before you proceed. Let’s look at some common abbreviations that you may come across in a prescription, though note that your workplace may have a specific list of abbreviations (Commonwealth of Australia, 2016):
| Abbreviation | Definition |
|---|---|
| mane | in the morning |
| nocte | at night |
| bd | twice a day |
| tds | three times a day |
| qd | every day |
| qid | four times a day |
| q4h, 4 hrly, 4 hourly | every 4 hours |
| q6h, 6 hrly, 6 hourly | every 6 hours |
| q8h, 8 hrly, 8 hourly | every 8 hours |
| prn | when required |
| 3d | For three days |
| 5d | For five days |
| IV | intravenous |
| PO | oral |
| g | grams |
| mg | milligrams |
| mL | millilitre |
| mg/L | milligram per litre |
See below a sample of how a prescription looks like.
Test Results
While health practitioners will be interpreting and analysing test results, some practices or work roles may require you to document patient’s test results for their medical records. Other than the few common diagnostic tests we looked at above, there are other specific tests that you may come across, depending on the specific field you work in. While this Study Guide could not possibly cover every single test, your workplace would most likely provide relevant training and/or procedural documents about documenting common test results for their practice.
Find Out More
If you are interested in finding out more about specific pathology tests, including why and how it is done, and what pathologists are looking for, take some time to visit Pathology Tests Explained. They have resources that look at different pathology tests and quick read information sheets.
Post-operative care instructions
Your workplace may hold surgical procedures, including operations, and you may be tasked to communicate post-operative care instructions to the patients or to check in with the patients about their post-operation progress. Post-operative care is basically the care that a patient receives after a surgical procedure, and the type of care depends on what kind of surgery they had and their health history. Hence, you should have some basic knowledge about post-operative care such as pain management and wound care, the procedure itself, expected post-operative course and any potential side effects or procedural complications. When working with individual patients, it is also good practice that you have some knowledge of the patient’s condition in relation to their procedure, any risk factors for developing complications and how their post-operative care will be carried out (Department of Health, 2015).
To aid with this, your practice will have a set of post-operative procedures for the staff to adhere to. Typically, the practitioner will communicate, both written and verbal post-operative orders to the patient and any staff involved. The stakeholders involved will then have to sign off to indicate they received and understood the instructions. If you are involved in delivering or actioning post-operative instructions, you are responsible for making sure you received the correct information and fully understood them before you sign off. Otherwise, please remember to raise any doubts and/or clarify with the practitioner before accepting care of patient.
Referrals
When working in a medical setting, one of the documents that you will frequently encounter is a referral. A referral is a written request from one health professional to another health professional or health service, requesting their expertise for the patient’s care and assessment. In principle, a referral is not a must for a patient to see a medical specialist, however, patients are able to benefit from having a referral. A referral typically includes clinical information about the patient and their condition so that the referred practitioner have a good idea of the patient’s background information and does not have to ask the patient so many questions, and they know exactly what they need to do with the patient. A referral also includes the date of referral and the signature of the practitioner who initiated the referral. The patient can request for the referral to be addressed to a specific specialist; if they do not have a preference, it will be a general referral without a specific name (e.g., Dear gynaecologist). Some common referrals include pathology services like blood and urine tests and diagnostic services such as x-rays and MRI scans.
A referral usually indicates clinical importance, and that Medicare would cover at least the partial cost. While a referral is not a must to see a specialist, Medicare does not cover specialist visits without a referral (Healthdirect, 2021). When receiving patients, it is important that you check with them whether they have a referral and clarify the billing procedure so that they do not have any unexpected costs. Also, when receiving patients with a referral, you need to ensure that referrals are not made from more than 12 months ago, unless they are patients receiving care for their chronic condition. Read the extract below that explains how long a referral lasts.
Most referrals from general practitioners (GPs) to specialists are limited to 12 months. They should cover a single course of treatment for the condition you are being referred for. The referral covers all the visits to the specialist for that condition.
If you need continuing care, such as for a chronic (continuing) health condition, the GP can write a referral beyond 12 months or for an indefinite period. If you develop a new condition, you will need a new referral for that condition.
Referrals from specialists and consultant physicians to other specialists are limited to 3 months unless the patient is admitted to hospital.
(Healthdirect, 2021)
Similar to other form of instructions, your workplace will have their policy and procedure surrounding referrals. For example, how are referred patients processed and how to establish and maintain their medical records. When in doubt, always clarify with your supervisor or refer to the policy and procedure manual. Otherwise, if the patient record is not processed correctly, it may affect their Medicare claims process. See below an example of a referral letter from a general practitioner to a speech pathologist.
Telephone calls
Another source of oral instruction that you may receive in your role is telephone calls. These calls can be between you and patients, patients’ families, fellow workers, and other health practitioners. Depending on the size of your workplace, you may even receive instructions from health practitioners from other departments. For instance, you may receive instructions from a fellow worker to check in on the progress of a patient you are working with. Perhaps you are asked to take down a message for a health practitioner at your workplace as they are unavailable. To do all these, you need a good command of the medical terminologies, otherwise you could not interpret their instructions and act on them. Additionally, you need to know the correct pronunciation of these terminologies to correctly interpret and understand what they are saying. As usual, always check and clarify if you are unsure to prevent miscommunication.
Work Health and Safety (WHS) signs
Another important set of instructions that you should be familiar with is the work health and safety (WHS) policy and procedures at your workplace. WHS is the management of risks to the health and safety of everyone in your workplace, including patients and their families, fellow workers, health practitioners, and any visitors to your workplace. Your workplace should have established a set of WHS policy and procedure to ensure the safety of everyone onsite, and you should be inducted about it when you commence work.
Due to the nature of your workplace, there will be various WHS signs and instructions to remind you about the potential health and safety risks. You must be able to correctly interpret and understand these instructions to avoid work incidents that may put yourself and others at risks. You should be familiar with some common signs such as the First Aid sign, fire signs, and emergency exits (shown below).
- The first aid sign
- Emergency exit sign
- The fire extinguisher sign
- While common signs such as the above ones would be present in most workplaces, depending on your workplace, there may be signs and instructions that are specific to your workplace. For example, if you work in a pathology clinic, you may see signs like the biohazard sign; if you work in a radiology clinic you may see signs like the radiation hazard sign (below).
- The bio-hazard sign
- The radiation hazard sign
Your workplace will induct you when you commence work, including showing and informing you of the different WHS signs and instructions. However, it is still good practice that you familiarise yourself with the common WHS signs, as well as periodically refresh your knowledge to avoid work incidents and maintain the safety and wellbeing of those on site.

Earlier on, we briefly mentioned that you are expected to follow the policies and procedures at your workplace. These are written documents that typically include guidelines and practices developed to address legal, regulatory, and ethical requirements. They are often used as a form of communication to the stakeholders about the organisation/practice/workplace’s vision and goals, and the methods and actions to be taken to achieve these goals.
As a staff, you are legally obligated to comply with some policies (e.g., work health and safety policies and emergency procedures), while other policies are put in place to ensure the safety and wellbeing of everyone present in the setting (cleanliness and hygiene protocol). Other than knowing how and where to access these documents, it is also crucial that all staff can interpret them correctly and know why it is necessary to adhere to these documents. When you commence work, your supervisor or the person inducting you should assist you in familiarising these documents.
Before we look at some key policies and procedures, let us clarify the differences between policies and procedures:
- Policies: They are an overall plan for an organisation to reach general goals and expectations. It is often a statement that acts as a guidance for staff on how they should behave and make decisions related to the operation of the workplace. It also acts as a guide of what is expected of the staff. Policies can be as broad as philosophies and as specific as rules and guidelines. Examples include policies about patient rights, drug storage and disposal, and transfer of medical records
- Procedures: They are more specific and factual as they describe how a policy is to be practically applied. Procedures also outline reporting processes, e.g., who should report to who, types of reports made and what should be included in a report. One of the aims for procedures is so that reports and progress are documented, and they can be referred to when needed. Examples include staff rosters, emergency response, submission of medical claims, administrative systems.
| State/Territory | Act |
|---|---|
| Australian Capital Territory | Work Health and Safety Act 2011 (ACT) |
| New South Wales | Work Health and Safety Act 2011 (NSW) |
| Northern Territory | Work Health and Safety (National Uniform Legislation) Act 2011 (NT) |
| Queensland | Work Health and Safety Act 2011 (Qld) |
| South Australia | Work Health and Safety Act 2012 (SA) |
| Tasmania | Work Health and Safety Act 2012 (TAS) |
| Victoria | Occupational Health and Safety Act 2004 (Vic) |
| Western Australia | Occupational Health and Safety Act 1984 (WA) |
| Commonwealth (covers workers for the Commonwealth Government and businesses licensed to self-insure under the Comcare scheme) |
Work Health and Safety Act 2011 (Cwth) |
Emergency Plans and Procedures

One major component of WHS policy and procedure is the emergency plan and procedure, i.e., what to do in an event of an accident or emergency. It acts as a guideline for workers and others at the workplace so they know what they should do in an emergency so as to achieve an effective response to an emergency. Having an emergency procedure in place also helps facilitate effective communication between the authorised individual coordinating the emergency response and everyone one else on site. The extract below shows what a typical emergency plan usually includes:
- emergency contact details for key personnel who have specific roles or responsibilities under the emergency plan, for example fire wardens, floor wardens and first aid officers
- contact details for local emergency services, for example police, fire brigade and poison information centre
- a description of the mechanisms for alerting people at the workplace to an emergency or possible emergency, for example siren or bell alarm
- evacuation procedures including arrangements for assisting any hearing, vision or mobility-impaired people
- a map of the workplace illustrating the location of fire protection equipment, emergency exits, assembly points
- triggers and processes for advising neighbouring businesses about emergencies, and
- the post-incident follow-up process, for example notifying the regulator, organising trauma counselling or medical treatment.
Procedures for testing the emergency plan including the frequency of testing must be included.
(Safework Australia, 2021, pp. 2-3)
It is crucial that your workplace keep their emergency plan and procedure plan up to date, and that all staff, including yourself, are familiar with these documents to help minimise workplace risk and be more ready if a work incident occurs. Depending on your specific role at work, it may be part of your duty to undertake the WHS duties, including maintaining the emergency plan to ensure that it is always effective and organising emergency drills.
On top of that, it is essential for your workplace to have first aid arrangements and plans, especially working in a medical setting. Your workplace and the designated WHS officer have a responsibility to make sure that the first aid equipment and facilities are always provided and accessible. Further, your workplace should have an adequate number of staff that are trained to administer first aid in response to an emergency.
Privacy and Confidentiality
As a manager, you must respect a patient’s rights to the privacy and confidentiality of their health information. To protect their interests, the Privacy Act 1988 are put in place to protect the patient’s privacy in health setting. The laws govern how the patient’s health record and information can be shared and handled, including who can and cannot access these documents. By laws, health practitioners must not disclose what they discuss with their patients with a third party, unless informed consent is provided by the patient. This also extends to health records when seeing a new practitioner – the patient has the right to determine whether they wish to share their previous health record with a new practitioner. This includes the healthcare situation the patient is experiencing, any medications or treatment discussed and received, and other personal information. Depending on your role, you may or may not discuss the patient’s medical situation with the patient, though you would most likely handle and process their medical and health records (Better Health Channel, 2015). In these cases, you must also respect the patient’s privacy and not disclose their health information to any third party and only handle the information as per your work role requirement, e.g., processing claims and updating medical records.
However, there are certain circumstances that are exempted from the privacy laws, i.e., the patient’s health information may be used or shared without their consent. This occurs when the health practitioner believes that the health and/or safety of the patient or someone else are going to be seriously threatened and the information would help minimise or avoid the harm. For example, the doctors may disclose the patient’s medication history and/or drug allergy if they are unconscious but require immediate care. Another situation would be when the information is crucial to prevent a serious threat to public health or safety. For instance, during the COVID-19 pandemic, de-identified contact tracing information were released to the public so they could get tested and monitor for any symptoms to prevent further spread.
This also extends to how patients’ information is recorded and stored at your workplace. Regardless of whether your workplace uses paper or electronic record, it is important to ensure that their medical record and personal information are stored securely and only accessible by those who are authorised to do so. Otherwise, patients’ privacy may be easily compromised and there may be legal repercussions under the privacy laws. Your workplace will have a privacy and confidentiality policy as well as a procedure to guide the staff on how to handle patient information. Make sure you have read through it and have a clear understanding and clarify with your supervisor when needed.
Specific Guidelines
Depending on the specific field you are in, there are additional policies and procedures that you and your practice are expected to follow. For example, if you are working in a general practice, you should adhere to the Royal Australian College of General Practitioners (RACGP). If you are working for a counselling practice, you should refer to the Australian Counselling Association’s Code of Ethics and Practice.
Find Out More
If you are interested to learn more about how health service providers should handle and maintain health information about their patients, read this guide to better understand the obligations under the privacy laws.
Office Practice Manual

Usually, a workplace will have a practice manual that acts as a guideline for all staff to adhere to, including the common protocols, practices, procedures, and systems that supports the workplace’s services and operation. As a staff, it is important for you to familiarise yourself with these procedures and act accordingly to assure that a consistent quality of care and services are delivered to patients. When all staff adhere to the practice manuals, it also facilitates a smooth service coordination within the practice, or even between departments, if you are working in a larger practice/facility.
For instance, you are tasked to call back a patient to schedule their appointment with your multi-disciplinary practice. However, the worker from the previous shift only took down their name and mobile number; without any further information, you spent a longer amount of time assisting the patient to figure out the more appropriate health practitioner to book an appointment with. The patient is also frustrated that they have to talk about their situation again. On the contrary, if the worker followed the workplace procedure about new patients, they would have taken down more basic information about the patient. With more information on hand, the patient does not have to repeat themselves and you could also improve work efficiency.
The content in the practice manual varies depending on your workplace and types of services that are offered there. It can range from accounting policies to privacy policies. Even though this manual should be kept in a place that is easily accessible by staff, you will still need to have a good understanding of the policies and procedures relevant to your roles and responsibilities. Of course, when in doubt, always clarify with your supervisor or a more senior staff to prevent miscommunication or conveying the wrong information to the patients and fellow workers. Let us briefly look at a few common procedures that are usually found in an office manual.
Recording Information
As mentioned earlier, a patient’s right to the privacy of their information including what is recorded and stored by the service provider. While the type of information to be taken down and its format will depend on your workplace, it generally documents all direct contact between the provider and the patient as well as any significant activity that is relevant to the patient’s care, e.g., information provided to the patient and any missed appointments. The following is an example of how a documentation may look like for an allied health assistant in an acute ward (note: PT = physiotherapist; OT = occupational therapist; SP = speech pathology).
Example 1: Acute Ward AHA
| Date Time | [DISCIPLINE] Allied Health Assistant |
|---|---|
|
Patient consent obtained. Nurse reports stable vital signs. |
|
|
[Document relevant comments from patient] Treatment - Mobilised X with X aid and X assistance as per PT instructions.
|
|
|
[Comment on relevant observations] Plan: Feedback to PT/OT/SP, review X |
|
|
[Signature] (Printed Name) Allied Health Assistant |
Depending on your role, you may not have any direct contact with patient, or are not directly involved in delivering treatment or care to the patient, but this does not mean that you would not need to record any patient information or do not have to abide by the privacy laws. You may need to record a patient’s information when they are new to the practice, or that you need to record or update their medical notes. Essentially, as long as you come across any patient information, you would need to adhere to your workplace’s procedure about recording information and abide by the privacy laws.
If your role requires you to manage the appointment system, you will need to ensure that you know how the system operates, e.g., how to schedule an appointment or reschedule an appointment. This is extremely important as you do not want to risk scheduling the wrong appointment times for the patient or did not correctly cancel an unwanted appointment.
Accessing and Updating Files
As per the privacy laws, only specific people are allowed to access patients’ medical files with informed consent. Other than the health practitioner and the patient themselves, you may receive requests from other service providers or health practitioners for a copy of the patient’s health record. You should never just hand over the patient’s information; instead, clarify whether the patient has provided informed consent for them to access their health records. You should only act in accordance with your workplace’s privacy policy and the procedure relevant to patients’ health records access. This includes updating the patient’s health record with new information.
Telephone Protocols
Other than in-person communication, telephone call is the most common way for a (potential) patient to get in touch with your practice. Therefore, it is essential that your workplace has a telephone protocol and that all staff follows it to ensure the service delivery standard is consistent and maintain work efficiency. The protocol typically includes the etiquette they expect staff to display, including but not limited to:
- the tone and speed when speaking on the phone
- answering the phone in a professional manner
- prioritise emergency calls and triage the urgency of each caller, including how to ask about patient’s signs and symptoms
- taking messages, including the information to take down
- transferring to a health practitioner or fellow worker
- not using speakerphone to respect patient’s privacy
- performing call backs/follow-ups phone calls
One thing to remember is that if the other person on the line is being rude and abusive, stay calm and follow your workplace’s protocol as to how to terminate the call. E.g., “I can hear how upset/angry/frustrated/annoyed you are about this issue. However, it is not appropriate for you to use inappropriate/abusive language. Please refrain from using abusive language or I will have to terminate the call and we can call back at a more appropriate time.” Also, if the caller is in crisis or experiencing an emergency, you should immediately advise them to ring emergency services, or transfer them to an emergency line operator (if your workplace offers this service).
Correspondence Formats
Other than telephone calls, you may also need to have written communication with patients, fellow workers, and health practitioners, e.g., letters, emails, and messages. It is important that when you are required to have written communication you adhere to the workplace’s standardised correspondence format to ensure effective communication and maintain work efficiency. Further, using a standardised correspondence format also conveys professionalism to stakeholders, which can also increase the reliability and trustworthiness of your practice to others. This usually includes email headings and signatures, the practice’s letterhead or fax templates, who are authorised to communicate with whom, and more.
For instance, a fellow worker might need to follow up with a patient that you have been corresponding with. If the communication is written in line with the workplace’s procedure, your co-worker would know where to find crucial information to assist the patient. Other instances that you may need to correspond with external stakeholders include other facilities or departments within your practice for different documents, e.g., pathology test results and referrals.
Billing Policies
You may receive enquiry about the billing policies such as Medicare and private health insurance claims, or the fee charged for the services provided by your workplace. While you may refer to the manual for the fee of a service if a (potential) patient enquires, taking some time to flip through the manual does not convey professionalism. Not only that, having a good understanding of the fees and billing process would reduce any misinformation provided to the patient so they would not be surprised by any unexpected cost. If you are unsure of the MBS item number when preparing invoice, it is always best practice to seek clarification from the health practitioner to avoid any mistakes.
Cleaning and Hygiene

Your workplace will have a cleaning and hygiene protocol, such as the hourly and daily cleaning schedule. For example, your workplace has a protocol whereby the bin has to be cleaned every two hours, and the reception area has to be disinfected before opening and after closing. This is particularly important as you would not want to compromise the health and safety of individuals visiting the practice as they may already be vulnerable. Further, after COVID-19 pandemic, most health settings have tighter cleaning and disinfection protocols, including signs about washing hands regularly and correctly, and to maintain a safe distance if feeling unwell. You should have a thorough understanding of your workplace’s hygiene protocol and make sure you adhere to them to minimise the risk of patients and other fellow workers.
While it may seem like there are many policies and procedures you have to keep track of, your workplace would most likely have an office practice manual that you can refer to. All staff should know where this manual is located, and it should be kept at a place that is always easily accessible to staff. Other than the office practice manual, if in doubt, you can always seek clarification from other sources, which we will look at now.

Working in a medical and health setting can sometimes be overwhelming due to the ever-changing field and many updated information to keep up with. If you are unsure or do not understand something, do not hesitate to seek assistance from others to clarify your doubts. This is especially so when you do not understand the meaning or context of a medical terminology. Otherwise, you may be providing incorrect information or knowledge to the patients and fellow workers, which may have serious consequences.
Other than referring to your office practice manual, you can approach your supervisors for assistance about the practice’s policies and protocols. For example, you are helping a patient who double-booked for an appointment, and you are unsure of the practice’s procedure on double bookings. You then reach out to your supervisor for their help to guide you through the procedure. You could also approach fellow workers who are more senior and experienced than you for their assistance.
For matters that are not relevant to the practice’s policies and procedures, you could refer to online resources. For example, your role may involve handling and managing drugs and you wish to learn more about the common drugs prescribed. You can then head to the Australian drug databases to find out more about the drugs. Recall that there are medical terminologies that are specific to a particular field. If you are working in one, or intending to, you might be interested in getting familiar with these terminologies. You can refer to a medical dictionary to learn more or use online resources to explore them. Below are some medical terminology references that you could refer to:
- Dorland’s Medical Dictionary
- Mosby’s Medical Dictionary
- Merriam-Webster Medical Dictionary
- Medical Term
- WebMD Dictionary
- Medical Mnemonics
Do note that you have to be mindful of the spellings and pronunciation of these medical terminologies and ensure they are in Australian/English spelling instead of American spelling.
Self-Reflection
Take a few moments to reflect on the following:
- What are some sources of clarification and assistance that I can go to at work?
- Do I have any additional sources or support available to me at work?
- What do I want to learn more about that are relevant to my work role? E.g., physiotherapy, counselling, GP practice, etc.
This section of the Study Guide provided you with some introduction about medical terminologies, including the word structure of a medical terminology and the different abbreviations commonly used in the field. You also learned the common medical equipment and procedures that you may come across as a manager, including the different medical specialties and Medicare and private health insurance. We also looked at the different policies and procedures that you need to familiarise yourself with and the need to adhere to them to ensure efficient and smooth service delivery and coordination between fellow workers.
