Dementia (mate wareware) is an umbrella term used to describe a group of symptoms that affect how well our brains work. It is characterised by changes in memory, thinking, behaviour, personality and emotions.
According to Alzheimer’s New Zealand, Dementia mate wareware can affect anyone. Dementia is not a normal part of the aging process, however as people get older the chances of developing dementia increase.
Dementia is associated with diseases of the brain, so we will begin by outlining the basic structure and functioning of the human brain and the nervous system. The brain and nervous system are like the body's communication network. The brain is the control centre, and the nervous system carries messages between the brain and the rest of the body. This system allows us to think, move, remember, and feel. When dementia occurs, there are problems with how the brain and nerves work leading to memory loss, confusion, and changes in behaviour.
How is the brain impacted in Dementia
The human brain is about the size of two fists and has a soft, folded structure. It's a complex organ with billions of nerve cells. The brain has two halves, left and right, connected by a bundle of nerve fibers called the corpus callosum. The left side is for speech and thinking, while the right side handles spatial tasks. Also, each side controls the opposite side of the body. So, if one side is damaged, it affects the other side of the body.
Activity - Exploring the brain and dementia
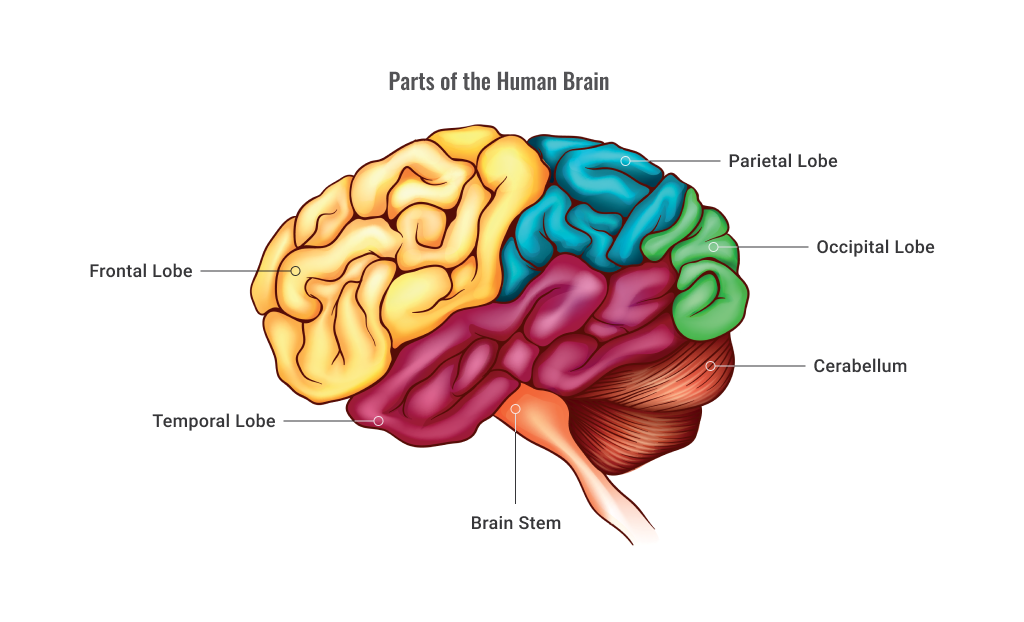
- Frontal Lobe
- Reasoning
- Thinking
- Planning
- Language
- Emotions
- Judgement
- Motor Function
- Movement
- Short Term Memory
- Parietal Lobe
- Knowing right from left
- Hearing
- Sensation
- Smell
- Taste
- Touch
- Occipital Lobe
- Vision
- Visual processing
- Colour identification
- Cerabellum
- Coordination
- Balance
- Vestibular
- Attention
- Brain Stem
- Breathing
- Temperature
- Heart rate
- Temporal Lobe
- Understanding language
- Memory
This activity is designed to help you understand the different parts of the brain and how they function, as well as how dementia affects the brain. You'll use an interactive brain tour on the Alzheimer's Research UK website to explore these concepts in more detail.
Read more at the Alzheimer's Research UK site: The Brain Tour.
Once on the website, explore the interactive Brain Tour by clicking on different parts of the brain.
Pay attention to the information provided about each brain region, its function, and how dementia can affect it.
Take your time to read and interact with the content. You can click on images, diagrams, and text for more information.
Use the diagram above and ‘the brain tour’ to answer these multiple choice questions.
Activity - Watch
Watch this introduction to dementia video to understand how dementia affects the brain.

Dementia is a significant concern in our aging population, and providing support and care to individuals affected by this condition may be a large part of your role in support work for aged care. In New Zealand, several dedicated organisations and resources are committed to improving the quality of life for those living with dementia, as well as offering guidance and assistance to their families and caregivers. First, let’s look at some facts about dementia in Aotearoa.
Read the questions below and flip the cards to find out the facts and figures about dementia in Aotearoa.
Read more facts and figures and how dementia affects Kiwis and people around the world.
Dementia support
In New Zealand, there are several organisations dedicated to dementia care and support. Understanding and being aware of these various organisations will equip you with essential tools for effective advocacy and client support. By knowing about these organisations, you can serve as knowledgeable guides for your clients, connecting them with the appropriate resources and services tailored to their specific needs. Moreover, this knowledge extends beyond individual clients, as support workers can also play a pivotal role in educating and providing valuable information to whānau of individuals with dementia ultimately enhancing the quality of life for both those living with dementia and their loved ones.
Some of these prominent organisations include:
Activity - Research
Take 30 minutes to research dementia support in your local area and find out about the support and help available to people affected by dementia in your region. This could be helpful information for the people you support in your day-to-day role as a support worker.
Activity - Watch
Watch this video from Alzheimer’s New Zealand about investing in new initiatives and providing resources and support for those living with dementia and their carers. Listen to what activities are important for people living with dementia.

There are many different types and causes of dementia. The most common types are:
- Alzheimer’s disease
- Vascular Dementia
- Lewy Body Dementia
- Korsakoff’s Syndrome and Alcohol-Related Dementia
- Frontotemporal Dementia
- Huntington’s Disease
- Parkinson’s Disease
- Young-Onset Dementia.
Alzheimer’s disease
It is the most common form of dementia, affecting 70% of people with dementia. It is caused by brain cells dying, which in turn causes the brain to shrink. This results in the progressive loss of functioning, and eventual death. It initially affects the hippocampus, which is responsible for memory and learning. As the disease progresses, it can also affect other parts of the brain involved in communication, reasoning, and other cognitive functions. There is no cure, and treatment focuses simply on maintaining the person’s functioning as long as possible and relieving symptoms and side effects, such as agitation, depression and insomnia.
The following list identifies the causes and risks associated with AD
- Genetics: Certain genes, such as the APOE gene, have been linked to an increased risk of developing Alzheimer's disease.
- Age: Alzheimer's disease is most common in people over the age of 65, and the risk increases as people get older.
- Lifestyle factors: Research suggests that lifestyle factors such as diet, exercise, and social engagement may play a role in the development of Alzheimer's disease. For example, a diet high in saturated fat and cholesterol may increase the risk, while regular physical activity and mental stimulation may decrease the risk.
- Brain changes: Alzheimer's disease is characterised by the accumulation of beta-amyloid protein plaques and tau protein tangles in the brain, which can interfere with normal brain function and eventually lead to the death of brain cells.
- Inflammation: Chronic inflammation in the brain has been linked to Alzheimer's disease, and may be caused by factors such as infections, head injuries, or chronic stress.
Resource
Learn about Alzheimer's in New Zealand.
Vascular Dementia
There are several types of vascular dementia (VaD), which results from inadequate flow of blood to the brain, often occurring after strokes. High blood pressure and thickening of the arteries are also contributing factors. Multi-infarct dementia, caused by a series of small strokes, develops progressively to cause damage to the brain’s cortex. This is the most common form of vascular dementia. Atherosclerosis, the buildup of plaque in the arteries, a condition known as atherosclerosis, can also increase the risk of VaD. Diabetes is another risk factor for VaD, as it can lead to damage to the blood vessels in the brain and other organs. Smoking has been linked to an increased risk of VaD, as it can damage the blood vessels throughout the body. The progress of the disease is similar to that of Alzheimer’s and may include mood swings, severe depression and epileptic seizures. Subcortical vascular dementia is also relatively common and related to changes in the brain resulting from a stroke. Brain damage that has already occurred cannot be reversed, but treatment to prevent future strokes through a healthy lifestyle as well as drugs to reduce cholesterol and high blood pressure can prevent further damage.
Resource
Learn more about vascular dementia.
Lewy Body Dementia
Lewy bodies (LBD) are abnormal, round structures that develop inside nerve cells in the brain and result in dementia. Lewy body disease is similar to Alzheimer’s and Parkinson’s, and there is no known cause or cure. The progress of Lewy body disease can be rapid. Symptoms can include hallucinations, fluctuations in mental state, stiffness and physical tremors. Treatment focuses on the use of drugs to relieve symptoms.
The following are some of the causes of LBD:
- Genetics: LBD can sometimes run in families, and some genetic mutations have been linked to an increased risk of developing the condition.
- Age: Lewy body dementia is more common in people over the age of 60, although it can occur in younger people as well.
- Environmental factors: Exposure to certain toxins or chemicals may increase the risk of developing LBD.
- Other medical conditions: People with certain medical conditions, such as Parkinson's disease or REM sleep behaviour disorder, may have a higher risk of developing LBD.
- Brain injuries: Traumatic brain injuries have been associated with an increased risk of developing LBD.
- Imbalances in brain chemicals: Imbalances in certain brain chemicals, such as dopamine, acetylcholine, and serotonin, may play a role in the development of LBD.
Watch - ‘Lewy Body Disease - Robin and Lis’ by Dementia Australia
Learn more about Lewy body disease by watching the following video:
Use the following documentation tool to list the symptoms of Lewy body and the ways you can support someone with Lewy Bodies as a support worker.
Korsakoff’s Syndrome
Excessive intake of alcohol over a long period of time damages the brain and can result in the person developing Korsakoff’s syndrome (also known as Wernicke-Korsakoff syndrome), which is one of the forms of dementia that affects younger people.
Its causes include:
- Direct toxic effects of alcohol on the brain: Long-term heavy alcohol use can cause damage to the brain cells, leading to cognitive impairment and memory loss.
- Nutritional deficiencies: Alcohol can interfere with the absorption of certain vitamins and minerals, such as thiamine, which is essential for brain function. Chronic alcohol use can lead to malnutrition and thiamine deficiency, which can contribute to the development of dementia.
- Liver disease: Long-term heavy alcohol use can cause liver damage and impair its ability to remove toxins from the body, leading to further damage to the brain.
- Cardiovascular disease: Chronic heavy alcohol use can increase the risk of cardiovascular disease, which can lead to reduced blood flow to the brain and contribute to the development of dementia.
- Other lifestyle factors: Individuals who abuse alcohol may also have other unhealthy lifestyle factors, such as poor diet and lack of exercise, which can further increase their risk of developing dementia.
Activity - Watch
The following video describes Wernicke Korsakoff Syndrome and its causes. Pay particular attention to the symptoms and the effective treatment.
Frontotemporal Dementia
Frontotemporal dementia (FTD) is caused by damage to the frontal and/or temporal lobes of the brain, which govern self-control, mood, social skills, attention, planning and judgement. FTD results in changes to thought processes, emotions and personality.
Here are some of the known causes and risk factors for FTD:
- Genetic factors: Some cases of FTD are caused by mutations in certain genes, such as the MAPT, GRN, and C9orf72 genes. These mutations can lead to the abnormal accumulation of proteins in the brain, which can cause damage to the brain cells and lead to the development of FTD.
- Environmental factors: There is some evidence to suggest that exposure to certain environmental toxins, such as pesticides, may increase the risk of developing FTD.
- Age: FTD typically occurs in individuals between the ages of 45 and 65, although it can occur at any age.
- Gender: FTD appears to be slightly more common in men than in women.
- Family history: Individuals with a family history of FTD or other neurodegenerative disorders may be at increased risk of developing the disease.
- Brain injury: There is some evidence to suggest that a history of traumatic brain injury may increase the risk of developing FTD.
- Neuroinflammation: Inflammation in the brain, which can be caused by a variety of factors, may contribute to the development and progression of FTD.
Symptoms can appear when a person is in their fifties or sixties, including personality changes and the loss of language skills. There is a genetic component in about 10–15% of cases, but this is not yet properly understood.
Activity - Watch
Watch this report by 60 minutes on frontotemporal dementia or FTD, the most common form of dementia among people under 60.
Huntington’s Disease
Huntington’s disease is a progressive disease that often results in premature death, but it can take between 10 and 30 years to progress to a fatal state. It is characterised by uncontrollable, jerky body movements (known as chorea), which can resemble dancing. It is a brain disease that affects the nervous system. Other symptoms include apraxia, which means that the person is unable to perform familiar movements; deterioration in memory, cognitive processes, judgment and the ability to plan and organise; and the loss of control over bodily functions. Huntington’s disease is genetically transmitted. Children of an affected parent have a 50% chance of inheriting the gene, developing the disease and/or transmitting it to their own children. It can appear at any age, but most commonly presents symptoms in a person’s forties and fifties. It is thought that the related gene interferes with the body’s ability to manufacture a protein that is essential for normal brain development. There is no cure or treatment to stop or reverse the progress of Huntington’s disease. Other common causes include:
- Toxic effects of the mutant protein: The mutant huntingtin protein can accumulate in the brain cells, disrupting their normal function and leading to their degeneration and death.
- Interference with normal cellular processes: The mutant protein can interfere with the normal cellular processes, such as regulating gene expression and transporting proteins within the cells.
- Neuroinflammation: The accumulation of the mutant protein can trigger an inflammatory response in the brain, leading to further damage and cell death.
- Genetic and environmental factors: While a genetic mutation causes HD, there is evidence that environmental factors may also play a role in the development and progression of the disease.
Activity - Watch
The following video produced by Huntington’s disease youth organisation explains facts about the disease. Pay particular attention to symptoms and think about how this may effect the support you provide someone with Huntington’s disease.
Parkinson’s Disease
Parkinson’s disease is a neurological condition that affects movement and balance. It occurs in about one to two people in a thousand, increasing to one in a hundred in people over the age of 60. Research shows Parkinson’s disease causes the death of nerve cells that produce dopamine in the brain, which results in difficulty controlling muscle tension and movement, which then leads to muscle tremors, rigid limbs, loss of balance and difficulty walking.
The following are potential, but clear causes of Parkinson’s Disease:
- Genetic factors: Although most cases of Parkinson's disease are not inherited, there are some genetic mutations that can increase the risk of developing the disease. For example, mutations in the LRRK2, SNCA, and Parkin genes are known to be associated with increased risk of PD.
- Environmental factors: Exposure to certain toxins, such as pesticides and herbicides, has been linked to an increased risk of developing Parkinson's disease. It has also been suggested that head injuries, particularly those that involve loss of consciousness, may increase the risk of PD.
- Age: Parkinson's disease is more common in older adults, with the risk increasing significantly after the age of 60.
- Gender: Parkinson's disease appears to be slightly more common in men than in women.
- Family history: Individuals with a family history of Parkinson's disease may be at increased risk of developing the disease.
- Neuroinflammation: Inflammation in the brain may contribute to the development and progression of Parkinson's disease.
Watch - ‘2-Minute Neuroscience: Parkinson’s Disease’ by Neuroscientifically Challenged
Learn more about Parkinson’s disease by watching the following video:
Young-Onset Dementia
Young-onset dementia is any form of dementia that occurs in a person under the age of 65. Dementia can occur in a person as young as 30 and is most commonly the result of Alzheimer’s disease, vascular dementia or frontotemporal dementia.
Causes of young onset dementia include:
- Infections: Certain infections, such as HIV/AIDS, can cause damage to the brain that may lead to the development of dementia.
- Substance abuse: Long-term alcohol or drug abuse can damage the brain and increase the risk of developing dementia.
- Cardiovascular disease: Cardiovascular disease, including high blood pressure, high cholesterol, and diabetes, can increase the risk of developing dementia.
- Environmental factors: Chronic stress, Exposure to environmental toxins, such as lead, can increase the risk of developing dementia.
- Lifestyle factors: Unhealthy lifestyle factors, such as a poor diet, lack of exercise, and smoking, can increase the risk of developing dementia.
The impact of dementia in a relatively early stage of life can be traumatic and can have economic and social implications different to those caused by dementia in a later stage of life. Progressive disease and symptoms vary according to the type of dementia but can include memory loss and difficulties with thought processes, communication and functioning within the home or community. Management of the disease also varies.
Watch - ‘Living With Young-Onset Dementia’ by Financial Times
Watch the following video to learn how young-onset dementia can affect a person’s life:

Each individual will experience dementia and its progression differently. For some people, progression is rapid, while for others, it develops more gradually. According to the Alzheimers association people with Alzheimer's usually live 4 to 8 years after diagnosis, but some may live up to 20 years, depending on different factors. Alzheimer 's-related brain changes start years before symptoms show up, called the preclinical phase, which can last for several years.
There are different models that detail the progression of dementia: a three-stage model, a four-stage model and a seven-stage model. Be aware that it may be difficult to place a person with Alzheimer's in a specific stage as stages may overlap.
These are the commonly recognised stages or phases in the three-stage model:
Stage 1: Early-Stage Dementia
Memory lapses characterise the first stage and having difficulty finding words (mild cognitive impairment). The onset of these symptoms can be gradual and may be recognised only as the disease progresses further. Many people continue to function independently at this stage, but symptoms begin to affect their daily lives and activities in the following ways:
The following are examples of early-stage dementia:
- Short-term memory loss and forgetting recent events
- Getting lost, forgetting where they are and what they are doing; and misplacing objects
- Difficulty problem-solving and completing complex tasks, and the loss of other skills
- Trouble expressing themselves and organising their thoughts, losing track of conversations and repeating themselves
- Personality changes, for example, withdrawing, interacting less, losing interest in activities and in engaging with people, becoming irritable, being reluctant to try new things and becoming more self-centred and easily upset
- Difficulty managing bills and money.
Stage 2: Moderate Dementia
This stage, typically the longest stage, can last for many years. Memory loss worsens, and individuals may struggle with familiar tasks, communication, and orientation. Assistance with daily living activities may be required as the following symptoms become more pronounced:
The following are examples of moderate dementia:
- More forgetful – Recall of past events remains, but they forget names of familiar people such as family members and confuse the identities of different people; they may leave the gas turned on or forget to remove pans from the stove when cooking
- More confused about where they are and what time or day it is
- More likely to behave inappropriately and overlook social norms and conventions
- More likely to neglect personal care and forget to eat or drink regularly
- More frustrated, agitated and distressed
- More likely to see and hear things that are not there and to become suspicious and hostile
- Having trouble controlling their bladder and bowels.
- Experiencing changes in sleep patterns, such as sleeping during the day and becoming restless at night.
- Showing an increased tendency to wander and become lost.
Stage 3: Advanced (Severe) Dementia
In the third stage, the person’s physical and mental condition declines further. Dementia begins to affect the person’s physical capabilities and individuals lose the ability to respond to their environment, to carry on a conversation and, eventually, to control movement. They may still say words or phrases, but communicating becomes difficult. As memory and cognitive skills continue to worsen, significant personality changes may take place and individuals need extensive care.
The following are examples of advanced dementia:
- Loss of the ability to communicate
- Being unable to recall things for even a short time (a few minutes) or recognise family and friends, and being unable to recognise familiar everyday objects
- Loss of mobility, becoming bedridden towards the end of life
- Increasing restlessness at night and disturbed sleep
- Becoming increasingly hostile and aggressive
- Losing touch with reality, for example, searching for a long-dead relative
- Incontinence and loss of control over bodily functions
- Increased susceptibility to infections.
Read more information on the stages of dementia.
Activity - Quiz
Answer the following multiple-choice questions about the stages of dementia.
