In this topic, we will investigate the nutrition guidelines for babies and toddlers, preparing and monitoring meals and following good food hygiene. We will also look at ways educators can encourage parental involvement in feeding, and ideas for creating positive mealtimes at the service.
By the end of this topic, you will understand:
- Nutrition and meal regulatory requirements
- Supporting parental involvement in feeding
- Properly preparing and monitoring meals
- Food hygiene regulations and practices
- Creating positive mealtimes.
Nutrition and eating contribute greatly to the health of babies, toddlers and children. Educators need to be knowledgeable about nutrition as well as food hygiene in order to support and guide children in their care.
National Quality Standard (NQS) 2.1 ‘Health’ and the elements within it outline specific standards related to nutrition and eating at services to ensure that all educators:
- Are familiar with current guidelines about healthy eating
- Understand and implement correct procedures relating to food handling, transportation and storage
- Ensure all children’s nutritional and dietary health needs are met in relation to food and beverages offered at the services, including when the service implements excursions and events.
Use the curriculum as an opportunity to educate and collaborate with children on getting nutrition and leading a balanced, healthy lifestyle. Education and care services are required to provide children with regular nutrition-based meals to meet the physical and developmental requirements of each individual child.
Services should follow the guidance of the:
- Education and Care Services National Regulations
- National Quality Framework and National Quality Standard
- Australian Dietary Guidelines
The Education and Care Services National Regulations provide clear details on expectations regarding nutrition and food preparation for services:
- Regulation 77 – Health, hygiene and safe food practices
- Regulation 78 – Food and beverages
- Regulation 79 – Service providing food and beverages
- Regulation 80 – Weekly menu
Think
NQS Quality Area 2 – Children’s health and safety, Element 2.1.3 ‘Healthy lifestyle’ states ‘Healthy eating and physical activity are promoted and appropriate for each child’. Consider how services can ensure the implementation on Element 2.1.3 in their services.
The Australian Dietary Guidelines provide clear recommendations for nutrition and meal requirements for babies, toddlers and children.
To assist your understanding of the nutritional requirements for children specifically, you will need to be aware of:
- Australian dietary guidelines 1–5
- Recommended food groups
- Serving suggestions and sizes.
The Australian Guide to Healthy Eating is a food selection guide that visually represents the proportion of the five food groups recommended for consumption each day. It also emphasises the need to drink plenty of water throughout the day.

For recommendations for children from birth to two years, access the Eat for Health: Infant Feeding Guidelines Summary by the National Health and Medical Research Council (NHMRC) and the Department of Health and Aging, published on the Eat for Health website. The Infant Feeding Guidelines provide advice and recommendations on breastfeeding, the introduction of solids, preparing infant formula and other common health-related concerns.
The Guideline contains the following recommendations:
- Breastfeeding is the healthiest start for infants.
- Cow’s milk should not be given as the main drink to infants under 12 months. However, small amounts may be used in the preparation of solid foods.
- Exclusively breastfed infants do not require additional fluids up to 6 months of age.
- Introduce solid foods at around 6 months to meet the infant’s increasing nutritional and developmental needs.
- Ensure that solid foods are of appropriate texture. The texture of foods that are introduced should be suited to an infant’s developmental stages, moving from pureed to lumpy to normal textures during the 6-12-month period.
- Do not add sugar or honey to infant foods as this increases the risk of dental caries.
- Avoid juices and sugar-sweetened drinks. Limit intake of all foods with added sugars.
- Do not add salt to foods for infants. This is an important safety issue as infants' kidneys are immature and unable to excrete excess salt.
Australian dietary guidelines (1-5)
The recommendations made by the Australian Dietary Guidelines are grouped around five (5) guidelines:
| Guideline 1 | To achieve and maintain a healthy weight, be physically active and choose amounts of nutritious food and drinks to meet your energy needs. |
| Guideline 2 | Enjoy a wide variety of nutritious foods from these five groups every day:
|
| Guideline 3 | Limit intake of foods containing saturated fat, added salt, added sugars and alcohol.
For women who are pregnant, planning a pregnancy or breastfeeding, not drinking alcohol is the safest option. |
| Guideline 4 | Encourage, support and promote breastfeeding |
| Guideline 5 | Care for your food; prepare and store it safely |
Food labels
In Australia, food producers must comply with the labelling requirements of the Food Standards Code.
Food labels are included on all food products, except for very small packets and fresh foods like fruit, vegetables and local bakery or organic products.
Food labels:
- tell you what ingredients and/or additives are in the food
- give you nutritional information about the food and food storage instructions
- tell you who manufactured the food.
Always read the food label to be aware of whether the food contains any saturated fat, added salt or sugar. Food labels also contain critical information to avoid foods that will agitate allergies.
Nutritional information panels (NIPs) are a part of the food label. These tell you what nutrients the food contains and how much of each nutrient there is.
When you buy a packaged food product, have a look at the back of the packet. You should be able to see a box with a heading like ‘Nutritional information’.
Under the heading, you’ll see categories like:
- serving size
- energy
- protein
- fat
- carbohydrates
- sugars
- salt
- dietary fibre
- sodium.
All foods have to list seven food components on their nutritional information panels – energy (kilojoules), protein, total fat, saturated fat, total carbohydrates, sugars and sodium. Manufacturers might decide to include other nutrients too, including fibre and calcium.
Comparing the nutritional information on different food products helps you work out the healthiest choice. The healthiest choices have lower saturated fat, lower sodium, lower sugar and higher fibre.
When you’re comparing two products, look at the ‘per 100 gm’ or ‘per 100 ml’ information on each, rather than the ‘per serving’ information. This way, you can compare the same thing on each product.
Many foods contain food additives. There are strict guidelines about the way food additives are used in foods and labelled on food products. All food additives must be shown on the ingredient list – for example, thickener (1442). The label must say if an additive is based on a potential allergen – for example, wheat thickener (1442).
You can get a list of food additive names, numbers and common uses from Food Standards Australia New Zealand – Additives.
When reading a food label, keep in mind that the label must be read every time, as manufacturers may change ingredients on the foods you regularly consume. Precautionary Allergen Labels (PAL) are more commonly known as “may contain” statements. However, be aware; they are currently voluntary.
For example, children with known nut allergy must not have any product that ‘may contain traces of peanuts’ as this may trigger an allergic or even anaphylactic reaction.
Nine (9) foods cause 90% of all food allergic reactions: peanuts, tree nuts, shellfish, fish, cow’s milk, eggs, soybeans, sesame and wheat. If these ingredients are in a food product, manufacturers must say so, no matter how small the amount.
The information can be stated in a few different ways.
For example, if you’re checking a product for egg, you might see:
- albumin (egg)
- egg albumin
- contains egg – at the end of the ingredient list
- sugar, chocolate, eggs – in bold type in the ingredient list.
Look at the following food label:
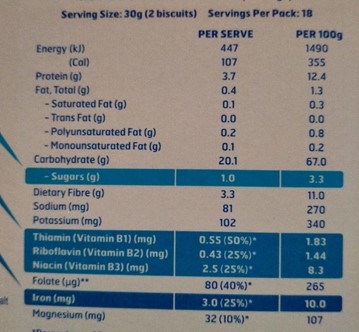
According to the food label, the product:
- is low in saturated fat (0.1 g per serve)
- is low in sugars (1 g per serve)
- contains 20.1 g carbohydrate per serve which a typical carbohydrate intake for a meal.
All foods with a shelf life of less than two years must have a date on them that tells you when the manufacturer advises the food will either be unsafe to eat or not as good to eat:
- Use by is for perishable foods like meat, fish and dairy. This is the date that tells you when a food is ‘off’. It’s illegal for shops to sell food past its ‘Use by’ date.
- Best before tells you the date when the food will still be safe to eat but might not be of the best quality anymore.
- Baked on or packed on is the date the food was manufactured or packed. This tells you how fresh it is. You might see this on foods like bread and meat.
You can read more information about food labels on Raising Children Network.
Check your understanding
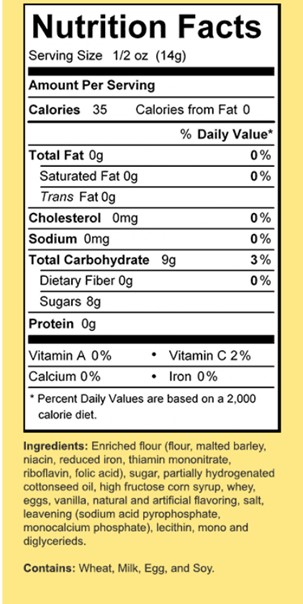
Look at the following food label and decide if a child who is allergic to gluten, lactose and egg can have the product:
Providing nutrition to children
Early childhood services will provide the following mealtimes for children:
- Breakfast
- Morning tea
- Lunch
- Afternoon tea
- Late snack
The time frames of these mealtimes will vary from room to room and service to service, but services should ensure children have access to food regularly, presenting food every two hours.
Kindergartens/Preschools and family day care services may have families providing their own food and lunch boxes.
Educators are still responsible for monitoring the food entering the service and the nutrition the child is receiving.
Nutrition for babies

There are three (3) very important considerations when it comes to nutrition for babies:
-
Exposure to food
Babies under one year should not be exposed to:
- Full-cream milk
- Honey
- Water that has not been sterilised (i.e. boiled and cooled)
- Any food products that have not been tested by families at home to prove they cause the baby no allergic responses.
-
Liquids not recommended
Any liquid other than milk and water is not recommended for babies. If a baby is around 6 months old, they can be offered small amounts of boiled and then cooled tap water, but you should not replace their breastmilk or formula feeds. Breastmilk or formula should still be their main drink up to 12 months of age.9
After 12 months, their main drink should be water and cow's milk or breastmilk. You can offer water or milk in a cup. There's no need to boil tap water once your baby has reached 12 months.
-
Appropriate foods
For babies six months to one year who are starting on solid foods, ensure the texture of the food is suitable for the baby’s stage of development (e.g. pureed for six-month-olds and lumpy for one-year-olds).
Follow each individual child’s needs in collaboration with families.
- Under six months: Babies under six months should have breast milk or infant formula only.
- Over six months: At six months, babies typically start on solid foods, which are introduced one at a time to monitor any potential allergies.
Nutrition for toddlers

By one year, toddlers have typically been introduced to a range of solid foods. It is important for them to eat foods from the five food groups every day.
The five (5) food groups are:
- Grain (cereal) foods, mostly wholegrain and/or high cereal-fibre varieties
- Vegetables and legumes/beans
- Fruit
- Milk, yoghurt, cheese and/or alternatives, mostly reduced fat
- Lean meats and poultry, fish, eggs, tofu, nuts and seeds, and legumes/beans.
The recommended servings per day of each food group for toddlers and pre-schoolers are as follows:
- Vegetables and legumes/beans: Most Australians eat only half the recommended quantity of vegetables every day. For children aged two to three years, two and a half servings per day are recommended (one serving = half a cup for most vegetables, one cup for leafy greens and salads).
- Fruit: Toddlers should have limited fruit juice. However, eating whole fruit is important. Children aged two to three should have one serving of fruit per day.
- Grain (cereal) foods: Whole grains are more nutritious than cereal grains that have added fat and sugar. Children aged two to three should have four servings of grains per day (one serving = one slice of bread or three medium-sized chips).
- Milk, yoghurt, cheese and/or alternatives: This includes dairy alternatives. Dairy is required mainly for its calcium, but there are non-dairy foods, such as salmon, sardines and almonds, that also have high amounts of calcium. Children aged two to three should have one and a half servings of dairy per day.
- Lean meats and poultry, fish, eggs, tofu, nuts and seeds, and legumes/beans: This food group also includes meat alternatives, such as nuts, eggs and tofu. Children aged two to three should have one serving of meat, fish or an alternative per day.
Note
Children should have plenty of water every day. Australian tap water is ideal for children one year and older.
Keep the following considerations in mind when feeding toddlers:
- Foods to avoid: Avoid foods that pose a choking hazard, such as very dry foods, seeded foods, hard or chewy foods, and foods to which a child has yet to be exposed.
- Milk and water: It is not recommended to continue using a baby’s bottle for children over the age of 12 months old. Instead, offer milk and water in a cup or sippy cup. Ensure children are drinking water throughout the day and after meals to clean any sugar off their teeth.
- Supervision: Always supervise children eating. Toddlers are learning to feed themselves, and choking is a higher risk than with older children.
- Appropriate foods: Foods should be consistent with the Australian Dietary Guidelines.
Mealtimes and progressive practices
Mealtimes include breakfast, morning tea, lunch, afternoon tea and late snack. Progressive mealtimes are when you plan meals to take place over a set time frame (e.g. an hour) to allow children to choose when they are ready to join in and eat.
WATCH
Watch the following 3-minute video for more on mealtime practices:
Key points
As an early childhood educator, it is important that you stay up to date on the latest Education and Care Services National Regulations.
Regulations 79 (Service providing food and beverages) and Regulations 80 (Weekly menu) provide helpful considerations for early childhood educators to keep in mind when mealtime planning:
| Regulations 79 | Service providing food and beverages |
|---|---|
| (1) | The approved provider of an education and care service that provides food or a beverage to children being educated and cared for by the service must ensure that—
(a) the food or beverage provided is nutritious and adequate in quantity; and (b) the food or beverage provided is chosen having regard to the dietary requirements of individual children taking into account— (i) each child’s growth and development needs; and (ii) any specific cultural, religious or health requirements. Penalty: $2000. |
| (2) | A nominated supervisor of an education and care service that provides food or a beverage to children being educated and cared for by the service must ensure that—
(a) the food or beverage provided is nutritious and adequate in quantity; and (b) the food or beverage provided is chosen having regard to the dietary requirements of individual children taking into account— (i) each child’s growth and development needs; and (ii) any specific cultural, religious or health requirements. Penalty: $2000. |
| (3) | A family day care educator who provides food or a beverage to children being educated and cared for by the educator as part of a family day care service must ensure that—
(a) the food or beverage provided is nutritious and adequate in quantity; and (b) the food or beverage provided is chosen having regard to the dietary requirements of individual children taking into account— (i) each child’s growth and development needs; and (ii) any specific cultural, religious or health requirements. Penalty: $2000. |
| (4) | To avoid doubt, this regulation does not apply to food or a beverage provided by a parent or family member for consumption by the child. |
| Regulations 80 | Weekly menu |
|---|---|
| (1) | The approved provider of an education and care service that provides food and beverages (other than water) to children being educated and cared for by the service must ensure that a weekly menu—
(a) is displayed at a place at the education and care service premises accessible to parents of children being educated and cared for by the service; and (b) accurately describes the food and beverages to be provided by the service each day. Penalty: $1000. |
| (2) | A nominated supervisor of an education and care service that provides food and beverages (other than water) to children being educated and cared for by the service must ensure that a weekly menu—
(a) is displayed at a place at the education and care service premises accessible to parents of children being educated and cared for by the service; and (b) accurately describes the food and beverages to be provided by the service each day. Penalty: $1000. |
| (3) | A family day care educator who provides food and beverages (other than water) to children being educated and cared for by the educator as part of a family day care service must ensure that a weekly menu—
(a) is displayed at a place at the family day care residence or approved family day care venue accessible to parents of children being educated and cared for by the service; and (b) accurately describes the food and beverages to be provided by the family day care educator each day. Penalty: $1000. |
| (4) | To avoid doubt, this regulation does not apply to food and beverages provided by a parent or family member for consumption by the child. |
Encouraging healthy eating in early childhood services
The following guidelines are useful to ensure that children in your care are meeting their dietary requirements and learning a healthy attitude to food:
- Limit the types of snack foods provided. Children engage in snacking multiple times across the day. For toddlers, snacking is usually their preferred option, as they are always on the move. Make sure, when offering snacks, you consider low-sugar options, such as veggie sticks, fruit, yoghurt or cheese, or crackers and dip.
- Limit sugary drinks. In an early childhood service, children will be offered milk and water only as per the recommendation of the Australian Dietary Guidelines. When collaborating with families, ensure to encourage reducing the number of sugary drinks that children are offered. This includes fruit juices and drinks, flavoured milk and soda.
- Do not use food as a motivator. Food is a basic right of every child. Food should be offered throughout the day and provided when the child is hungry, even around planned mealtimes. It is never appropriate to use food as a means of bribery or punishment.
- Use intentional teaching. Look for opportunities to discuss with and teach children the importance of food and nutrition to our growth and wellbeing. Plan experiences that explore this.
- Role model healthy eating. When children are eating, sit with them and eat the same food. Role model trying new foods, talking positively about food and enjoying the mealtime experience.
Childhood obesity
Childhood obesity is when a child has too much body fat for their age. Being overweight and living with obesity are common in Australia, affecting 1 in 4 Australian children.
Children living with obesity generally have a body mass index (BMI) at the 95th percentile or higher for their age group.
Helping a child or teenager maintain a healthy weight means they’re less likely to struggle with weight problems as adults. You can help manage obesity in children by modelling healthy eating habits with them, encouraging lots of physical activity and limiting screen time.
The most visible sign of obesity is excess body fat, but it’s not always easy to tell if your child is living with obesity or overweight.
A child is healthiest if they stay within a certain weight range for their age known as a ‘BMI-for-age’. A BMI-for-age score between the 85th and 95th percentile may mean that your child is overweight. A score at the 95th percentile or higher may indicate they are living with obesity.
You can use NSW Health’s healthy weight calculator to estimate your child’s BMI for age.
Some causes of obesity and excessive weight gain may be outside your control, such as the way their body works (for example, your child’s metabolic rate — how quickly their body uses energy), their lifestyle and their environment.10
Risks of childhood obesity include diabetes, high blood pressure and high cholesterol. Childhood obesity can also lead to poor self-esteem and depression.
Food allergies

A food allergy occurs when the immune system reacts to a food which is usually harmless. If you, or someone in your care, has a severe allergic reaction (anaphylaxis), call triple zero (000) for an ambulance. The person having the reaction should not stand or walk. An educator with a current First Aid certificate must administer an adrenaline (epinephrine) injector (such as EpiPen® or Anapen®) into outer mid-thigh.
Food intolerance occurs when the body has a chemical reaction to eating a particular food or drink.
The symptoms for mild to moderate food allergy or intolerance may sometimes be similar, but food intolerance does not involve the immune system and does not cause anaphylaxis.
Symptoms of food intolerance can include:
- nervousness
- tremor
- sweating
- palpitations
- rapid breathing
- headache, migraine
- diarrhoea
Signs of anaphylaxis (severe allergic reaction):
- difficult or noisy breathing
- swelling of tongue
- swelling or tightness in throat
- wheeze or persistent cough
- difficulty talking or hoarse voice
- persistent dizziness or collapse
- pale and floppy (young children).
Early childhood services will need to manage a range of food allergies within each room. It is important for service management, educators, families and the service chef to collaborate and develop a plan to ensure each child’s individual needs are met. The plan should engage in inclusive practices and make the children feel welcome at each mealtime. Also, you must learn to read food labels so you can avoid foods that cause allergic reactions. If you have a child with known severe food allergy, it is advisable to always check the food label as ingredients may slightly change over time and the food that used to be safe, could contain traces of allergens.
When a child enrols at a service, or when a food allergy has been diagnosed by a doctor, the family will need to provide a copy of the child’s allergy plan. This plan will be placed in the child’s room and given to the centre chef. The chef will then provide meals or alternative meals to ensure the child is not exposed to the allergen. The child’s food will be delivered to their room in a separate bowl or container with the child’s full name on it.
Educators are encouraged to serve this food first and supervise the child during mealtime to ensure the child is not sharing food with or from others.
Every service will develop policies and procedures that will outline how to manage children’s individual food allergies. This will include implementing the child’s allergy management plan and training all staff that have a responsibility to care for that child.
Ensure you are aware of the children at your service with allergies and take serious precautions to avoid exposure to allergens. You will need to learn about and be able to identify food allergy symptoms and be prepared to act swiftly (for further information about food allergies see section 8.4). Both permanent and casual educators should be briefed on risk minimisation strategies for children with food allergies and emergency procedures when something goes wrong.
Unfortunately, allergies are on the increase worldwide and food allergies have also become more common. Most allergies appear during the first year of life. Cow’s milk allergy is one of the most common in early childhood. Most children grow out of cow’s milk allergy before they start school.
Peanuts, tree nuts, eggs, cow’s milk, wheat, sesame, fish, shellfish and soy cause the majority of food allergic reactions. Peanut allergy is one of the most common allergies in older children as only approximately one in 4 children will outgrow peanut allergy.
The foods that tend to cause intolerance reactions in sensitive people include:
- dairy products, including cow’s milk, cheese and yoghurt
- chocolate
- eggs, particularly egg white
- flavour enhancers such as MSG (monosodium glutamate 621)
- food additives
- strawberries, citrus fruits and tomatoes
- wine, particularly red wine
- histamine and other amines in some foods.
You should only avoid foods to which you have a diagnosed allergy. Learn the terms used to describe these foods on food labels, for example:

- milk protein – milk, non-fat milk solids, cheese, yoghurt, caseinates, whey, lactose
- lactose – milk, lactose
- egg – eggs, egg albumen, egg yolk, egg lecithin
- gluten – wheat, barley, rye, triticale, wheat bran, malt, oats, cornflour, oat bran
- soy – soybeans, hydrolysed vegetable protein, soy protein isolate, soy lecithin
- salicylates – strawberries, tomatoes.
You can read more about food allergies and intolerance on the Better Health Channel.
As it is explained on Community Early Learning Australia’s (CELA) website, Allergy & Anaphylaxis Australia has some helpful resources, including posters you can purchase or print.
The following resources will assist you in developing risk minimisation strategies and managing allergic reactions if they happen.
- Allergy Management – Schooling & Childcare
- Allergy & Anaphylaxis Australia Free digital resources
- Allergy Management: 3-5 years
- Allergy Management: 0-3 years
- Allergy & Anaphylaxis Australia has a helpline 1300 728 000
- Allergy & Anaphylaxis Australia website
- Allergy & Anaphylaxis Australia Facebook page
- Jeremy’s Cake - animated storybook
- How to give an EpiPen® animation
Creating a meal plan:
Under the Education and Care Services National Regulations, an approved provider must ensure that policies and procedures are in place for nutrition, food and beverages, and dietary requirements (regulation 168) and take reasonable steps to ensure those policies and procedures are followed (regulation 170).
The Education and Care Services National Regulations require approved providers, nominated supervisors and family day care (FDC) educators to ensure:
- adequate health and hygiene practices, as well as safe practices for handling, preparing and storing food (regulation 77)
- that children have access to safe drinking water at all times and are offered food and beverages appropriate to each child’s needs on a regular basis throughout the day (regulation 78)
- the food or beverages provided are nutritious and adequate in quantity and chosen based on each child’s dietary requirements (accounting for their growth and development needs, as well as any specific cultural, religious or health requirements) (regulation 79)
- a weekly menu is displayed and accessible to family members, which accurately describes the food and beverages to be provided by the service each day (regulation 80).
When creating a meal plan, services should consider the following:
- Australian dietary guidelines
- Children’s age group and individual dietary requirements
- Children’s individual dietary restrictions and allergies
- Current season. Services usually have a summer menu and a winter menu with incorporated seasonal fruits and vegetables.
- The menu should include a variety of meals from different cultures and a variety of tastes, colours, textures and flavours, representing the families attending the service. Where possible, families can provide their favourite family recipes to promote diversity and inclusivity within the service.
- Main meals should not be repeated in the two-week menu cycle, and the main ingredient in a meal should not be repeated on the same day each week.
There are many online tools that can help create a menu based on dietary guidelines, such as:
Example
View the following sample menus for reference:
- Littlle.ly Early Learning Centre’s sample menu
- Sample menu published by the Victorian Health Department.
- Kookaburra Childcare Centre’s menu available online
- Little Grace's Childcare Centre’s menu available online
Check your understanding

Encouraging parental involvement in feeding includes supporting mothers who are breastfeeding and providing families with up-to-date feeding information.
The NQS includes a requirement for educators to update families on their child's food and drink intake. In fact, it goes further than that and recognises that educators play a key role in supporting breastfeeding and also religious and cultural practices related to food.
Keeping families involved
The NQS requires services to demonstrate that families are being provided with daily information about their child's intake of and experiences with food and drink.
Educators have an important role to play in keeping parents involved in the feeding and nutrition of their children while they are in the service. Open communication with parents helps educators consciously contribute to the child's total daily nutrition intake.
How to share information with families:
- Note down what and how much the child ate on the service’s software tracking system or daily checklist.
- Talk to the parents about feeding practices on arrival and collection of the child.
- Ensure the team is communicating about the daily intake of each child.
Supporting breastfeeding
The Eat for Health: Infant Feeding Guidelines: Summary states, ‘Australia is a nation in which breastfeeding is protected, promoted, supported and valued by the whole of society. Breastfeeding provides major public health benefits.’
As an educator, part of your role is to uphold and reinforce the infant feeding guidelines at your service.
There are many ways by which you can encourage mothers to breastfeed, and you should support them to do so using the following practices:
- Use encouragement. Encourage and support breastfeeding until the baby is six months of age. However, it is recommended breastfeeding continue from six months to one year and beyond. Ensure mothers feel welcomed and affirmed
- Encourage continued breastfeeding alongside providing solids. Advise continued breastfeeding until at least 12 months of age while introducing complementary foods.
- Promote community services. Support families to be aware of community-based services that support breastfeeding.
- Encourage breastfeeding. Provide mothers with the choice to breastfeed at the service or bring expressed breast milk to care with their child. Ensure that the breastfeeding space is a private, comfortable space, with a chair, blankets, cushions, magazines and access to a drink.
- Respect decisions. Support and respect a family’s decision not to breastfeed a baby, and instead use infant formula. All mothers should be supported to breastfeed their child as long as they feel comfortable.
Check your understanding
Supporting religious and cultural practices
Many times, families will have certain feeding norms that are related to their religious or cultural practices. It is important that you take time to understand these practices and learn to support them as well as the Australian Dietary Guidelines.
When working with families, use the following tips for considering and supporting family values related to nutrition and feeding:
- Be informed. Have open discussions with families about any religious or cultural practices they follow relating to food and nutrition. Become informed and remain curious and open minded. Consider religious practices such as eating kosher or halal food, or observing Ramadan (although Muslim children do not fast for Ramadan, their family will likely be adhering to a different routine).
- Discuss special needs. If a child has specific needs related to eating, be sure to discuss the best way to approach this with the family. This may involve the family providing food from home.
- Consider Aboriginal traditional foods. All food has meaning in Aboriginal and Torres Strait Islander cultures. They believe that the land and all animals and plants were created by ancestral spirits of the Dreaming. Certain foods are referred to as ‘totems’, which are forbidden to be eaten except at special ceremonies.
- Be open to feedback. Regularly seek families’ feedback to ensure you understand their needs and preferences, then try to incorporate the feedback in the service’s daily practice.
Note
Remember, if you encounter a language barrier when communicating with parents, use an interpreter to ensure both you and they have clear lines of connection.
Food from home

While many services have policies that state families cannot bring food from home into the service, because of risk to children with food allergies, food can be brought into a service in some cases, such as:
- Family day care services – Families have to supply the food for their children for the day.
- Occasional care – Some occasional-care services require families to bring food for their children for the day.
- Kindergarten programs – These programs often have children ‘bring a lunch box’ during term 4 in preparation for school.
- Sessional kindergarten programs – Often these programs require children to bring their own lunchbox each session as meals and meal preparation are not provided at the service.
Note
Often, when food can be brought into the service, strict guidelines are in place to prevent any nuts and sometimes eggs from being brought into the service as these are common allergies.
The following tips address working positively with food brought from home:
- Encourage the food groups: Families should be encouraged to learn about the Australian Dietary Guidelines food groups and to bring foods that coincide with these, such as vegetables, fruit, grains and dairy. Often, we also encourage families to pack food in containers or sealed bags rather than using cling wrap and foil.
- Provide resources: Assist the parents’ journey in learning about appropriate foods. Make sure your service has a section with pamphlets about healthy and balanced eating. You can have fact sheets and handouts that you offer at the start of the year as well. The service’s website may have links to other websites and further information on healthy eating. Always be available to answer questions from families and refer them to a health professional if required. The Australian Guide to Healthy Eating is an excellent resource to share with parents.
- Clean water bottle: Assist children and families in getting into the habit of bringing a clean water bottle every day to the service. Often, services will keep the water bottle at the service. Water bottles should be easy for children to use: a child should be able to open the lid, drink, and fill the bottle up themselves if this is age appropriate.
Handling breast milk
It is important that babies receiving expressed breast milk at a service are given breast milk from only their own mother. Ensure that mothers are given information from your service on how to store, label and provide their breast milk. Always check that breast milk provided is properly labelled and stored in the refrigerator.
Babies can drink breast milk straight from the refrigerator; however, many prefer warm milk similar in temperature to an actual breastfeeding experience.
Follow these tips for safe breast milk handling and management:
- Store milk properly: Store labelled bottles standing up in the fridge.
- Keep records: Sign the baby's feeding record and follow your service's procedures for breast milk feeding.
- Never microwave breast milk: Breast milk should NOT be microwaved. This heats the milk unevenly (which can cause burns) and can destroy its natural benefits.
- Discard leftovers: Leftover milk should not be reused. Always discard it—never rewarm it later.
- Own mistakes: If you think a mistake may have been made and a baby may have been given milk from another mother, notify your director right away.
- Offer support: If a mother indicates she is having trouble continuing breastfeeding, offer support and provide options, such as the Australian Breastfeeding Association website and helpline (1800 686 268).
Refer to the Australian Breastfeeding Association website for advice on supporting breastfeeding.
Preparing breast milk
Follow these guidelines when you need to give a baby breast milk provided by the mother:
- Sterilise serving containers: Clean bottles and cups using a steriliser or by submerging them in boiling water for five minutes.
- Double-check names: If you are preparing breast milk for more than one baby, work with a colleague to ensure the name on the bottle matches the name of the baby to be fed.
- Use a bottle or cup: Breast milk should be offered in either a sterilised bottle (for babies six months and under) or a sterilised cup (for babies over seven months). Follow the choices of the family.
- Use a bottle warmer: Heat the milk using a bottle warmer.
- Check the temperature. Always check the temperature of the milk before giving it to the baby. You can do this by expressing a few drops on your wrist. Do not touch the teat to your body.
There are several guidelines for the storage of breastmilk that must be followed:
- All prepared breastmilk supplied by families must be stored in dated and labelled bottles in the fridge. They must be refrigerated at 5˚C or below and used within 24 hours.
- Time frames of storage:
- In freezer for up to 3 months if freezer is separate from the fridge
- In refrigerator (below 5 degrees Celsius) for 24 hours if previously frozen and thawed in refrigerator
- In refrigerator (below 5 degrees Celsius) for 4 hours if previously frozen and thawed outside a fridge in warm water
Note
If prepared bottles are provided by the family, then make sure the bottles have the child’s full name and you have discussed with the parent how and when they would like the bottle given to their child.
WATCH
Watch the following 2-minute video to learn about descaling an electric steriliser:
Preparing infant formula
If a baby is receiving infant formula instead of breast milk, it is likely you will need to prepare the formula.
Formula will come in a tin or a separate container provided by the parent. Store the formula in a dry, cool place, out of reach of children.
Place the bottle in the fridge standing up to avoid leaking and spills.
When preparing formula bottles, always begin by washing your hands, then follow these steps:
- Sterilise equipment: Sterilise the bottle, teats and caps in a steriliser or for five minutes in boiling water.
- Add water: Add water to the bottle (see formula instructions for correct amount). Always use boiled and cooled tap water (bottled water is fine if the container has not been previously opened).
- Measure and add formula powder: Always measure the amount of powder using a measured scoop (see formula instructions for correct amount), ensuring the scoop is levelled, then add the powder to the bottle.
- Shake and test: Shake the bottle (with the teat and cap on) until the powder dissolves, then test the temperature of the liquid on your wrist (it should be warm, not hot or cool).
As with breast milk, leftover formula should not be stored and reused. Discard it.
WATCH
Watch the following 2-minute video to learn more about preparing a baby bottle:
Monitoring mealtimes
Because babies and toddlers are just starting to learn to sit for meals and use utensils and are at risk of choking, they should always be closely supervised during eating.
Know the difference between gagging and choking:
- Babies and toddlers often gag with coughing, spluttering or spit-up while they are learning to eat and experiencing new textures in food. This is normal and not a cause for concern.
- Choking prevents breathing and is a medical emergency. You should be trained in first aid procedures for choking.
Educators are required to sit with children at all times during meals. Babies are placed in high chairs, and toddlers are on chairs at the table.
When monitoring mealtimes, keep the following considerations in mind:
- No propping. Never prop up bottles for babies or put babies in a cot with a bottle.
- Developmentally ready. It is important to contemplate whether introducing new foods or more texture to food is appropriate for the child. Make sure babies are developmentally ready to eat the solids being offered.
- Awake and alert. Make sure children are awake and alert when eating. If a child is sleepy or tired, do not force them to eat.
- Suitable texture. Start with solids that are smooth, and progress to foods with more texture. Grate, cook or mash hard foods such as apples and carrots before offering them to babies.
- No small and hard foods. Do not serve pieces of hard, raw fruit or vegetables, or foods such as nuts, popcorn or hard candy to babies and toddlers. Avoid sticky solid foods.
Supporting children with additional needs with feeding
Be aware of children in your service who have disabilities or a chronic illness with special needs during feeding. Depending on the children’s illness or disability, they may not be able to chew and swallow effectively.
Conditions and illnesses that may require support include:
- Cerebral palsy
- Down syndrome
- Brian injuries
- Sore throat
- Swollen tonsils.
Plan meals for children in a way that supports their needs, for example:
- Providing foods you know the child is able to chew and swallow
- Cutting food down to a size that the child is able to eat.
As a child with additional needs would be considered high risk when eating, educators will need to ensure they supervise the child closely during mealtimes. This would require an educator sitting next to or near the child and observing the child eat.
Food must be handled and prepared safely. Practices should be put in place and followed to ensure contamination does not happen.
Children are particularly at risk of illnesses caused by foodborne organisms and food contamination. As an educator, it is your responsibility to know and follow safe food handling procedures and practice good food hygiene.
Services need to comply with the following regulations around food safety as identified in the Education and Care Services National Regulations 2011:
- Regulation 77 – Health, hygiene and safe food practices
- Regulation 78 – Food and beverages
- Regulation 79 – Service providing food and beverages
DoFoodSafely is a great government initiative that allows you to complete a free, non-accredited food safety course. This is great for professional development and to extend your knowledge around safe food handling.
Food hygiene and contamination
Food contamination can be caused by a number of things, for example:
- Bacteria (particularly from dirty hands)
- Chemicals from the food production process (already on foods your service purchases) or from cleaning materials used
- Foreign bodies such as hair or small objects picked up during preparation
- Natural contaminants such as toxins
- Contamination from pests, such as flies.
Preventing food contamination
You can prevent food contamination by adhering to the following guidelines:
- Wash hands and wash fresh produce. Always ensure you thoroughly wash your hands before touching food for preparation or meals, and ensure children do the same. Hand washing is important to limit the spread of bacterial and viral germs. Wash fruits and vegetables with clean water before cutting and preparing them.
- Separate raw meats. Always separate raw meats from other food, and use separate utensils, knives and cutting boards when preparing meat. (These are often colour coded).
- Store foods at the correct temperature. Make sure food is kept at the correct temperature, particularly high-risk foods such as milk, meat and fish, and do not allow food to sit out for long periods, particularly during hot days.
- Clean prep tools. Be sure to prepare and serve food with tools that have been properly cleaned.
- Ensure personal hygiene. Be sure to wear proper personal protective equipment (PPE), such as gloves, when preparing food. Wash your hands before and after serving food. Do not prepare food if you are feeling unwell.
- Discard leftovers. Do not store and reuse food that was served at a table or from individual plates.
Additional practices for serving food safely:
- Use tongs and serving spoons to serve food.
- Reheat and re-serve appropriate foods only and do this just once. Discard leftover food after first reheat.
- During mealtimes, if the food is not being served, ensure it is covered.
Check your understanding
Mealtimes provide educators the opportunity to relax and socialise with the children and other educators. Mealtimes should be fun and engaging, and reflect having a table meal with families at home.
National Quality Standard Element 2.1.3 requires educators go beyond ensuring good hygiene and balanced nutrition. The Aussie Childcare Network suggests this can be achieved by creating ‘experiences, conversations and routines that promote relaxed and enjoyable mealtimes and promote healthy, balanced lifestyles’.
WATCH
Watch the following 1-minute video by Nutrition Australia to better understand the educator’s role in creating positive mealtimes:
Read the following article and consider the questions it poses:
- ‘Creating Positive Mealtimes’ from ACECQA's We Hear You
Check your understanding
Consider these mealtime strategies and how you could use them to improve the quality of mealtimes:
- Teach while cooking. Cooking and preparing food (including during make believe games and play) is an opportunity to teach children about healthy food choices and nutrition. Encourage children to be a part of preparing and setting up mealtimes where possible.
- Encourage social conversation. Allow children to lead the conversation at mealtime. Follow the lead of the children—engage and ask questions and share stories together.
- Do not use food bribery. Never use food to reward or punish children.
- Recognise a full stomach. Do not require children to eat everything on their plate or eat more than they need. Help them recognise when they are full or hungry. Respect their right to choose what foods they like and do not like while encouraging them to be explorative with food.
- Model mealtimes. Sit with children at mealtimes, and model healthy eating habits and nutrition practices.
- Ask children questions. Engage with children during mealtime: ask them what the food tastes like, what it feels like, what foods the children do and do not like to eat. Engage in social conversation as well. Make sure the mealtime is fun and engaging. This often means reflecting the children’s interest in play they have been involved with for the day.
Supporting positive food attitudes
Children often go through phases of being fussy or particular about certain foods.
The following guidelines will help you encourage fussy eaters to eat:
- Understand the child’s eating patterns. Understand the child’s eating patterns. Babies and toddlers will often snack in small doses throughout the day—you may need to alter your expectations for mealtimes and provide food more often throughout the day. Older children will often have foods they do and do not like, and will eat larger meals. Make these times enjoyable and involve the children in planning and preparing for mealtimes as well as making choices about their foods where appropriate.
- Avoid stress. Work with your colleagues to ensure that mealtimes are enjoyable and stress free. Support each other if someone is having a tough time and needs help.
- Do not give up. Continue to offer foods that have been refused before. Do not force the child, but do allow them to have another chance to try a particular food. Very often, children need multiple exposures to a new food before they will even taste it.
- Set a time limit. Set a time limit for a meal, and after that time remove any uneaten food. Allow the child to leave the table and do not offer alternative food until the next snack or meal. (This does not apply to babies.) Note: Some services will ask you to provide a sandwich as an alternative if a child refuses lunch.
Children and body image

Children often become aware of social preferences for body image at young ages. Educators can help children form a positive self-image by helping them learn to see food as important for a healthy body.
Use these tips to help children see food and eating in a positive way:
- Avoid discussion about weight. Make sure discussions about food are related to how the child feels, such as saying ‘This food will give you energy or make you feel strong’. Never address food in relation to appearance or body weight.
- Focus on nutrition. Make sure conversations about food are positive and focused on healthy nutrition. Do not label foods as ‘good’ or ‘bad’.
- Avoid diet talk. Do not talk about your own dieting or food restrictions with children or your colleagues, and never encourage children to restrict their food intake.
- Use the right praise. Promote positive body image by focusing on what children can do, instead of how they look (even if you feel it is a positive look).
Check your understanding
Use the following questions to check your knowledge. You can check the correct answer by clicking on the 'Answer' button:
-
List and describe the regulations that relate to food serving and food safety.
- Regulation 77 Health, hygiene and safe food practices
- Regulation 78 Food and beverages
- Regulation 79 Service providing food and beverages
- Regulation 80 Weekly menu
-
Detail the daily serving recommendations for a three-year-old for each food group.
- Meat - 1 serve
- Dairy - 1 and a half serve ,li>Vegetables- 2 and a half serves
- Fruit - 1 serve
- Grain - 4 serves
-
Describe the concept of progressive mealtimes.
It is children's free choice to join mealtime when they are ready within the scope of 1-2 hours. -
List one way a service may manage food allergies during mealtimes.
- Serving food in separate bowl or container with child's name on it
- Have allergy plans with pictures up on the wall
- Staff check allergy plans before serving food
- A child with an allergy gets served food first
- Supervise mealtime closely
-
Describe the area that should be set up for a breastfeeding mother. What should it include?
- A private room
- Couch
- Blankets
- Hot and cold drinks
- Music
- Privacy
-
List the steps for preparing a formula bottle for a child.
Always begin by washing your hands.- Sterilise. Sterilise the bottle, teats, and caps for 5 minutes in boiling water.
- Use boiled water. Always use boiled and cooled tap water (bottled water is ok if the container has not been previously opened. Do not use sparkling mineral water or soda water).
- Water first. Start with water, then add the formula.
- Measure. Always measure the amount of powder using a measuring scoop and ensure the powder in the scoop is levelled..
- Shake and test. Shake the bottle (with the teat on) until the powder dissolves and test the temperature on your wrist (it should be warm, not hot or cool).
-
List three ways you can ensure mealtimes are enjoyable for children.
- Relaxed and unhurried
- Engage with children in discussion
- Share humour and jokes
- Have small groups of children eating at the table
- Allow children choice and to socialise
- Role model healthy eating
