In this topic, we will explore the process of managing short- and long-term medical needs of children, including illness and injury; identifying the health data collected from families; and understanding the implementation of medical management plans.
By the end of this topic, you will understand:
- Legal requirements around illness and injury management
- Collection and maintenance of health records
- Short term medical needs and long-term medical conditions
- Responding to illness and injury
- Documenting illness and injury
- Management of long-term medical conditions, including asthma, allergies and anaphylaxis.
We will also look at how to identify and respond to signs and symptoms of illness and injury and ensure the correct documentation and process have been completed based on legal requirements and service policies and procedures.
National Quality Standard (NQS) Quality Area 2 – Children's Health and Safety covers several specific areas related to this topic:
- Element 2.1.2 - ‘Health practices and procedures’ requires that ‘effective illness and injury management and hygiene practices are promoted and implemented’.
- Element 2.2.2 - ‘Incident and emergency management’ requires that ‘plans to effectively manage incidents and emergencies are developed in consultation with relevant authorities, practised and implemented’.
The Education and Care Services National Regulations 2011 are highly relevant to this topic, particularly the following regulations:
- Regulation 85 Incident, injury, trauma and illness policies and procedures
- Regulation 86 Notification to parents of incident, injury, trauma and illness
- Regulation 87 Incident, injury, trauma and illness record
- Regulation 88 Infectious diseases
- Regulation 89 First aid kits
- Regulation 90 Medical conditions policy
- Regulation 91 Medical conditions policy to be provided to parents
- Regulation 92 Medication record
- Regulation 93 Administration of medication
- Regulation 94 Exception to authorisation requirement—anaphylaxis or asthma emergency
- Regulation 95 Procedure for administration of medication
- Regulation 96 Self-administration of medication

This section outlines the health information and data that is required by the Education and Care Services National Law Act 2010 (Cth) and the Education and Care Services National Regulations to be collected from families for each child on enrolment and before they commence care into the service, and when this information changes during the child’s care within the service.
Purpose of collecting children’s health and medical records
Maintaining accurate health records is essential to providing quality care and protecting the health and safety of children who attend the service. It provides the service with relevant information about each child’s medical history and current level of health and professional medical advice on how best to care and provide for the health needs of each individual child.
This information helps you:
- Identify preventative health needs such as immunisation or dental care
- Prepare a special care plan for children with chronic health issues or special needs such as asthma
- Determine whether or not to exclude a child from activities for health reasons
Privacy and confidentiality
A service has an obligation to ensure any medical information or health data collected from families is received, implemented and stored with the highest level of privacy and confidentiality.
Health information and records should be shared only with employees and educators that are responsible for providing care to the child.
Outside of sharing information to meet the child’s care and health needs, information should not be shared or spoken about with others. This includes other employees, families, friends, community groups or visitors in or out of the service.
Health information and data, including enrolment records, must be kept in safe storage. This will commonly be in a personal file in a locked filing cabinet, with a key under the supervision of the management team in the office area.
Where appropriate, medical information related to medical action plans, such as for anaphylaxis and allergies, may be displayed in the kitchen, staffroom and the child’s rooms. The display of this information should always be implemented with the consent of the parents/guardians.
Types of health data collected
The National Law and Regulations specify the types of health data that must be collected. The data may be collected in paper format or through online software.
Regulation 162 (excerpts) Health information to be kept in enrolment record (excerpts)
- (a)the name, address and telephone number of the child’s registered medical practitioner or medical service
- (b) if available, the child’s Medicare number
- (c) details of any –
- (i) specific healthcare needs of the child, including any medical condition; and
- (ii) allergies, including whether the child has been diagnosed as at risk of anaphylaxis
- (d) any medical management plan, anaphylaxis medical management plan or risk minimisation plan to be followed with respect to a specific healthcare need, medical condition or allergy referred to in paragraph (c)
- (e) details of any dietary restrictions for the child
- (f) the immunisation status of the child
Health data is initially collected through the enrolment form, and the child is unable to commence care with the service until the required information has been supplied. This is to ensure the service has all the relevant information in order to prepare and provide high-quality care for the child.
Example
View Little.ly Early Learning Centre’s enrolment form for reference.
Use the checklist to read the specific types of health data that should be collected. The Education and Care Services National Regulations (specifically Regulation 162 – Health information to be kept in enrolment record) specify the exact health data that must be collected about a child from the family.
General health information that must be collected includes:
- The child’s name, address and date of birth
- The child’s current general practitioner (GP) and other medical practitioner information
- Any current medical conditions, such as allergies
- Any medical management plans in place for the child
- Immunisations records outlining the child’s status
- Authorisation to administer medical care and medication
- Authorisation to call an ambulance and transport the child to hospital.
Collecting immunisation information
Immunisation information is a key part of a child's health record, and in early childhood services, this information often requires updating. Having accurate, up-to-date records is critical, and directors are required to seek medical documentation and update children's records every six months or as the child moves through the immunisation requirements.
Immunisation schedules in Australia cover the requirements of all families and children. Access the Department of Health and National Centre for Immunisation and Research Australia websites and review the following information relating to the National Immunisation Program Schedules:
From two months to four years of age, children go through up to six immunisation periods. The national immunisation schedule for children is for all nonindigenous people.
| Age | Vaccine |
|---|---|
| Birth | Hepatitis B |
| Two months |
|
| Four months |
|
| Six months |
|
| 12 months |
|
| 18 months |
|
| Four years |
|
Note
Children who are not medically vaccinated (which does not include homeopathic or natural immunisation remedies) must be excluded from care during outbreaks of infectious diseases from which they are not protected (even if they are well).
Keeping records current
While it is a parent’s and family’s responsibility to provide any changes or updates to their child’s health information, early childhood services need to proactively help.
You can do this by:
- Communicating frequently with parents to stay updated on a child’s health, and make every effort to ensure records are maintained with up-to-date information
- Working proactively with other educators to ensure the sharing of a child’s health information
- Ensuring lines of communication are strong between all the critical caregivers in a child’s life.
Check your understanding

Knowing what to look for and how to swiftly respond to illness and injury in children helps to care for the child, and keep them and those around them safe. The content in this section assumes that educators have a current first-aid certificate. Your first-aid manual is an excellent resource for learning appropriate first-aid practices and techniques.
Short and long-term medical conditions
In a service educators will commonly need to identify, respond to and manage children’s medical needs and illnesses. This is a daily practice, and educators need to be confident in their understanding of the child’s short term medical needs and long-term medical conditions. Common signs and symptoms of an illness can be present in both short-term illness and long-term medical conditions.
Short-term medical needs
Short-term medical needs relate to illness that usually lasts between one and seven days. This kind of illness can typically be treated with general home care, such as rest, hydration and medication.
Short-term illness in an early childhood service may include:
- Cold- or flu-like symptoms
- Stomach upsets
- Conjunctivitis
- Headaches.
Long-term medical conditions
Long-term medical conditions refer to medical conditions that have been diagnosed by a medical professional and that last over six months.
Long-term medical conditions in an early childhood service may include:
- Asthma
- Anaphylaxis
- Allergies
- Diabetes
- Epilepsy
- Eczema.
Personal protective equipment

When responding to short-term illness, long-term medical conditions, or injury, you must always protect yourself from harm by using the appropriate personal protective equipment (PPE).
PPE, such as gloves, should be available at all times in the room and also in the outdoor area. Staff are encouraged to put on gloves before administering first aid or caring for an unwell child. A first-aid kit should be available in each room or in a bathroom that is shared by more than one room.
Each room should always have plastic bags available, such as bin bags or large-sized nappy bags, for bloody clothes, and educators should use gloves to remove bloodied clothing and place it in the plastic bag. The bag should then have the child’s name put on it and be given to the family on departure.
Other forms of PPE include:
- Closed-toe shoes
- Clothing covering your shoulders
- Sunglasses
- Sun hat
- Apron
- Hair net.
Identifying and responding to illness
A child may present a variety of signs and symptoms when feeling unwell. These signs and symptoms may be common for either or both short-term illness and long term medical conditions.
Early childhood educators want the best for each child in their care. When a child is unwell, it is vital we ensure they receive care as well as implement practices to ensure we reduce the risk of spreading the illness to other children, staff and families.
Most services have limited ability to care for unwell children and need to be confident to identify, respond to, manage and exclude children where required for the safety of all children and staff.
Health check
Educators should ensure they do a health check of each child when children arrive at the service. This should be done in a subtle manner and without the family and child being aware.
When conducting a health check on a child’s arrival, consider the following:
|
|
|
|---|---|
|
|
|
| Physical appearance | Check the child’s physical appearance. If the child is pale and has red cheeks or yellowish skin, and they seem lethargic, this could indicate the child is unwell. |
| Breathing | Listen to the child’s breathing. If they are coughing, wheezing or using more energy than normal to breathe, this could indicate the child is unwell. |
| Fluids | Check to see if there is any bodily fluid beyond what is normal for the child, such as nose, ear or eye discretion. |
| Skin | Check to see if the skin looks pale or clammy, and look for any sores or rashes that could indicate the child is unwell. |
| Behaviour | Consider whether the child’s behaviour is out of character and whether the child is lethargic or sleepy, scratching repeatedly or unusually clingy with their parent. |
If you do note any health concerns when a child arrives at the service, you should communicate these concerns with the parent. There may be additional reasons or circumstances for the signs and symptoms. For example, a child may look lethargic and pale due to lack of sleep.
Each educator will need to be guided by the legal requirements and service policies to conclude if the child is well enough to be accepted into the service on that day.
Assessing a child’s wellness
Once a child is in your care, you can still use the health check to monitor the health needs of the child. However, educators will also need to ensure they can respond to a child when they determine a child is unwell.
Common illnesses you need to be able to recognise:
- Temperature
- Vomiting
- Diarrhea
- Rash
- Conjunctivitis
- Head lice
- Common cold
- Hand, foot and mouth
- Chickenpox
- COVID-19
The following table details the signs and symptoms of each of these common illnesses, the exclusion periods and the care you should provide:
|
|
|
|
|---|---|---|
| Temperature | It is common for a child to have a slightly elevated temperature from common experiences such as vaccinations or teething, factors that are important for services to be aware of. However, high fevers or fevers from unknown illness should be investigated.
Temperatures between 36.2 and 37.2 degrees Celsius are considered normal. If a child has a temperature of 37.5°C to 38°C, retake their temperature after 20 minutes. If it has increased or remains at 38°C, call the child’s parents to ask for permission to give medication (if no medication form was signed prior). If a child has a temperature of 39°C or higher, they are to be sent home immediately. |
Ensure you read the energy of the child. Some children can have a slightly elevated temperature and still be up and about.
If the child is lethargic, make sure you provide a quiet space for the child to lie, offer fluids and take off excess clothing the child is wearing. You may want to wet a small face washer using cool tap water and lay it across the child’s neck, groin or wrists. |
| Vomiting | Pay attention to the frequency of and other indicators related to vomiting. Children may have one episode of vomiting after active play, for example, but this would not indicate a medical issue.
However, if a child vomits twice in one day, the child should be excluded unless there is an obvious non-contagious reason (such as reflux). |
Ensure you provide the child a quiet space for them to lie, provide them a bucket and ensure you keep up their fluid intake. Do not give the child food, and monitor them until they are collected. |
| Diarrhea | Children who have diarrhea, especially if associated with fever, can become dehydrated quickly.
If the child has two loose stools in a day, the child must be excluded until they have gone 24 hours without a loose stool. |
Ensure you provide the child a quiet space for them to lie, and keep up their fluid intake. Do not give the child food, and monitor them until they are collected.
If blood is found in stool, ensure you refer the child to hospital. |
| Rash | Rashes may include small red dots or larger blotches. Rashes can be flat or raised and can cover a small or large part of the body.
Some rashes may be itchy for children and some may not. Rashes can occur when children are unwell and infectious or can be an aspect of a long-term medical condition such as eczema, which is not contagious. Rashes can also be caused by a child feeling stressed or hot, or crying. Rashes can last 10 minutes or be continuous. It is important to consider the likelihood of the rash indicating a serious medical issue and act accordingly. |
If you are aware that the rash is being caused by the child’s feelings of stress, then comfort and nurture the child. If you are aware that the rash is caused by a long-term medical condition, then refer to the child’s medical action plan.
If you are unaware of why the rash has occurred, you need to treat it as infectious. Call the child’s parents to collect the child. Isolate the child from other children and check for other signs and symptoms. Monitor the child until parents arrive. |
| Conjunctivitis | Children will often present with red or swollen eyes, which may contain mucus. This mucus will normally present most frequently after sleep, and it might glue the eyes shut.
An educator is required to wipe away the mucus and wait 20 minutes. If the mucus returns, they need to call the parent and exclude the child from the service. The child can return only when the mucus has gone (or when they are on medication from a doctor). |
Use a cotton ball with lukewarm water and wipe the eye gently from the inside (closest to the nose) to the outside (farthest from the nose), using one wipe per cotton ball.
Clean the eye in this way every time mucus presents, and monitor the child until they are collected by their parent or an authorised person. Always wear gloves when wiping eyes to reduce the risk of conjunctivitis spreading. |
| Head lice | Head lice is very common and can be identified by noticing a child scratching their head repeatedly. An educator may see a single louse or a number of head lice and eggs on the child’s head.
Once a child has been identified with head lice, you must call the parents and exclude the child until they have been treated. |
It is not appropriate to exclude the child from other children in the service. However, educators can encourage children to keep distance from each other and ensure the child with head lice feels comfortable until they are collected by their parent or an authorised person. |
| Common cold | Common colds tend to come on gradually. They usually include a temperature, stuffy nose, sore throat and sneezing. The child will often look pale, be lethargic, have difficulty sleeping and lose their appetite. They might also be uncommonly unsettled and want to go home.
When a child has a temperature over 39 degrees or shows signs and symptoms of being infectious or too unwell to be at the service, and the service cannot provide the required care, then the child would be excluded until they are well again. |
Ensure you provide the child with a quiet space for them to lie or play, and encourage the child to sleep, eat and hydrate where possible.
Promote restful play and monitor the child’s symptoms. Take the child’s temperature every 30 minutes. |
| Hand, foot and mouth | Signs and symptoms include fever, sore throat and painful mouth sores that usually begin as flat, red spots and then develop as blisters—these may appear on the palms of the hands; soles of the feet; and sometimes the knees, elbows, buttocks or genital area.
The child will need to be excluded immediately for at least four to five days or until the blisters have dried. |
Ensure the child has a quiet place to rest.
Monitor their temperature and keep up their intake of fluids and food. Encourage rest and monitor symptoms until the child is collected by their parent or an authorised person. |
| Chickenpox | Chickenpox begins with a fever, aches and pains. Within one or two days, the child will get a rash, which is usually itchy and can make the child uncomfortable. Most children lose their appetite and have a headache during the first few days.
Children will need to be immediately excluded and can return to care only after the blisters have dried—usually not before four to five days. |
Ensure the child has a quiet place to rest. Monitor their temperature and keep up their intake of fluids and food. Encourage rest and monitor symptoms until the child is collected by their parent or an authorised person. |
| COVID-19 | The most common signs and symptoms of COVID-19 include fever, chills, worsening cough or barking cough, shortness of breath, sore throat, extreme tiredness, sluggishness or lack of appetite. Call Triple Zero (000) if a child presents the following signs: severe difficulty breathing, confusion or loss of consciousness.
The child will need to be immediately excluded when showing signs and symptoms of COVID-19. Children will need to be tested and receive a negative test result in order to return to the service. Children are also required to be well and free of symptoms or obtain a doctor’s medical confirmation before returning to the service. |
Ensure the child has a quiet place to rest. Monitor their temperature and keep up their intake of fluids and food. Encourage rest and monitor symptoms until the child is collected by their parent or an authorised person. |
Other common indicators of illness:
Responding to signs and symptoms of illness
If you suspect a child may be ill, follow these steps:
Speak to your colleagues to find out what the child has eaten and drunk and about the child’s nappy changing or toileting that day. Before giving any medication, remember to check with other educators that medication has not been given beforehand or prior to the child arriving at the service, and review the child’s medical history.
Separating a child means providing a quiet space for the child to lie down and rest and encouraging the other children to let the child rest, but the child will still be in the same room as the other children.
Be sure to stay with the child to comfort and monitor them while a decision is being made about calling the parents.
This information should be recorded on your service’s illness and accident forms.
While caring for the child, remember the following guidelines to minimise infection spread:
- Remind the child to cough or sneeze into their elbow. Wash their hands if they have coughed or sneezed into their hands.
- If you wipe their nose, dispose of the tissue and wash your hands.
- Wash your hands and have the child wash theirs before touching other children.
Taking a temperature

High temperatures can be associated with many signs, symptoms and illnesses. Many children will have mild, low-grade temperatures as a result of vaccinations or teething. While a temperature alone is not a clear indicator of a child being sick, monitoring the temperature of a child who appears unwell or hot is important.
Steps to take a temperature:
- Wash your hands thoroughly.
- Use a protective cover for the thermometer if available.
- Clean and reset the thermometer.
- If taking a temperature orally, make sure that the child has not had anything hot or cold to eat or drink in the previous 10 minutes.
- Place the thermometer under the arm, tongue or in the ear, depending on the type of thermometer.
- Leave in place until it beeps, for up to one minute.
- Record the temperature, time and method.
note
Normal body temperature: 36.2–37.2°C
Low-grade fever: Under 38°C
High-grade fever: 39°C and above
Care and hygiene
When caring for an unwell child, always remember to wash your hands and have the child wash theirs thoroughly. Ensure any areas the unwell child has been using, or that may be affected by body fluids, discharge or germs, are cleaned and disinfected to keep yourself and the children safe.
You should wash your and a child’s hands for 20 seconds to ensure good hygiene. You can time 20 seconds by singing the song ‘Happy Birthday’!
WATCH
Watch the following 2-minute video on singing ‘Happy Birthday’ with children when washing their hands:
Revisit Staying Healthy: Preventing Infectious Diseases in Early Childhood Education and Care Services, and read pages 10–27, which provide more information on minimising the spread of infection.
Identifying and responding to injury
Children, particularly toddlers and children just learning to be mobile, are prone to falling, bumping and bruising. It is also hard for them to describe exactly what happened when an injury happens. This means it is important to be constantly supervising children and providing a safe space for them. However, even with the best supervision, injury is possible—it takes only a few seconds for a child to trip and bump their head or scrape their hands.
Key points
Maintain your first-aid knowledge—all educators are required to have a current first-aid certificate. Review your notes regularly and keep your skills sharp. Don’t forget that First Aid certificates are valid for three (3) years, while the cardiopulmonary resuscitation (CPR) training needs to be repeated every year to keep your knowledge and skills up-to-date.
When responding to injuries, you may be presented with the following:
- Blood
- Scratches and cuts
- Burns
- Breaks and fractures
- Grazes
- Sprains
- Swelling
- Lumps and bruises
It is advised that educators refer to their first-aid training when deciding how best to respond and manage a child’s injury.
The foundations of First Aid
- Protect yourself. First, ensure you and the other children are not in danger. You cannot help a child if you are not safe. This means removing yourself and others from danger, and using PPE to protect yourself against bodily fluids.
- Assess the child’s needs. Assess the child’s needs and injuries, and action first aid.
- Call for help. If required, call Triple Zero (000), and also ask for assistance from other staff—this could include asking them to remove other children from the area.
- Prioritise injuries. If more than one child is injured, prioritise the most wounded and urgent first.
- Document. Document the injury, incident, accident or trauma on the service’s incident report form.
Incidents involving blood
Children can be injured in a manner that causes bleeding. Common bleeding injuries we see in the early childhood setting are nosebleeds, bites from other children, falls, scrapes and cuts. It is important to treat the child and be diligent in cleaning up the blood and protecting other children from coming into contact with the blood.
In the event of a bleeding injury, follow these guidelines:
- Look after the child. Comfort the child and move them to safety. Avoid contact with the blood—put on gloves if possible. Apply pressure and elevate the wound. Reach out for assistance if needed.
- Dress the wound. Dress the wound with a suitable bandage. Call Triple Zero (000) if the situation is urgent. Remember to remove your gloves and wash your hands after dressing the wound.
- Clean the blood spill. The most effective way to clean small and large blood spills is with warm water and detergent. Large spills will require an absorbing agent or scrapper and may also require disinfection with diluted bleach.
Cleaning up faeces, vomit, urine
- Wear gloves.
- Cover the spill with paper towel and let the spill soak in. Put paper towel in plastic bag.
- Clean the surface with warm water and detergent—let it dry.
- Wash hands thoroughly.
Example
View this example illness and accident form approved by ACECQA.
Documentation
In the case of illness, and injury or incident, documentation of the event is critical. When an injury occurs, the staff member who saw the incident or noticed the injury would be the one to complete an incident, injury, trauma and illness record. A witness will also need to sign the form to confirm the details of the form. A witness, which is anyone else who saw the injury or incident, or was in the room at the time (typically another educator), should sign the form. All incident, injury, trauma and illness records must be signed by the director and the affected child’s parent.
When an illness is identified, the person who noted the illness needs to complete the form in relation to the signs and symptoms, and the continuous care and monitoring that has taken place. This form will need to be completed and then signed by a witness.
Check your understanding
Read the following case study that will have to be documented in an Illness Report:
Child's name: Ava Jenson
Date of Birth (DOB): 7/10/2017
Parent: Sara Jenson
Incident's date: 20/2/2020, 10.20 am
The toddlers were playing outside. Ava was walking along the balance beam unaided outside. The balance beam is 30 cm above the ground and has a frame on each end.
Ava walked to the end of the balance beam and attempted to climb over the frame at the end. Her left foot slipped, and she fell, knocking her chin on the frame. This left a shallow, bleeding cut that was 1 cm long on the bottom of her chin.
You comforted Ava immediately. You put gloves on and applied a pad directly to her chin with pressure for about five minutes. Once the bleeding stopped, you wiped the area gently with saline and applied a patch.
You monitored Ava, and 1 hour 20 minutes later, you called her mother, Sara Jenson, who collected Ava and took her to their doctor to see if she needed stitches.
Additional Details
After speaking with Hayley Schramm (the director) and Yindi Harris, an educator who witnessed Ava's injury, you created a plan to retrain staff in high-risk activities that require outdoor supervision. Specifically, educators should stay within 30 cm of a child on the balance beam and hold a child's hand whenever they step over the frame.
A few days later, you followed up with Sara and heard that not only did Ava not require stitches, but also there was no bruising or swelling after. You assured Sara the staff training had taken place.
Click here to access (and download if you wish) the completed pdf form.
Teaching children about sun safety
It is vital that we use approved practices to protect children from overexposure to the sun. It is also important that we educate children on the how best they can protect themselves and develop agency in this area.
This can be done by:
- Familiarising the children with the UV widget and asking them to check it before going outside
- Setting up a sunscreen-and-hats station with a mirror so children can learn to apply their own sunscreen and protective gear
- Reading stories and singing songs that encourage protection learning
- Collaborating with the children about their sun protection
- Embedding educator-led play to teach the children the cause and effects of sun damage and how to protect themselves
- Encouraging the children to use sunscreen in play, such as putting it on dolls
- Having posters and visuals around the room and door to the outside as reminders.
Note
Services often provide their own sunscreen. If a child has a sensitivity to the provided sunscreen, the child’s family will provide their own.
Read
Visit the following links to learn about clothing to protect from the sun:
- 'Sun Protective Clothing’ from SunSmart
- ‘Sun Protective Hats’ from SunSmart
You can monitor the UV rays throughout the day by using the SunSmart widget, which provides real-time updates about the UV level and protection required throughout the day—you can download the widget at this link.
Medication
Accepting medication
Medications may be purchased off the shelf from pharmacies or be prescribed by a doctor.
Medications purchased off the shelf need to be brought to the service in their original packaging, with full instructions and details, and the child’s full name on the medication.
Prescription medication has to come in its original packaging and must have a label printed by the pharmacy with the doctor’s name, child’s name, and instructions.
Educators are responsible for reading the instructions and ensuring they administer medication only in relevance to the instructions. Medication can only be administered if it is authorised by a registered medical practitioner and/or a parent. Whenever is possible, another educator should check the dosage of the medication to be administered and the identify of the child to whom the medication is to be administered.
When a family member or parent brings in medication, they must have a discussion with the educator about their child’s symptoms and the reason for the medication. The symptoms must be in line with the information on the package.
The parent will need to update their section of the medication record, and an educator should place the medication in a fridge or locked in a high cupboard, out of reach of children.
Administering medication
When children require administration of medication in an early childhood setting, educators need to ensure compliance with the Education and Care Services National Regulations. Medication is addressed in regulation:
- Regulation 92 – Medication record
- Regulation 93 – Administration of medication
- Regulation 95 – Procedure for administration of medication
Medication that is commonly administered includes:
- Pain relief
- Cough medicine
- Antibiotics
- Creams and ointments
- Ear and eye drops.
Example
Here’s an example of an administration of medication policy by Little.ly Early Learning Centre.
Example
Have a look at the following sample medication record that has been approved by the ACECQA for services to use when administering medication.
Check your understanding

Many children have long-term medical conditions that are managed but can still require medical treatment and monitoring, and in some cases, emergency medical attention.
It is important to be up to date on the medical history and conditions of the children in your care. Some conditions may be diagnosed at the time of enrolment, and others may develop or be diagnosed while the child is attending your service.
Three (3) common ongoing conditions are anaphylaxis (a life-threatening allergic reaction), asthma and allergies.
Anaphylaxis
Anaphylaxis is a life-threatening reaction that causes the swelling of a person’s throat, restricting the ability to breathe.
Triggers
Common triggers for anaphylaxis are:
- Food
- Insect bites
- Medicines.
Anaphylaxis: What to look for
- Difficult or noisy breathing
- Swelling of tongue
- Swelling or tightness in throat
- Wheezing or persistent cough
- Difficulty talking or hoarse voice
- Persistent dizziness
- Collapsing
- Pale skin and floppiness (young children)
WATCH
Watch the following 1-minute video to see the use of an EpiPen for an anaphylactic reaction:
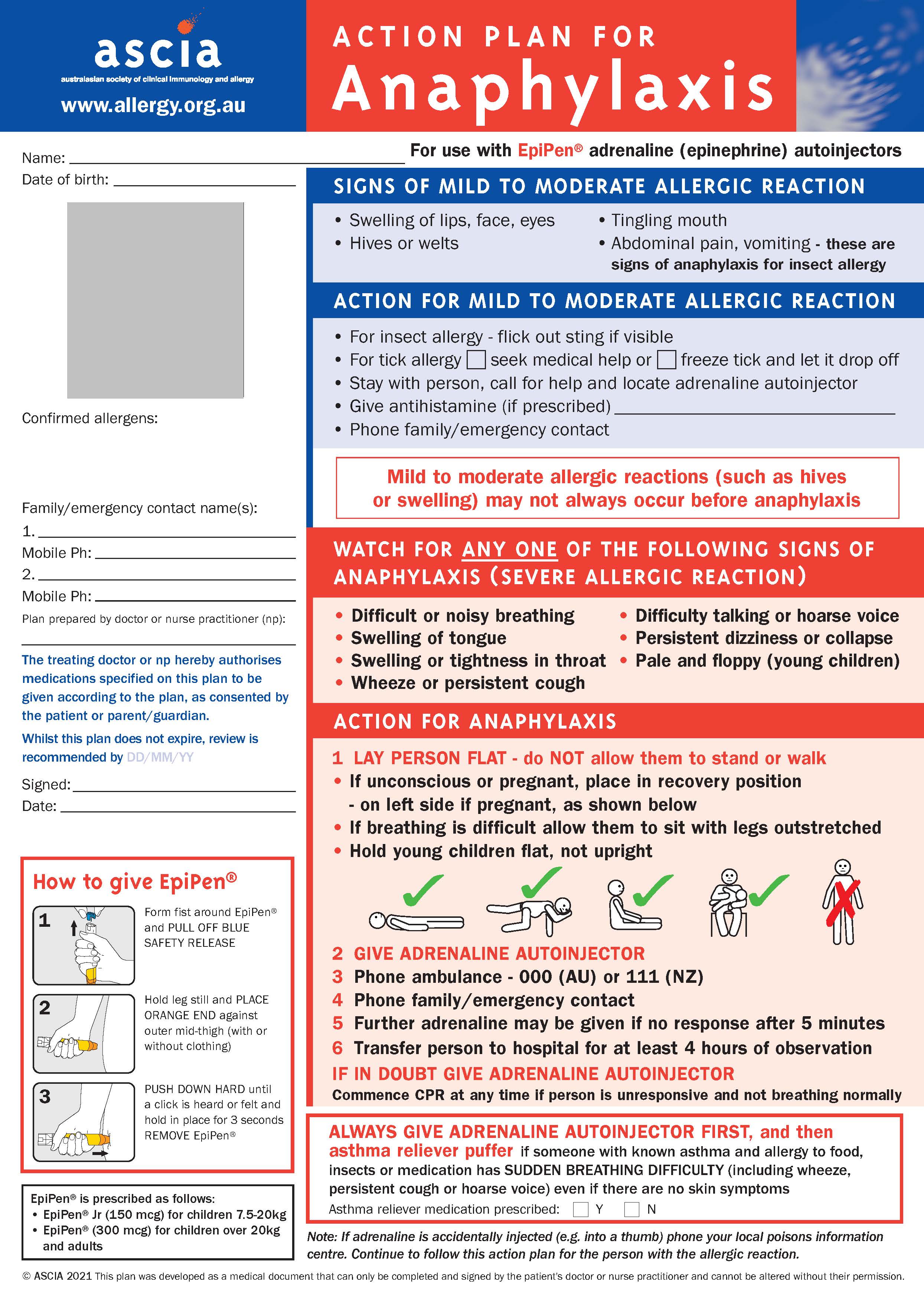
Treatment
When a child is having an anaphylactic reaction, you need to follow the treatment instructions on the child’s anaphylaxis management action plan.
The steps required will likely be as follows:
- Remain calm. Remain calm and call for assistance from other educators.
- Call for assistance. Lay the child down while ensuring someone is calling Triple Zero (000) and accessing the child’s management plan and EpiPen Jr.®
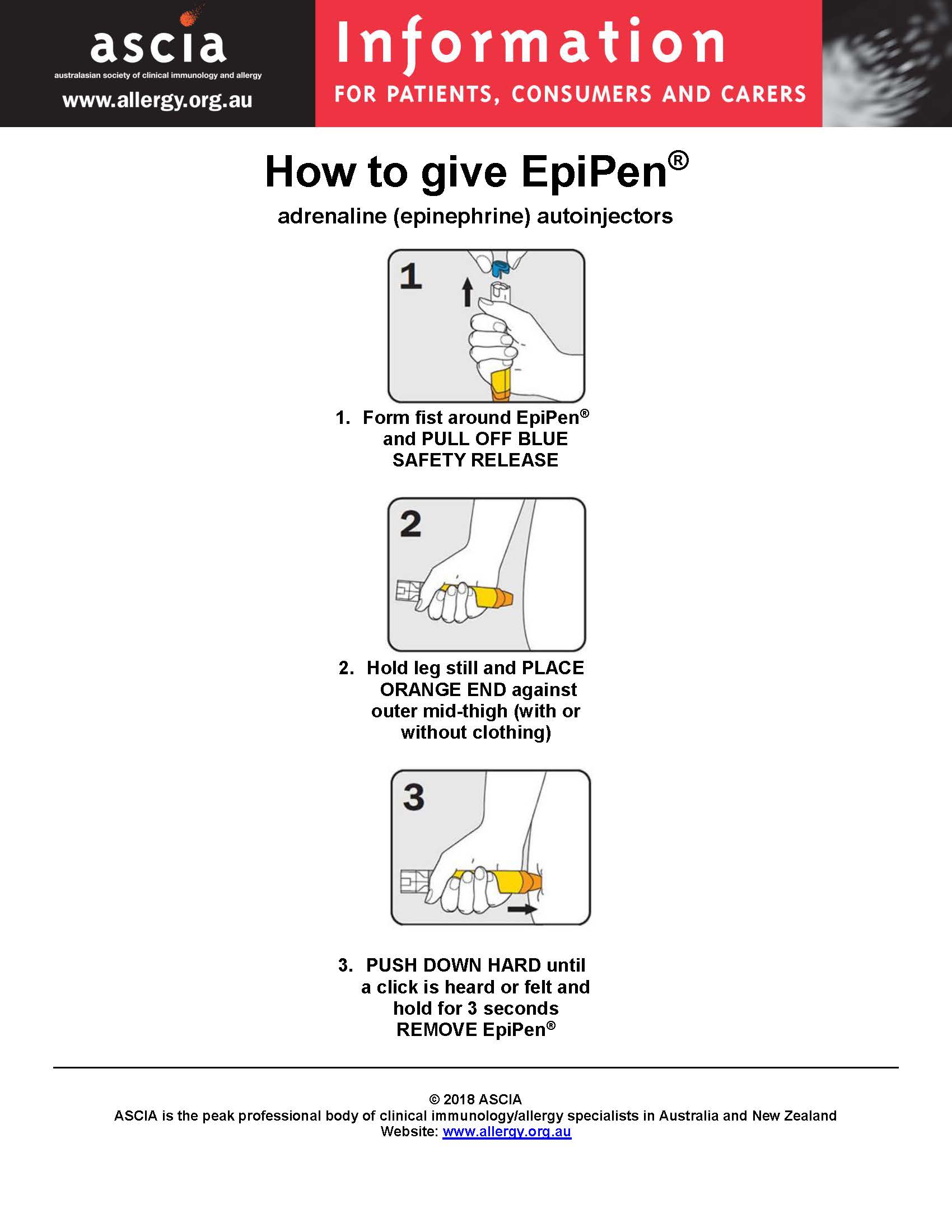
- Prepare the EpiPen Jr.® Form a fist around the EpiPen and remove the blue safety release.
- Prepare the child. Hold the child’s leg still and place the orange end against their mid-thigh.
- Administer the EpiPen Jr.® Push down using the EpiPen and hold it in the thigh for three to four seconds.
- Monitor responses. Monitor the child for a response—continue following advice of the emergency services.
- Notify the parents or family. Contact the child’s parents or family to notify them of the anaphylactic reaction.
Administering an EpiPen®
- Form fist around EpiPen® and pull off blue safety release
- Hold leg still and place orange end against outer mid-thigh (with or without clothing)
Push down hard until a click is heard or felt and hold in place for 3 seconds. Remove EpiPen®.
The following graphic demonstrates how to properly administer an EpiPen®:
To learn more about anaphylaxis, including triggers, signs and symptoms, risk factors and treatment, visit Better Health Channel.
Asthma
Asthma is a medical condition that affects the respiratory system of a person, narrowing the airways and filling them with mucus. This results in an inability to breathe properly and clearly, and needs interception of medication.
Children may take two forms of medication:
- Prevention
- Reliever.
Triggers
Common triggers of asthma are:
- Colds and flu
- Physical activity
- Weather
- Irritants in the air.
Signs and symptoms
Asthma: What to look for:
- Gasping, wheezing, coughing, rapid and shallow breathing
- Inability to say more than a few words without pausing to breathe
- Tightness in the chest
Treatment
When a child is having an asthma attack, you need to follow the treatment instructions on the child’s asthma management action plan.
The steps that you will be required to carry out are as follows:
- Check the environment. Check to see if there is something in the environment that is triggering the attack, and move the child away from the trigger. Access the child’s asthma management action plan and medication.
- Implement the reliever using the 4x4x4 method. Sit the child down on the floor or a chair. Place the medication into the spacer, and place the spacer in the child’s mouth. Dispense one puff of the medication and ask the child to take four slow breaths— repeat this process three more times. Wait and monitor the child for four minutes.
- Monitor the child and repeat step 2 if necessary. If the child has not improved after the four minutes, implement the 4x4x4 method with the reliever medication again. If after two attempts you see no improvement, call Triple Zero (000).
WATCH
Watch the following 6-minute video to learn more about asthma, its symptoms, triggers and treatment:
To learn more about asthma, including triggers, signs and symptoms, and causes, visit the National Asthma Council Australia’s website.
Allergies
Allergic conditions are a common health issue affecting children. Allergies can be triggered by a host of indoor and outdoor allergens, and many children have more than one type of allergy. Known allergies should be discussed at enrolment, and educators must be up to date on knowing each child's record and be aware that allergies can change as children are exposed to new things.
Allergies refer to the body’s immune system’s reaction to the presentation of particular food, pollen or substance. Allergens refer to the particular food, pollen or substance that causes the reaction of the immune system.
Intolerance refers to a substance that the body can consume in a particular amount. Once that amount is exceeded, the body will have a reaction.
Note
Severe allergic reactions require immediate medical help.
Signs and symptoms
Allergies: What to look for
- Coughing
- Sneezing
- Itchy eyes
- Runny nose
- Scratchy throat
- Rashes or hives
- Breathing trouble
Responding to an allergic reaction
Always refer to the child’s allergy management plan to ensure you are actioning the correct treatment, which can include:
- Using antihistamines
- Resting and monitoring the child
- Using a cold pack or cool face washer to relieve swelling, redness or itchiness.
Common allergies in children
| Indoor/outdoor allergies | Triggers of outdoor allergies can include grass and tree pollens, insect and bees, and general pets and animals.
Triggers of indoor allergies can include dust and dust mites, certain fabrics, mould, and perfumes or cleaning products. Bodily response to these allergens usually includes sneezing, running nose, sore red or itchy eyes. The response can also include a sore throat and onset of asthma, and the allergens may cause redness or itching around the impacted area. |
| Skin allergies | While children can have reactions of the skin for most allergies, there is also a range of skin allergies that are often caused by the child having a low immune system. Common reactions to skin allergies include dermatitis and eczema.
Exposure to the following can antagonise skin allergies:
Responses to these triggers can include outbreaks of dry skin, red rashes, sores, and in some situations, infection in broken or damaged skin. |
| Food allergies | Food allergies are based on a child consuming a food the body has a reaction to.
Common food allergies include:
When children come into contact with these triggers, they may show signs of:
|
| Drug allergies | Some children may have an allergy to medication. A common medication children may be allergic to is penicillin.
Penicillin is a common antibiotic used to support fighting an infection. Allergic reactions to drugs can include:
|
| Insect allergies |
Some children can have an allergic reaction to insect bites. Common insect bites that cause an allergic reaction include:
Children’s allergic reactions can range from minor to severe and include the following symptoms:
|
WATCH
Watch the following 5-minute video to learn more about how to deal with food allergies in an education and care setting:
To learn more about allergies, including what happens during an allergic reaction, what causes a reaction, and signs and symptoms, visit ASCIA’s website.
Management plans
Medical management plans are documents that have been prepared and signed by a doctor that describe symptoms, causes, clear instructions on action and treatment for the child’s specific medical condition, and include the child’s name and a photograph of the child. An example of this is the Australasian Society of Clinical Immunology and Allergy (ASCIA) Action Plan.
Being trained and prepared to handle anaphylaxis, allergies and asthma care is highly important given the often sudden and severe nature of attacks. It is important you ensure your training is up to date and that you know and follow the related policies of your service.
For anaphylaxis, asthma and allergies, the family is required to have a medical action plan approved by a doctor and submitted to the service. These action plans will be displayed in the room the child is currently in, possibly also in the staff room and the kitchen, and need to be updated every 12 months and reviewed by the doctor.
These action management plans will indicate the specific signs and symptoms of the child, and actions to take to provide appropriate medical care for the child.
Example
Visit the following links for examples of medical action plans: ‘Asthma Care Plan for Education and Care Services’ from Asthma Australia:
- ASCIA Action Plans here, and here
- 'First Aid Plans for Anaphylaxis’ from the Australasian Society of Clinical Immunology and Allergy (ASCIA)
For more information on asthma care plans and first aid, visit the Asthma Australia website.
Example
View Little.ly Early Learning Centre’s asthma and anaphylaxis management policy for reference.
Additional common long-term medical conditions
Being trained and prepared to handle anaphylaxis, allergies and asthma care is highly important given the often sudden and severe nature of attacks. It is important you ensure your training is up to date and that you know and follow the related policies of your service.
For anaphylaxis, asthma and allergies, the family is required to have a medical action plan approved by a doctor and submitted to the service. These action plans will be displayed in the room the child is currently in, possibly also in the staff room and the kitchen, and need to be updated every 12 months and reviewed by the doctor.
These action management plans will indicate the specific signs and symptoms of the child, and actions to take to provide appropriate medical care for the child.
| Condition | Description & Resource | Signs & Symptoms | Treatment |
|---|---|---|---|
| Epilepsy | Epilepsy is a disorder that affects the brain.
(Source: ‘What Is Epilepsy?’ from the Epilepsy Foundation) |
|
If you are aware of the child’s diagnosis, then action the child’s epilepsy management plan.
Note: It is important to allow the seizure to occur. You must make the area safe and time the seizure. |
| Diabetes |
Diabetes is a chronic condition that involves the child’s level of glucose in the body. There are two types of diabetes: type 1 and type 2. (Source: ‘Diabetes’ from The Royal Children’s Hospital Melbourne.) |
Low blood sugar levels:
High blood sugar levels:
|
Be aware of the signs and symptoms of the child’s diabetes. Ensure you monitor the child regularly and act fast when identifying signs of high or low blood sugar. Follow the health advice of the child’s doctor, who will provide an action plan for the child. |
| Eczema |
Eczema is a condition of the skin, and there are many types and forms. (Source: ‘Eczema (Atopic Dermatitis)’ from the Better Health Channel) |
|
Each child should have a doctor-approved plan to treat the child’s skin. This will usually include a combination of creams and moisturises that may be applied multiple times a day. |
Check your understanding
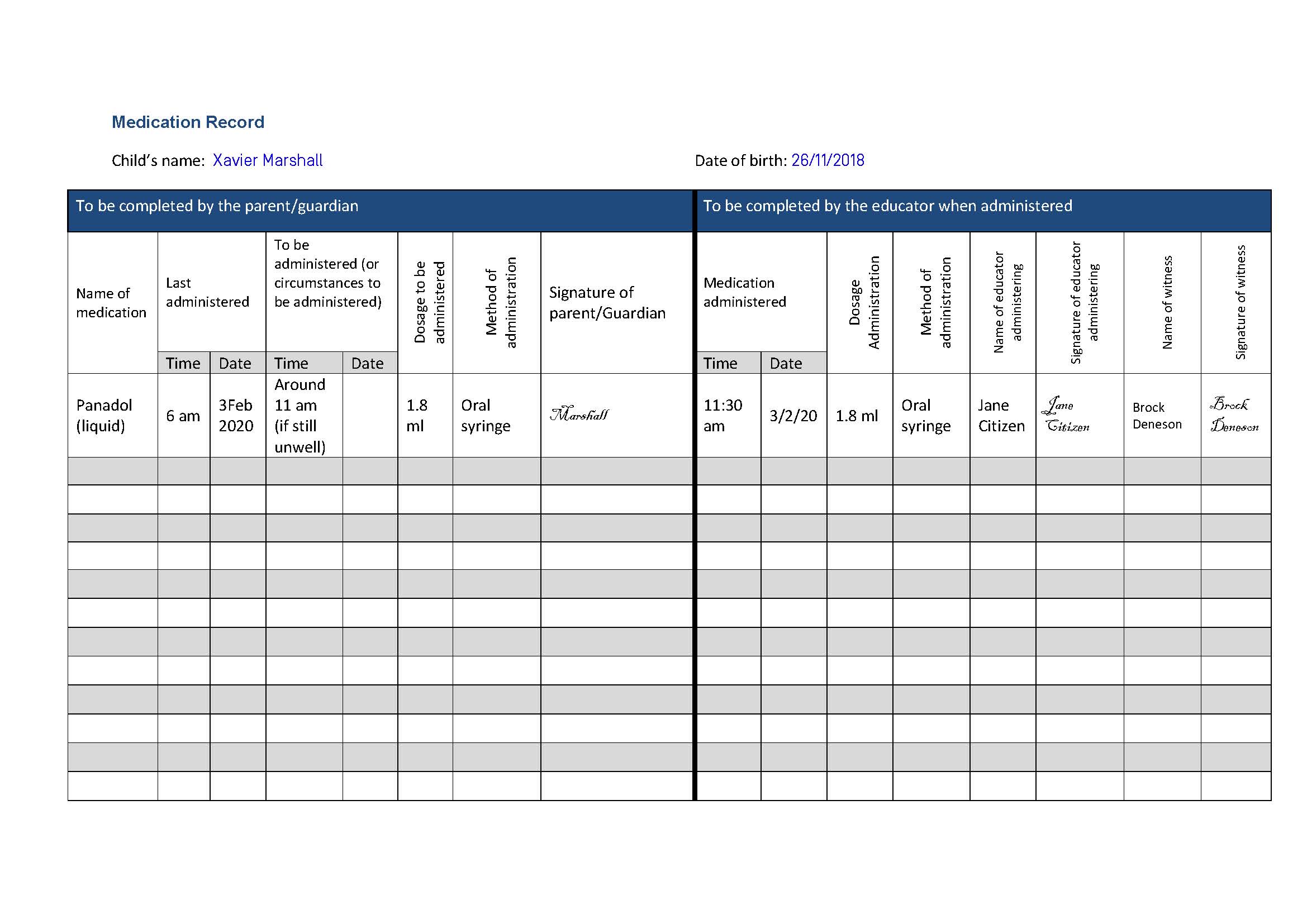
Read the following case study and complete the task that follows:You are an early childhood educator at Little.ly Early Learning Centre.
Today, 3 February 2020, one of the children in your care, Xavier Marshall (born 26/11/2018), was immunised a few days ago. He now has a mild temperature and is upset. His mother has provided Panadol.
She gave him 1.8 ml (by oral syringe) at 6 a.m.
By 11:30 a.m., you notice the child is unsettled again.
You administer another dose of Panadol, and your colleague, Brock Deneson, helps to verify the dosage and administration.
Use the following website to consider whether the medication given to the child was appropriate according to the instructions:
- ‘Here’s How to Choose the Right Dose for Your Child’ from Panadol.
Following the service's procedure, you must complete the medication form for Xavier.
Use the following questions to check your knowledge. You can check the correct answer by clicking on the 'Answer' button:
-
What may be included in a child health record?
- Immunisations
- Medicare and health insurance details
- Medical history
- Current medical needs such as illness or injures
- Asthma, allergies and anaphylaxis information
- Any medications child needs to take
-
How does a service collect and store information regarding children’s immunisations?
The family will provide a copy of the child’s health record. This could be in the form of a health book. These days it’s usually emailed through the mygov app. A copy is printed and placed in the child file under lock and key in the office and is rechecked every 6–12 months. -
What is a healthy temperature range for children?
36.2oC-37.5oC -
What illnesses require a child or staff member to be excluded from the service?
For example:- measles
- chickenpox
- conjunctivitis
- gastro
- flu
- hand, foot and mouth disease
- rubella
-
List six pieces of information that need to be included in an incident, injury, trauma and illness record.
The Incident, injury, trauma and illness record must include:- (a) details of any incident in relation to a child or injury received by a child or trauma to which a child has been subjected while being educated and cared for by the education and care service or the family day care educator, including:
- (i) the name and age of the child; and
- (ii) the circumstances leading to the incident, injury or trauma; and
- (iii) the time and date the incident occurred, the injury was received or the child was subjected to the trauma;
- (b) details of any illness which becomes apparent while the child is being educated and cared for by the education and care service or the family day care educator including:
- (i) the name and age of the child; and
- (ii) the relevant circumstances surrounding the child becoming ill and any apparent symptoms; and
- (iii) the time and date of the apparent onset of the illness;
- (c) details of the action taken by the education and care service or family day care educator in relation to any incident, injury, trauma or illness which a child has suffered while being educated and cared for by the education and care service or family day care educator, including:
- (iv) any medication administered or first aid provided; and
- (v) any medical personnel contacted;
- (d) details of any person who witnessed the incident, injury or trauma;
- (e) the name of any person:
- (i) whom the education and care service notified or attempted to notify, of any incident, injury, trauma or illness which a child has suffered while being educated and cared for by the education and care service or family day care educator; and
- (ii) the time and date of the notifications or attempted notifications;
- (f) the name and signature of the person making an entry in the record, and the time and date that the entry was made.
- (a) details of any incident in relation to a child or injury received by a child or trauma to which a child has been subjected while being educated and cared for by the education and care service or the family day care educator, including:
