Reading A: ‘Environments of concern’: reframing challenging behaviour within a human rights approach
Reading B: Do health care professionals worry about delirium? Relatives’ experience of delirium in the intensive care unit: A qualitative interview study.
Reading C: The fundamentals of person-centred care for individuals with dementia
Reading D: Addressing behaviours of concern: The interplay of health, communication, limitations, and psycho-social factors
Important note to students: The Readings contained in this Book of Readings are a collection of extracts from various books, articles and other publications. The Readings have been replicated exactly from their original source, meaning that any errors in the original document will be transferred into this Book of Readings. In addition, if a Reading originates from an American source, it will maintain its American spelling and terminology. AIPC is committed to providing you with high quality study materials and trusts that you will find these Readings beneficial and enjoyable.

Jorgensen, M., Nankervis, K., Chan, J. (2023). ‘Environments of concern’: reframing challenging behaviour within a human rights approach. International Journal of Developmental Disabilities, 69(1), 95-100.
History of Challenging Behaviour
Historically, personal expressions of people with intellectual and other cognitive disability such as aggression, self-harm, and repetitive behaviours were labelled as ‘abnormal’, ‘dysfunctional’, ‘aberrant’, ‘problem’ or ‘maladaptive’ (NICE, 2015). However, in the absence of acute medical causes, these behaviours are often valid responses to being unable to communicate unmet needs (NICE, 2015) or being in difficult environments and situations (Ramcharan et al., 2009) Like any person who is unable to exercise choice and control, a person with disability might react negatively to an oppressive home environment by yelling or leaving home. As one person with intellectual disability living in a residential facility put it:
I wanted a glass of milk and they said ‘no’ so I kicked off. They said there wasn’t enough, but there was. (Jones and Kroese, 2009)
Emerson and Bromley’s term ‘challenging behaviour’ was coined in 1995 and, along with the close derivative ‘behaviour that challenges’, is still widely used today. Unlike earlier terms that implied the ‘problem’ was entirely located within the person, ‘challenging behaviour’ was originally intended to remind those working with people with disability that such behaviour was a challenge to service provision. Under Emerson and Bromley’s (1995) definition, ‘challenging behaviour’ is seen as:
Culturally abnormal behaviour of such an intensity, frequency or duration that the physical safety of the person or others is likely to be placed in serious jeopardy, or behaviour which is likely to seriously limit use of, or result in the person being denied access to, ordinary community facilities. (Emerson and Bromley (1995)
Emerson and Einfeld (2011)extend that definition to characterise ‘challenging behaviour’ not just in terms of those that risk physical harm or limiting community access, but also those that impact more broadly on wellbeing and life quality. They also argue that ‘challenging behaviour’ must be seen as a social construction – that is, that social processes are involved in defining ‘acceptable’ behaviour and that this has consequences for the person with disability and others in their lives.
Though emphasising the socio-cultural context for behaviour, both Emerson’s 1995 and 2011 definitions of ‘challenging behaviour’ centre the experience of the service provider or society, still framing the ‘behaviour’ of the person with disability as the problem that is ‘challenging’ others. In these definitions, the behaviour is defined by society, but not explicitly caused by it – the focus is not on identifying problems with the environment that a person is in. Further, it takes a view that such behaviour is ‘abnormal’, even though the behaviour may be a ‘normal human response’ to a challenging situation (Swaffer, 2018), or very functional in being a way to quickly and easily communicate distress.
Ramcharan et al. (2009) suggest that many ‘challenging behaviours’ may be better framed as ‘adaptive behaviours to maladaptive environments’. In this context, behaviour can be seen as a form of ‘resistance’ or ‘legitimate protest’. However, like another proposed alternative that focuses on external causes – ‘responsive behaviour’ (Markwell, 2016) – this phrase likely requires significant explanation to be fully understood by most people (Cunningham et al., 2019).
Others have advocated for the phrase ‘behaviours of concern’, as a way to move away from highlighting the adversarial ‘challenge’ set to providers (Chan et al., 2012). While ‘behaviours of concern’ has been widely adopted and used within Australia, ‘challenging behaviour’ and ‘behaviour that challenges’ (Gore et al., 2022)) still predominates in the field of PBS internationally. The drift toward using these terms as diagnostic labels (Emerson and Einfeld, 2011) (e.g. ‘his challenging behaviours’) demonstrates that unless there is real change in how behaviour is viewed, any changes in terminology will just become another simile for an entrenched approach that sees the person as the problem.
Language is never ‘just semantics’; words have power. We shape our language, and those words in turn shape how we think and the things that we do. The behaviour of people with disability is pathologised through language in a way that it is not for people without disability, and this has consequences.
For people with disability, normal acts of everyday life are frequently labelled and medicalised – going to the toilet becomes ‘toileting’; going out becomes ‘accessing the community’ (and also implies that a person with disability is not part of the community). These acts of labelling and medicalisation can lead to an ‘othering’ of people with disability (Hayes and Hannold, 2007), undermining their human rights and creating further vulnerability and marginalisation. Kitwood, for example, used the phrase ‘malignant social psychology’ to describe the ways in which those around a person with dementia can undermine the person’s wellbeing through depersonalising language and actions, reducing life-affirming interactions and precipitating further cognitive decline (Kitwood, 1997).
Critically, the pathologisation and labelling of a person with disability as having ‘challenging behaviours’ can provide a medical rationale to medicate and restrain. Despite increasing regulation and years of research highlighting the negative impact of psychotropic medication and other restraints, their use in managing the behaviour of people with disability remains highly prevalent (Branford et al., 2019). A reframing of ‘challenging behaviour’ that moves past a biomedical lens is needed – not just for terminology’s sake, but as a mechanism to shift behaviour support practice to better identify and address ‘environments of concern’.
The evidence for ‘environments of concern’
The aim of PBS is to ensure high quality support that combines the goals of enhancing life quality and reducing ‘behaviours that challenge’, for the benefit of people with disability and other key people in their lives (Gore et al., 2022)). This should include bespoke support ‘environments’ and constructional approaches that support people to learn and use important skills to mitigate the risk of ‘behaviours that challenge’ (Gore et al., 2022).
Increasing evidence suggests that focusing on ‘environments’ is the key to meeting behaviour support needs and improving quality of life for people with disability. Central to this evidence is the views of people with disability themselves, as well as evidence on the effectiveness of behaviour change interventions both for people with disability and in the wider population.
Van den Bogaard et al (2019) undertook a systematic review of studies that asked people with intellectual disability for their views on the causes of their own or others’ ’challenging behaviours’. They identified three main types of factors across 10 studies: environmental, interpersonal, and intrapersonal factors. Environmental factors leading to ‘challenging behaviour’ related not just to the physical environment, but also to the wider community and its structure, including feeling excluded or isolated. Intrapersonal causes (i.e. factors coming from within), such as emotions, were often seen by people with disability as being triggered by interpersonal interactions or environmental factors.
In the field of PBS, interventions that focus just on the ‘environments’ around a person with disability have been shown to be effective in improving outcomes for caregivers, agencies and the person themselves. A randomised trial of caregiver training comparing Mindfulness-Based Positive Behavior Support (MBPBS) and PBS alone demonstrated that both interventions were effective in reducing ‘challenging behaviours’ as well as other outcomes, though MBPBS showed greater improvements (Singh et al., 2020). By combining PBS with mindfulness-based practices, MBPBS teaches caregivers to reduce their own stress by viewing and responding to behaviour in a mindful manner (Singh et al., 2020). Organisational contexts can also have a major influence on ‘challenging behaviour’, as well as on the use of restrictive practices. In a longitudinal evaluation of an organisational change effort to minimise restraint and seclusion, Craig and Sanders (2018) reported marked decreases in the use of restrictive practices, reduced staff injuries from restraints, and increases in client goal mastery. Organisational factors such as the culture of an organisational environment (e.g. perceived purpose, regard for residents) can also be key to resident quality of life (Olivier-Pijpers et al., 2019).
In addition, contemporary evidence on behaviour change in the wider population backs a shift away from targeting individuals’ behaviours towards a focus on environments. Historically, many behaviour change interventions in public health focused solely on increasing knowledge and awareness – for example, telling people to exercise and improve their diet in order to lose weight. However research has demonstrated that this emphasis on individual capabilities and motivation fails to lead to sustained benefits for many people (Davis et al., 2015). Being able to exercise and eat well also requires conducive environments, such as having enough time and money to buy and prepare healthy meals (or someone who can facilitate this), and availability of safe and accessible spaces for exercise.
That is, improving population health also requires ‘swimming upstream’ to address the wider social, environmental and cultural factors that determine an individual’s health (Kiran and Pinto, 2016). Behaviour change interventions are thus more effective in improving population health if they simultaneously target different levels (e.g. individual, community and population) (NICE, 2007) This multitiered approach is used as the basis for the field of school-wide positive behaviour interventions and supports (SWPBIS), which has been identified as an effective way to reduce school discipline and increase academic achievement (Lee and Gage, 2020). SWPBIS explicitly focuses on primary prevention at the level of the wider school environment by providing universal supports for all students, such as developing a school‐wide recognition system for appropriate behaviour, with secondary or tertiary behaviour support intervention only as needed (Lee and Gage, 2020)
Yet, the growing recognition of the importance of ‘environments’ does not mean that behaviour change interventions always, or even often, place social context front and centre (Holman et al., 2018). Like interventions for the wider population, addressing multiple ‘environments’ for a person with disability is more complex and difficult than just focusing on the individual and their needs alone to reduce ‘challenging behaviours’. However, we argue this reorientation towards environments is needed to shape behaviour support practice in a way that is more aligned with a human rights-based approach.
Putting human rights at the centre of positive behaviour support
The CRPD overwhelmingly emphasises removing barriers or changing environments in order to promote the full participation in society by people with disability. By locating the main problem in societal factors external to the individual, the CRPD reflects the social model of disability (Lawson and Beckett, 2021). However, the CRPD also applies a human rights lens to disability in acknowledging that societal barriers are only one part of the puzzle – that is, even once these barriers are removed, many people will still need support to enjoy their inherent human rights on an equal basis with others. Since impairments are diverse and environments shape people in different ways, the support each person needs will be unique. The person with disability themselves is therefore the expert on what that support should look like. Further, because impairment is an expected dimension of human diversity, societies have a responsibility to advance social justice for people with disability.
In many ways, PBS aligns with the CRPD in being a values-based approach that seeks to promote and protect the person’s rights through its emphasis on improving quality of life (Chan et al., 2011). However, the biopsychosocial model that is widely recognised as underpinning PBS (Gore et al., 2022) may not be the most suitable for supporting a pivot away from focusing on the person as the source of the difficulty and proactively advancing social justice. The biopsychosocial model suggests ‘challenging behaviour’ results from vulnerability factors, including some inherently biological but mainly psychosocial risks, as well as the social processes that maintain behaviour. A limitation of this model is that it does not explicitly identify ‘environments’ beyond inter-personal interactions; this is subsumed into the ‘psychosocial’. Where the function of a behaviour stems from an aspect of the environment, such as the culture of a supported living home or a policy of locked doors in residential aged care, positive behaviour support strategies that focus solely on the biopsychosocial may not be compatible with a human rights approach.
French et al. (2010) suggest that an increased human rights focus means that clinicians and service providers working with people who have ‘challenging behaviour’ will be exposed to a more intense scrutiny of treatment and service interventions from a human rights perspective, as distinct from a clinical one. They suggest that affirmative human-rights related objectives should be explicit in service provision, and that new methodologies will be needed to make this practice fit-for-purpose with the CRPD. Below, we outline how an existing model could be used as a framework to help shift behaviour support practice towards ‘environments of concern’, and in doing so, better align with the human rights approach.
The social-ecological model as a tool for positive behaviour support
The ‘social-ecological model’ (McLeroy et al., 1998)) is one framework that could be used as a tool to support a paradigm shift in both terminology and the practice of PBS. Social-ecological models were first introduced by sociologists in the 1970s as a way to explain child development (Kilanowski 2017), and developed as a reaction to the perceived narrow scope of research of developmental psychologists at the time. The aim of these models was to bridge the gap between psychologists’ behavioural theories that tended to focus on the inherent nature of the child, and ‘big picture’ anthropological theories. That is, they were trying to address the complex interplay between intrapersonal factors and environmental factors in child development.
The model outlines how individuals’ behaviour may be influenced by internal factors such as health needs (e.g. pain) or previous experiences of trauma (Hastings et al., 2013), as well as social or interpersonal factors like how support staff interact with and respond to the person. It also allows for considering the bigger environments around people that are known to impact behaviour and wellbeing, such as the design of the built environment (Roos et al., 2022)); the culture of organisations in their approaches to behaviour support, including at the executive level (Olivier-Pijpers et al., 2019); the wider community and society norms around ‘acceptable’ behaviours and inclusion; and the public policies that shape all of these environments and ensure that people’s needs are met (or not). For practitioners and providers who implement PBS, a social-ecological approach to assessment and behaviour support planning might therefore include tools that explicitly aim to understand or address both social and physical environments (e.g. Limbu et al. 2021, Smith et al., 2012) or things like organisational culture (e.g. Craig and Sanders, 2018).
Like the CRPD and human rights approaches generally, the social-ecological model locates the main ‘problem’ in societal factors external to the individual, while still placing the individual at the centre stage. However, a true rights-based approach also needs to emphasise self-determination, choice and autonomy (UN CRPD 2006) in developing responses to ‘challenging behaviour’ both at the individual and population level. This means allowing people with disability to determine for themselves if a behaviour is ‘challenging’ or a ‘normal human response’ (Swaffer, 2018), and the right to make their own choices and decisions, even when those decisions could put them in harm’s way (dignity of risk) (Marsh and Kelly, 2018). For those working at a system level in PBS research and policy, it also means not just consultation with people with disability but co-creation of solutions, and a bigger picture focus on advancing social justice. A pivot further towards a human rights- and environments-based agenda in PBS will require reconceptualising how future professionals are trained, building on traditional person-centred practice to develop a workforce with additional skills as system-level change agents (Vera, 2020).
Conclusion
There is an urgent need for a reframing of ‘challenging behaviour’ so that people with disability are viewed, assessed and responded to in ways that are person-centred, evidence-based and with human rights and dignity at the core. The social-ecological model is one tool that may be useful in developing responses that explicitly focus on ’environments of concern’ to improve the wellbeing of people with disability who have behaviour support needs. While any new terminology that is adopted to decrease stigma and increase understanding likely will, through common usage, become stigmatising in its own right, there is value in continuing a robust discourse in relation to how we understand and discuss behaviour of people with disability.

delirium? Relatives’ experience of delirium in the intensive care unit: A qualitative interview study. Intensive and Critical Care Nursing, 53, 84-91.
Introduction
The incidence of delirium in intensive care units (ICU) ranges from 45 to 87% and appears to be strongly influenced by mechanical ventilation in critically ill patients, as this is an important risk factor for delirium (Cavallazzi et al., 2012). Delirium is defined by the American Psychiatric Association in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) as a disturbance in attention and awareness with additional disturbance in cognition (American Psychiatric Association, 1995). The condition develops over hours to days and fluctuates throughout the day and cannot be explained by pre-existing neurocognitive disorder (American Psychiatric Association). Delirium in ICU is related to the risk of morbidity, length of stay in hospital and mortality (Salluh et al., 2015). An evidence-based multicomponent bundle has been proposed in the literature and is associated with reduction in delirium in ICU (Barnes-Daly et al., 2017). The evidence-based bundle consists of the following steps: A: Assessment, prevention and management of pain. B: Both spontaneous awakening and breathing trials. C: Choice of sedatives and analgesia. D: Delirium assessment, prevention, and management. E: Early mobility/exercise. F: Family engagement and empowerment (Marra et al., 2017; Ely, 2017; Pandharipande et al., 2017). Despite that the ABCDEF bundle has evolved to include, ‘F’, family engagement as a part of the bundle of how to manage critically ill patients and prevent delirium, there is a lack of research to investigate the thoughts and perspectives of relatives on their experiences of witnessing delirium (Marra et al., 2017; Marandi et al., 2017). Recently, a multinational, interprofessional perspective on what research is needed in the field of ICU delirium concluded that family experiences should be explored in future studies (Pandharipande et al., 2017).
Relatives play a vital role for patient recovery why knowledge of the relatives’ experience of delirium in ICU is needed to identify relative’s needs and provide new insights to be considered while delivering the bundle of care primarily for the critically ill patients but may also benefit of relatives as well. The aim of this study was to explore relatives’ experiences of ICU delirium in critically ill patients.
Methods and materials
Design
A qualitative semi-structured interview study design with a phenomenological approach was used to collect data from relatives of critically ill patients with delirium in an ICU setting. The study is reported in accordance with the Consolidated Criteria for Reporting Qualitative (COREQ) research checklist (Tong et al., 2007). Phenomenology investigates the lived experience and the life-world of a person to achieve a deeper understanding of the person’s everyday life existence (Laverty, 2003). In methodology, phenomenological research is descriptive and focuses on the structures of experience and seeks to elucidate them as they appear in consciousness (Laverty, 2003).
Preunderstanding
The researchers must strive to achieve phenomenological reduction and be aware of their own impact on the material in order to be loyal to the experiences of the participants without the researchers’ interpretations. However, a complete phenomenological reduction in its pure form is considered to be unachievable in practice, but by making the researchers preconceptions visible, it is thereby kept at a distance (Malterud, 2011).
We remained conscious of our own preconceptions from our background in nursing and medicine, and from working with delirious patients and their relatives in ICU. From our knowledge of the serious risk of consequences of delirium for ICU survivors and experiencing delirium to be a major center of attention for the nurses and physicians in the ICU, we initially expected this to be reflected in the description from the relatives.
Participant recruitment
To be eligible for study participation, the participant had to be a relative of a patient (18 years) admitted in ICU for at least 48 hours and having delirium by DSM-IV identified with a positive score by Confusion Assessment Method for the ICU (CAM-ICU) (Gusmao-Flores et al., 2012), at least during two days of their ICU stay. Inclusion criteria for relatives were that they were an adult (>18), and a spouse, family member or close friend with a patient with the above criteria. Relatives were excluded if they lacked the capacity to consent, or if they did not speak Danish fluently. Non-participation and the reason for people refusing to participate or to reconsider participation was registered.
Potential participants received information about the study through a researcher and handout pamphlets, if they were agreed to be contacted. In the information the term delirium was used as a term but was not fully explained to minimize the influence on the later responds during the interview.
Setting
The study was carried out in a Danish 11 beds general medical/ surgical level II ICU at Herlev XXX Hospital, Herlev. The unit had a 24 hour a day open visiting policy and all patients stayed in single patient rooms. Patients in the ICU received standard medical and nursing health care, that included a delirium-bundle. Nurses and physicians at the unit had received instructions to the bundle before the study started. The bundle was focussing on pain management, no/light sedation, twice a day a routine of delirium assessment using the CAM-ICU, circadian rhythm/sleep, and early exercise.
Data Collection
The interviews were conducted from December 2017 to April 2018 using an interview guide with ten research questions . Questions were generally broad and open ended and followed the structure of Method of Phenomenological Interview based on themes of experience contextualisation, apprehending the phenomenon and its clarification (Bevan, 2014). Content validity of the interview guide was gained by a review of the literature, clinical experience of both the research team and fellow nurses from the ICU. A pilot testing on two relatives was made with subsequent modification of the wording of the questions. The modification consisted primarily of adding synonyms to the wording of the questions, as relatives was not familiar with delirium as a term. The clarification of delirium came after the second question in the interview guide.
The participants were interviewed at the hospital at their preference. Interviews were recorded using a digital voice recorder. Field notes were taken to document issues that could not be captured by audiotape such as the participants’ gestures or facial expressions. All interviews were transcribed verbatim and organised with NVivo 11.4.2 software. Data saturation was discussed between the researchers to clarify when themes were recurring and no new themes seemed to emerge, then the inclusion of new participants was stopped. After the interviews, the participants were asked to complete a short, written questionnaire to provide basic demographic details and background of being a relative in the ICU.
Data Analysis
Analysis was based on Kirsti Malteruds description of a four-step systematic text condensation (Malterud, 2011; Malterud, 2012): 1) The text was read several times to obtain an overall impression of experiences related to delirium in ICU from which the preliminary themes emerged. 2) Units of meaning were identified based on preliminary themes and sorted into code groups across individual participants. 3) Condensing all code groups was sorted in subgroups to visualize different perspectives. 4) Finally, categories were made based on a summary by the essence from code groups (Malterud, 2011; Malterud, 2012). The four steps of systematic text condensation analysis method are described and illustrated through an example of the process of the analysis (Table 2). All authors participated in analysing the data and finding categories through discussion. Quotes were chosen on the bases of what clearly represented issues of what was mentioned in the results.
Ethics
This study complied with the Declaration of Helsinki. Prior to participation written and verbal information was provided and participants were required to give written consent. Danish Data Protection Agency approved the study (I-Suite no.:06022, ID-no.: HGH-2017-113). According to Danish law formal approval of qualitative studies is not necessary, however we notified the Ethics Committee in the Capital Region, Denmark (file no 17029440). Every interview ended with a short session of debriefing and in cases where it was relevant the interviewer helped to initiate a meeting between relevant health care personal and the relative. This was relevant in two cases.
Findings
Participants
In total 11 relatives were interviewed, eight during ICU admission and three the day after the patient was transferred to the ward. The interviews lasted between 28 and 59 min.
Categories
Three categories emerged from the analysis.
Category 1: Delirium is not the main concern
This category refers to relatives’ knowledge and preunderstanding of delirium, and how this condition was found to be a natural consequence of critical illness and was considered secondary among other concerns.
Pre-understanding of delirium
Most of the participants had never heard about delirium as a term used in ICU. They had experienced the patient being different or doing/saying things out of the ordinary and from health staff this condition was spoken off as ‘‘being confused”, ‘‘having fatigue”, ‘‘being sad or restless”.
"Most of them [health care professionals] did not say anything. But when they did say something about it [delirium] they said, ‘he is a bit sad today’, ‘he is a little confused today’, ‘he is very tired today’. These were the words that were used." (Informant 10)
Participants had different pre-understandings of delirium as a term. Typically, participants associated delirium with alcohol withdrawal or alcohol intoxication, but not in a context related to the ICU. Some participants explained they had looked the term delirium up to gain some knowledge about the phenomenon prior to the interview. Some participants referred to family members or colleagues who had had a relative in an ICU and from this they had some knowledge of delirium. The exploration of knowledge about delirium took place for some participants before they were asked to participate, and for others they had not heard the word before they were invited to participate in the study.
"I have never heard the word before! I read this [information material from the project], I do know what delirium is, it’s some abstinence that you’ll get if you have drunk too much, right? But I am not sure. Nobody has never mentioned that word." (Informant 10)
Delirium as a natural consequence
"I think it [delirium] has something to do with him being unconscious for so long. Just like all the other organs, that his body has been shut down, the kidneys have shut down or something like that. Maybe it could be that the brain needs some kind off reset. You could say it needs to get running again. That’s what I think about it." (Informant 4)
There were many narratives where participants had an explanation to what they believed had caused delirium. These were mainly created from the relatives’ own hypothesis and some from information given by health care professionals. Typically, participants attributed the causes of delirium to the effect of drugs, ventilator treatment or the patient being afraid.
"Well, I think there are many factors. Partly, that he has had difficulty breathing...he has had extremely high oxygen supply. Partly, that he suffers from anxiety." (Informant 6)
Delirium is secondary to life and death
For most of the relatives, delirium was not the main concern in ICU. The greatest concern was whether the patient would survive and in that context symptoms of delirium were dealt with later on.
"But in some ways, you realised that as ill as he was, the delusions were not the most important thing at that time. It was that he was breathing and surviving. So, the brain could be taken care of afterwards." (Informant 2)
Category 2: Communication with health care professionals is crucial
This category refers to relatives’ experiences of the way delirium is communicated in the ICU. As we found delirium was an unfamiliar term for relatives, health care professionals communication about delirium influenced relatives perception of it.
Health care professionals don’t seem to worry about delirium
Typically, participants were in general well-informed about the overall condition of patient, but issues related to delirium were left unspoken. This left participants with the impression that delirium was not a central concern of health care professionals.
"They haven’t talked to me about it [delirium], because then I would have remembered something about it, and they have not. But otherwise, they have informed me about the medication and the physiotherapist and they were going to do this and..." (Informant 5)
Overall, there was incongruence in relation to how participants experienced the talk of delirium and what approach health care professionals had to it. One participant, who had been a relative to a patient with severe symptoms of delirium over several days, experienced health care professionals handling delirium in several different ways (i.e. one physician increased the dose of haloperidol and shortly after the medical treatment was stopped by another) and with different impressions of the severity depending on which doctors and nurses were on duty. Few participants had heard the term: ‘delirium’ used directly and in these cases relatives were told by health care professionals that it was a normal condition in ICU and health care professionals gave the impression that it was not a serious condition and it was temporarily.
"...the nurse came and said, ‘can you feel she’s different?’ So, I said, ‘Yes, I can. She is irritated and...restless...and angry about all this’. So, she said to me, ‘Well, this is delirium. You should not be worried about it. It will pass’." (Informant 7)
Medication as the articulated treatment of delirium
Most of the participants mentioned the pharmacological treatment, but did not talk about non-pharmacological approaches and said they did not notice anything being done. They said, they would like to be involved if they could do anything to diminish symptoms of delirium, but nobody experienced an invitation to become involved. "Well, it has mostly been on the medical treatment that you could see that they have tried to treat it. I can’t think of anything more... Some have been good, telling him what they were doing around him and said, ‘Now I’m just right behind you and will make some noise’. Explaining what they were doing might make him feel more comfortable." (Informant 6)
Need for information
Participants seemed to become increasingly aware of the lack of knowledge they had about delirium during the interview. If they had had the possibility, they would have preferred more information and expressed a need for information specifying pathologies, possible treatments and assumed causes. Information about delirium was beneficial by dialog with health care professionals or/and standard written information.
"Is it a normal situation? How common is it? Is it rare? Is it critical? Is it not critical? Is it dangerous? Is it not dangerous? I want to know what it is." (Informant 11)
Although, several relatives wished for more information about delirium, some said they were of the impression they could ask nurses and physicians about delirium if they wanted to, but often they didn’t. As one participant described there were plenty of other things to be concerned about.
"If I had asked more about it, then perhaps they would have told me more. But I thought...my impression was, that they handled it well. I thought so." (Informant 2)
Talking about it is a relief
The few participants who experienced being informed by health care professionals about delirium as a condition, described it as being a relief as it helped them to process the changes in patients’ awareness or attention they already were witnessing. Explanations about delirium that were recognisable and learning it is a well-known condition in ICU that health care staff are used to treat was considered reassuring.
"I was relieved when I heard about delirium because it explained what I have been seeing. I’m not an expert in this area, but I could see he was not himself." (Informant 6)
Category 3: Delirium impacts on relatives
This category refers to what the participants experienced when they witnessed symptoms of delirium for the first time and the way it affected them.
First encounter with delirium
The first sign of delirium was noticed by relatives at very different time points during the period of hospitalization. Some relatives initially said they had not noticed any delirium, however, when they talked about what they had experienced they described symptoms of delirium (e.g. different strange behaviour, irritated or agitated behaviour etc.), they just did not recognize it as delirium at the time.
"I thought she was very restless, and I thought it was strange that she pulled in the lines [IV-lines, monitoring-lines]. I thought, why is she doing that? And I said, ‘you must not pull in all the lines’." (Informant 7)
When the patient is like a stranger
Some described the patient had become as a stranger. In cases where they could not recognise the patient behind the changes in attention and awareness, it seemed to affect and bring concerns to a higher level. One relative described the patient as being mentally absent, which the participant said was the most worrying part.
"It’s not the person that I knew before he came in [to Hospital]. That’s what worries me the most." (Informant 8)
In contrast, some participants seemed content if only the patient could recognize the family members. They experienced symptoms of delirium like an extension of the patient’s personality, which made it easier to cope with.
"He has been confused about where he was and what had happed, and what floor he was on. Well, he has been able to recognise us who have come visit him. He has been able to do that all the time. I have had the feeling, he was himself, behind that blurry, very weakened state he was in." (Informant 2)
Ways of coping
As recognition of delirium differed among the relatives, it affected participants ways of coping in various ways. Several participants described how they tried not to demand too much of the patient, and some were precautious of what they said to the patient as they did not want to create more worries or anxiety. They balanced between just letting things slip or correcting if the patient said or did things that were abnormal.
"I am trying just to let it go, unless there is something that can be said, ‘it’s like this and that’, then I would tell him, and then he’ll say, ‘oh, yes’...So I won’t let him drive out in that nonsense...I will just follow all the nonsense, unless it is totally chaotic." (Informant 2)
What about the future?
Most relatives expected the patient to recover from delirium, but still most of them were filled with uncertainty if that really was true and what the future would bring. These kinds of thoughts were mainly described by participants with patients who had survived the most critical state of illness, which seemed to open up thoughts of long-term consequences.
"...things are difficult, but...but I wonder a lot about how it’s going to be at the end. It’s clear, if he continues to be a bit strange in his head, to say it straight out, I would be really upset about that. But I don’t think so...because some things he says, shows me he is there." (Informant 4)
Discussion
Main Findings
‘Delirium is not the main concern’
Findings indicating that relatives have little knowledge about delirium have been found in studies from non-ICU settings (Toye et al., 2014; Namba et al., 2007). Toye et al. (2014) indicated in a qualitative study from a hospital ward setting, that the lack of understanding of the patient’s delirium condition challenged the relative’s wish to participate in the treatment of the patient (Toye et al., 2014). Furthermore, a need for information was also constantly demonstrated, and relatives sought information elsewhere, because this need had not been met by health care professionals (Toye et al., 2014). In present study relatives also sought information elsewhere. However, some of them where first aware of their lack of knowledge when they were introduced to the term delirium during the invitation to participate in the study.
Furthermore, a need for information was also constantly demonstrated, and like this present study, relatives sought information elsewhere, because this need had not been met by health care professionals (Toye et al., 2014). Relatives in our study considered symptoms of delirium to be a natural consequence of critical illness, in consistence with a qualitative study in a non-ICU setting of relatives of terminally ill cancer patients with delirium, that also recognized delirium as a natural part of the process in critical illness (Namba et al., 2007). In contrast to our study, relatives in non-ICU settings seemed to have delirium as a main concern (Namba et al., 2007; O’Malley et al., 2008; Day and Higgins, 2015). It is possible that this difference in results may be related to timing. Many of the participants in our study were interviewed during a critical state of the patients’ condition, where it was first and foremost a matter of survival.
‘Communication with health care professionals is crucial’
The lack of communication and the need for health care staff to be more communicative about delirium has been identified consistently in other studies in non-ICU settings (Namba et al., 2007; O’Malley et al., 2008; Smithburger et al., 2017). In line with our study, other qualitative studies in ICU settings found that relatives have a desire to be involved in the care of the patient in general (Smithburger et al., 2017; Garrouste-Orgeas et al., 2010; Azoulay et al., 2003). Providing information to relatives has been shown to be an effective way of improving relatives’ satisfaction and comprehension and gives the relatives the opportunity to actively participate in the care of the patient (Azoulay et al., 2002). Furthermore, this could help relatives in ICU to gain control by building reasonable expectations about patient outcomes and to cope with possible distress (Azoulay et al., 2002; Maillet et al., 1993). Better comprehension does not generate more symptoms of anxiety or depression in the relative in ICU (Azoulay et al., 2002). It has even been seen to be able to reduce the distress of relatives by providing knowledge and tools to make them participate in care giving (Skoog et al., 2016). This is in line with the relatives in this present study who had been informed of delirium as they described information about delirium as a relief. It helped them to verbalise what they already could see was different and difficult to understand and handle. Relatives in our study described a need for information about delirium, in context of dialog with health care professionals as well as standard written information. In a study from a hospital ward written information about delirium was available, however, relatives emphasised the need for dialogue with health care staff (Toye et al., 2014) as the written information cannot stand alone.
As in all other respects, the health care professionals approach to relatives and patients should be caring and respectful when informing of delirium. However, health care professionals must be aware of the consequences of delirium in ICU that is related to the risk of morbidity, prolonged length of stay in hospital and increased mortality (Salluh et al., 2015). So, for many cases it is not just a condition that will pass, as one of the participants said she where told.
‘Impact on relatives’
In line with present study, Smithburger et al. demonstrated that relatives intuitively had ideas of their own on how to cope with delirium in ICU, although it was not something they had discussed with health care professionals (Smithburger et al., 2017). Garrouste-Oregeas et al. found in ICU settings that almost all relatives (96%) wanted to be a part of the care of the patient, but only a few started an activity on their own (13%) without counselling with health care professionals (Garrouste-Orgeas et al., 2010). This underlines that despite relatives willingness to take part in actions to reduce delirium, it is of great importance that they are guided by health care professionals. Moreover, involvement of relatives has shown to be an effective way of eliminating delirium and has a potential to prevent or shorten episodes of delirium (Rosa et al., 2017). In line with our study, other studies from non-ICU settings discover various findings in the relative’s experiences of delirium (Toye et al., 2014; Namba et al., 2007; Day and Higgins, 2015). Namba et al. (2007) described that some relatives thought that the patient was the same as usual even when the patient was delirious. Opposite in other studies relatives describe the delirious person becoming strange and unfamiliar (Day and Higgins, 2015). Confirming that delirium may appear in different clinical ways and be perceived in just as many by relatives. Unlike this present study, relatives in non-ICU settings seemed to be more affected by the patient’s delirious condition, especially when it came to speculation about the future (Toye et al., 2014). This indicates that focus moves when the patients most likely have overcome the life-threatening situation, why ICU nurses must prepare relatives for this.
Methodological Considerations and Limitations
To our knowledge this is the first study to examine how relatives experience delirium in the critically ill patient in ICU. The qualitative methodology used is a valid design to reveal relatives experience of delirium that cannot be captured by quantitative methods. Credibility of this study was strengthened by investigator triangulation during analysis with varying backgrounds in professions and experience that ensured a broader understanding of the phenomenon. Furthermore, the transparency of every step in the data analysis is reported in Table 2 and demonstrates how interpretation was grounded in data.
The qualitative methodology is not valid in making generalisable results. However, results can be transferable as participants seem to have a demographic data similar to the literature of relatives in ICU, in relation to the higher rate of female relatives, age and proportion between spouses and other relatives (Bohart et al., 2018). This is a single centre study why results need to be interpreted in the local context.
We approached and asked 18 relatives to participate and 11 agreed. The main reason for non-participation was a lack of energy due to the critical illness of the patient. Similar non-participation rates and reasons have been found in studies with relatives in ICU’s (Bohart et al., 2018; McAdam et al., 2012). Studies have shown that non-participants usually have less resources than participants (De Jong et al., 2004; Rosted et al., 2016). This perspective must be taken into consideration as our results might overestimate relatives’ ability of coping with the illness of the patient.
Conclusions
The findings of this study provide a new insight into relatives’ experience of delirium in an ICU setting. Relatives have sparse knowledge of delirium as a concept. Symptoms of delirium were described as a natural consequence of critical illness in a patient and seemed to be a secondary problem in the context of ICU. When healthcare professionals did not talk about delirium, relatives perceived it as if delirium was unimportant. However, in hindsight information about delirium was requested by relatives, as this was found to give them a sense of better understanding and relief. Delirium and the manifestation of it was experienced in different ways and brought different ways of coping forward. Uncertainty of possible long-term consequences after hospital admission appeared. When ICU in the future are approaching delirium by evidencebase bundles, we emphasise the importance of the ABCDE-bundle also includes relatives by adding the F, family engagement. Further investigation is needed to extend the knowledge of relatives’ experiences of delirium as future research must investigate the potential in helping relatives to engage and cope with delirium, to the benefit of both patient and relatives.

Fazio, S., Pace, D., Flinner, J., & Kallymer, B. (2018). The fundamentals of person-centered care for individuals with dementia. The Gerontologist, 58(1), 10-19.
Overview of Person-Centered Care for People with Dementia
Origins of Person-Centered Care
The term person-centered care has its origins in the work of Carl Rogers, which focused on individual personal experience as the basis and standard for living and therapeutic effect. Tom Kitwood first used the term in 1988 to distinguish a certain type of care approach from more medical and behavioral approaches to dementia. Kitwood used the term to bring together ideas and ways of working that emphasized communication and relationships. Kitwood (1998) proposed that dementia could be best understood as an interplay between neurological impairment and psychosocial factors, namely, health, individual psychology, and the environment, with particular emphasis on social context. He believed that the environment has as much effect on the brain as the brain has on a person’s abilities. Fundamental to Kitwood’s theory was a rejection of the standard medical approach to dementia, which focused on rigidly treating a disease. He believed that the basic assumption in the medical sciences of dementia carried far too negative and predictable implications for the nature of caregiving.
Kitwood and Bredin (1992) shared evidence from studies of different care practices, suggesting that dementia does not universally progress in a linear fashion, and most importantly, it varies from person to person. They concluded that the person with dementia is in a state of relative well-being or ill-being, and that indicators can be observed through detailed observation. They found a need for highquality interpersonal care that affirms personhood; one that implies recognition, respect, and trust. The approach that Kitwood and Bredin developed to fill this need was person-centered care. Philosophically, they looked at what persons with dementia need and determined that the answer began with love at the center surrounded by the following five offshoots: comfort, attachment, inclusion, occupation, and identity (Kitwood, 1997). Individuals need comfort or warmth to “remain in one piece” when they may feel as though they are falling apart. Individuals with dementia need to feel attachment when they so often feel as though they are in a strange place. Individuals need to be included and involved both in care and in life, and more than simply being occupied; they need to be involved in past and current interests and sources of fulfillment and satisfaction. Finally, people with dementia need to have an identity and their caregivers must help maintain this identity (Kitwood, 1997). As Kitwood (1997) stated, “To have an identity is to know who one is, in cognition and in feeling. It means having a sense of continuity with the past; and hence a ‘narrative,’ a story to present to others” (p43). Due to declining cognition, persons with dementia need others to “hold their story” and to respond to them as “thou, in the uniqueness of their being” (Kitwood, 1997).
Kitwood (1997) developed a conceptual approach to care that provides staff with a way of thinking about what they do according to principles that guide care and reinforce or support personhood and well-being throughout the course of dementia. Rather than simply providing care in accordance with routines organized for staff convenience, efficiency, or some other criteria, Kitwood (1997) suggested that the focus should be on the person who is the recipient of care. Kitwood’s framework encourages staff to focus less on what is done and more on how it is done. Kitwood’s principles assist those who provide care to critically evaluate how programs and communication strategies can be adopted and implemented to support the multidimensional person with dementia.
Selfhood and Person-Centered Care
At the core of person-centered care is the self—who we are, our values and beliefs, etc. Selfhood is much more than memory and should not be viewed only in terms of cognitive abilities. Recognizing and maintaining selfhood is key to person-centered care. Researchers have found intact manifestations of selfhood in spite of significant cognitive impairments and that it is not intact autobiographical memory that constitutes self or personal identity (Sabat & Harré, 1992; Sabat & Collins, 1999). Sabat and Harré (1992) revealed through case studies that the self of personal identity persists far into the end stage of AD. Sabat and Collins (1999) suggested that the multiple personae presented in public and in relationships can be lost, partly as a result of how others treat and view the person with AD. Thus, losses in aspects of selfhood might be traced, in part, to dysfunctional social interactions rather than solely the neuropathology of Alzheimer’s disease. Based on findings suggesting a connection between self and interactions with healthy others, Sabat (2002) concluded that it is possible—through discourse, or language—to observe intact selves in individuals with AD. He also suggested that a self of social identity could be seen by the attributes or characteristic that one possesses, and a self of personal identity by pronouns used.
Building on Sabat’s research, Fazio and Mitchell (2009) quantitatively evaluated the persistence of self in persons with dementia through language use and visual self-recognition. They found that although overall frequency of language usage declined across impairment levels, there were no significant differences in either rates or proportions of pronoun and attribute usage. This suggests that it is not a loss of self per se that is responsible for a lower frequency of language usage, but more likely a decreased ability to initiate conversation. In addition, when individuals were asked to identify themselves in photographs, cognitively impaired individuals—in spite of forgetting the photographic session only minutes earlier—exhibited unimpaired self-recognition, consistent with a preserved self.
Others are an essential part of maintaining the self in people with dementia. When a person is seen as diminished due a decline in cognitive functioning, they can be treated as if they were no longer a human being and in nonhuman ways (Fazio, 2008). Kitwood and Bredin (1992) state that some of the most disabling effects of brain disease are to be found not in functional impairment but in the threats to one’s self and personhood. They believe personhood is dependent on other people. Recognizing that selfhood persists, learning about the complete self, and finding ways to maintaining selfhood though interactions and conversations are fundamental components of person-centered care for people with dementia.
Relationships and Person-Centered Care
Maintaining selfhood is a key part of building and nurturing relationships. Kitwood and Bredin (1992) discussed how interdependence is a necessary condition of being human. However, due to the Alzheimer’s disease, a dependence on others is a necessity for persons with dementia. The care provider becomes an absolute necessity, both physically and psychologically. This relationship is critical. Kitwood and Bredin (1992) explained that personhood can be ensured only within the context of a mutually recognizing, respecting, and trusting relationship. In his earlier work, Kitwood (1990) described 10 processes and interactions that tend to depersonalize a person with dementia, which include disempowerment, labeling, infantilism, and objectification. Words do matter, as language leads to perceptions, and ultimately approaches to care (Fazio, 1996). Labels depersonalize individuals and can lead them to be treated in ways that do not support their personhood.
Relationships with others do have a great impact on personhood. Kitwood and Bredin (1992) believe that the personhood of individuals with dementia needs to be continually replenished, their selfhood continually evoked and reassured. The other person, the caregiver, is needed to offset degeneration and fragmentation and sustain personhood. The further the dementia advances, the greater the need for “person-work.” The caregiver is needed to hold the pieces together to become the memory (Fazio, 2008). Kitwood and Bredin (1992) believe that this may be understood as the true agenda of dementia care. Care partners need to be the support that maintains the self and structure the environment and interactions within it to effectively do so. Knowing the person is central to care that is based in mutual trusting and caring relationship.
Key Components of Person-Centered Dementia Care
Researchers have worked to find commonalities among models and practices of person-centered dementia care. Levy-Storms (2013) conducted a literature review and found several commonalities among models and practices including (a) supporting a sense of self and personhood through relationship-based care and services, (b) providing individualized activities and meaningful engagement, and (c) offering guidance to those who care for them. Kogan, Wilber, & Mosqueda (2016) conducted an extensive literature review for definitions of person-centered care. They identified 15 definitions, addressing 17 principles or values. They found that the six most prominent domains were (a) holistic or person-centered care, (b) respect and value, (c) choice, (d) dignity, (e) self-determination, and (f) purposeful living. In all, it was clear that there is a shift in focus away from the traditional biomedical model in favor of embracing personal choice and autonomy.
Brooker (2004), a colleague of Tom Kitwood, has outlined one of the most respected descriptions. Brooker outlined that four key components are integral to a personcentered care approach for people with dementia and can result in a shift in practice and culture. These components are: (a) valuing and respecting persons with dementia and those who care for them; (b) treating people with dementia as individuals with unique needs; (c) seeing the world from the perspective of the person with dementia, so as to understand the person’s behavior and what is being communicated, and validating the subjective experience that is being perceived as the reality of the individual; and (d) creating a positive social environment in which the person with dementia can experience relative well-being through care that promotes the building of relationships.
In Person-Centered Dementia Care: Making Services Better, Brooker (2006) expanded upon these components and identified key indicators or practices for each of the four components. Key indicators in valuing care providers include having a clear vision, developing practices that value employees, creating systems to support staff development, designing supportive and inclusive physical and social environments, and ensuring quality improvement mechanisms. Key indicators of individualized care include developing and regularly reviewing care plans that reflect strengths and needs, allowing use of personal possessions, accommodating individual preferences and daily routines, learning about individual life stories, and offering a variety of activities. Key indicators in taking the perspective of the person with dementia include communicating effectively, experiencing empathy, monitoring the physical environment, assessing physical health, uncovering reasons for behaviors, and being an advocate. Lastly, key indicators for the social environment include treating individuals with respect, creating an atmosphere of warmth, validating feelings, providing appropriate support and assistance, and fostering a sense of community. Indicators such as these outlined by Brooker are important to consider as providers find ways to implement a person-centered philosophy within every day practices.
Examples of Person-Centered Care Approaches Throughout the Progression of Alzheimer's Disease or Related Dementia
Person-centered care in practice
Below you will find examples of person-centered care approaches throughout the progression of Alzheimer's disease or related demention.
Early
Tom has always been a very independent man. Although he was diagnosed with Alzheimer's disease, he want to remain as independent as possible. He goes through his day as he always did, although now his wife Joan is always there for support if needed. Joan sometimes has to assist with a task, help with finding the right word, or give a friendly reminder. She also continues to include Tom in decisions, including treatments, future care and finances.
Middle
Frank was a professional musician and played at all of the local and regional clubs. Since he played late night gigs, he was used to staying up late each night as well as sleeping late each morning. When Frank's care needs became too much for his wife, she looked for a memory care center that would support his life long schedule. In his new home, Frank stays up late in his rooms, oftentimes listening to old records. Staff let him wake on his own each morning and include that information in his care plan. Since there is a piano in the reception area, Frank often plays for other residents and visitors.
Late
Emily was an avid gardener. Her yard was perfectly kept with many varieties of plants, which she grew from seed. He loved fragrant bushes, especially lavender. One side of her yard was filled with beautiful bushes. Throughout the progression, she stayed involved in gardening. In the later stage of the Alzheimer's disease, care providers looked through seed catalogues with her, and talked about different varieties. They kept fragrant cut flowers and plants in her rooms, especially lavender when available. They kept a small satchel of dried lavender under her pillow, and also used a nice lavender lotion to moisturize her hands and feet.
Evolution of Person-Centered Care Models
Elements of person-centered care can be seen in the Federal 1987 Nursing Home Reform Act (OBRA ‘87). OBRA ‘87 states that each person receives the necessary care and services to attain or maintain the highest practicable physical, mental, and psychosocial well-being, in accordance with the comprehensive assessment and plan of care. Additionally, the culture change movement, consisting of models like the Eden Alternative, Wellspring, and Greenhouse/Small House, implemented various elements of what we now call person-centered care. One of the best known of these models is The Eden Alternative, founded by Bill Thomas. Its central mission is to eliminate the three ‘‘intolerable plagues’’ of nursing home life—loneliness, helplessness, and boredom—by following ten Eden principles, thereby improving elders’ quality of life (Thomas, 1996). One important strategy in this approach is to transform the physical institutional environment to be more homelike. Plants, animals, and intergenerational programs are included in the homelike environment to enhance the elder’s social engagement. The Green House or Small House model aims to provide a good quality of life for residents by transforming physical environments, radically revising staff configurations, and emphasizing companionship under normal rather than therapeutic circumstances (Li & Porock, 2014). Personcentered care is also an important component of the 2016 Centers for Medicare and Medicaid Service (CMS) Quality Strategy as noted in “Goal 2: Strengthen person and family engagement as partners in their care.” The objectives of Goal 2 are to ensure all care delivery incorporates person and family preferences, improve experience of care for persons and families and promote self-management.
Tools for Measuring Person-Centered Care Practices
A variety of tools to assess person-centered care practices currently can be found in the literature. Edvardsson and Innes (2010) conducted a critical comparative review of published tools measuring the person-centeredness of care for older people and people with dementia. The tools were compared in terms of conceptual influences, perspectives studied and intended use, applicability, psychometric properties, and credibility. Twelve tools eligible for review were identified; eight tools for evaluating long-term care for older adults, three for hospital-based care, and one for home care. One tool, Dementia Care Mapping (DCM), was dementia specific. Each tool explicitly aimed to measure forms of person-centered care as perceived by care recipients, family members, or staff. Edvardsson and Innes (2010) did recommend that their validity, reliability, and applicability be further explored. A brief summary of each tool included in their extensive review is provided below. Although most of them have not been specifically designed for individuals with dementia, their focus on knowing the person, interpersonal relationships and individual autonomy makes them relevant for assessing person-centered dementia care.
Specifically for long-term care settings, DCM (Brooker & Surr, 2005, as cited by Edvardsson & Innes, 2010) is an observational tool that uses four predetermined coding frames that aim to make the observer view the world from the point of view of the person with dementia. Coding frames of DCMs are as follows: mood enhancers (6-item scale), behavior categories (23 items), personal detractions (PD, 17 items), and personal enhancers (PE, 17 items). Items are rated on a 2-point scale ranging between “detracting” and “highly detracting” for PD and “enhancing” and “highly enhancing” for PE. DCM was developed through a systematic process of item development.
Also for long-term care settings, the Person-Directed Care Measure (White et al., 2008, as cited by Edvardsson & Innes, 2010) consists of 50 items covering eight domains of person-centered care and is divided into two dimensions: person-directed care and person-directed environment. Another tool, the Person-Centered Care Assessment Tool (P-CAT) (Edvardsson et al., 2010, as cited by Edvardsson & Innes, 2010) consists of 13 items in three subscales: personalizing care, organizational support, and environmental accessibility. In addition, the Measures of Individualized Care (Chappell, Reid, & Gish, 2007, as cited by Edvardsson & Innes, 2010) consists of three tools to measure individualized care. The first tool operationalizes the domain “knowing the person” (13 items). The second tool operationalizes “resident autonomy” (15 items), and the third tool measures “communication” (18 items). Lastly, the Family Involvement in Care (Reid, Chappell, & Gish, 2007, as cited by Edvardsson & Innes, 2010) consists of two measures of family involvement in the care of a relative with dementia in a long-term care setting. The first measure (20 items) measures to what extent family members perceive they are involved in the care of their relative. The second measure (18 items) measures the importance attached to being involved in the care of the relative living in long-term care.
Designed for hospital settings, the Person-Centered Climate Questionnaire (PCQ) (Edvardsson et al., 2009, 2010, as cited by Edvardsson & Innes, 2010) consists of two tools (staff and patient versions) to measure to what extent the psychosocial environment of health care settings is perceived to be person centered. The staff tool (14 items) consists of four subscales: safety, everydayness, community, and comprehensibility. The patient tool (17 items) consists of two subscales: safety and hospitality. Another instrument, the Person-Centered Impatient Scale (Coyle & Williams, 2001, as cited by Edvardsson & Innes, 2010), measures recipient experiences of care and contains 20 items in five dimensions: personalization, empowerment, information, approachability/availability, and respectfulness. Intended for home care settings, the Client-Centered Care Questionnaire (DeWitte et al., 2006, as cited by Edvardsson & Innes, 2010) is 15-item questionnaire that was developed to measure to what extent older people receiving home care experience the care as being client centered.
A few additional tools were found that were developed after the 2010 review of Edvardsson and Innes. Zimmerman et al. (2014) developed the PersonCentered Practices in Assisted Living (PC-PAL) in collaboration with the Center for Excellence in Assisted Living (CEAL) as part of a toolkit for person-centered care in assisted living. The PC-PAL includes one questionnaire for completion by residents, and one for completion by staff. They are research quality, evidencebased questionnaires to help organizations measure their person-centered practices and inform their quality improvement efforts. The Resident PC-PAL (49 items) includes four areas that reflect person- centeredness in assisted living: (a) well-being and belonging (18 items), (b) individualized care and services (12 items), (c) social connectedness (10 items), and (d) atmosphere (9 items). The Staff PC-PAL (62 items) includes five areas that reflect person-centeredness in assisted living: (a) workplace practices (23 items), (b) social connectedness (16 items), (c) individualized care and services (8 items), (d) atmosphere (8 items), and (e) caregiver-resident relationships (7 items).
In addition, the Advancing Excellence in America’s Nursing Home Campaign developed a Person-Centered Care Tracking Tool consisting of seven steps to success. The steps include (a) explore goal, (b) identify baseline, (c) examine process, (d) create improvement, (e) engage, (f) monitor and sustain, and (g) celebrate success. This tool includes spreadsheets, forms, links to resources, etc. to help gather data, make changes, and celebrate success. Lastly, Burke, Stein-Parbury, Luscombe, & Chenoweth (2016) developed the Person-Centered Environment and Care Assessment Tool (PCECAT) to assess and improve residential care standards using person-centered principles, while also meeting Australian care guidelines for older adults. The development included a review of existing assessment instruments and their alignment with person-centered principles and Australian dementia care quality standards—management systems, staffing and organizational development, health and personal care, resident lifestyle, physical environment, and safe systems. The tool successfully moved from concept to development and testing, proving to be valid and reliable. The tool is specific to Australian care standards but can be adapted for use in other countries. As shown, a variety of tools are currently available to measure person-centered care practices but more research and consistency is needed. It is important that tools continue to be developed and tested so we can consistently measure the outcomes associated with person-centered care practices.
Benefits of Person-Centered Care Approaches
Early research in person-centered care demonstrated measurable results. Epp (2003) highlighted several studies that revealed positive results from implementing personcentered care practices including improved quality of life, decreased agitation, improved sleep patterns and maintenance of self-esteem. More broadly, research in the application of person-centered practices and culture-change principles has shown how they can make life better for residents and improve working conditions for staff (Koren, 2010). Relatively simple interventions have produced measurable results—for example, keeping shower rooms warm can make bathing a more pleasurable experience for residents, reduce staff stress, and save time (Koren, 2010). Koren (2010) also stated that several management studies support the link between strategic human resource management and organizational performance, lending support for the organizational redesign called for by culture-change proponents.
Effects of Person-Centered Care Interventions on Individuals
Li and Porock (2014) provided a comprehensive review article that synthesized current evidence of the effects of multiple person-centered care models on resident outcomes. Systematic searches were conducted using various databases, using multiple keywords. Searches were limited to articles written in English and published from January 1990 to April 2013. In addition, a manual search of the reference lists of selected relevant articles was conducted. Twenty-four studies from three countries were reviewed and compared in terms of person-centered interventions, measurement, and resident outcomes. Fifteen culture change studies for residents who were cognitively intact or with minor cognitive impairment and nine studies for residents with dementia were reviewed. Across the studies, culture change models had some beneficial effects on residents’ psychological wellbeing. Person-centered dementia care had significant effects on decreasing behavioral symptoms and psychotropic medication use in residents with dementia in long-term care. The outcomes of these culture change and person-centered care studies outlined by Li and Poro
Culture Change Studies
Most of the 15 culture change studies focused on residents with intact cognition or with mild dementia and aimed to test a single component of a culture change model. Nine of the studies were guided by the Eden Alternative, two by Green House/Small House model, one by Wellspring, one by “resident-centered care,” one by “Social Care Model,” and one was conducted by Pioneer Network to test PCC principles. Across studies, there were challenges with weak designs, threats to internal and external validity, simplistic methods, and small biased sample sizes (Li & Porock, 2014). Residents’ cognition, quality of life (QoL), psychological wellbeing, physical wellbeing, and other care-related resident outcomes were measured in these studies. The effectiveness of culture change in terms of QoL, depression, loneliness, helplessness, boredom, and activities of daily living (ADL) was the major focus of all studies. Other outcomes examined included restraint use, pressure ulcers, infections, medication use, falls, and nutrition problems (Li & Porock, 2014). Three of the five studies that examined the impacts of culture change models on residents’ QoL found beneficial effects, including dignity, security, individuality, and autonomy (Li & Porock, 2014). Other studies illustrated impact on depression as shown by a significant decrease in the Global Depression Scale in both cognitively intact and cognitively impaired residents over time, and by lower levels of helplessness, boredom, and loneliness (Li & Porock, 2014). Activities of daily living were examined in four Eden studies and two Green House studies, showing a lower percentage of residents who were dependent in eating and lower incidence of decline in late-loss ADLs than residents in comparison groups (Li & Porock, 2014). In addition, physical restraint use was reported in five studies, with less physical restraint use was found in three studies (Li & Porock, 2014).
Person-Centered Dementia Care Studies
Li and Porock (2014) reported that eight of nine personcentered dementia care studies were grounded by Kitwood’s concepts. Seven of the nine person-centered dementia care studies developed individualized interventions based on understanding residents’ needs, histories, and wishes. Dementia care mapping was used to develop the personcentered dementia care interventions in two studies. Studies applied a variety of validated instruments to measure residents’ cognitive impairment, QoL, behavioral symptoms, affects, and other physical wellbeing (Li & Porock, 2014).
Behavioral disturbance was observed in eight studies. The five studies that used aggression or agitation as primary outcomes showed that interventions significantly decreased the challenging behaviors expressed by residents with dementia (Li & Porock, 2014). However, three studies that did not primarily target such behaviors nevertheless did achieve significant findings. Integrating results of these studies shows that person-centered interventions seem to be effective in decreasing agitated behaviors in residents with dementia (Li & Porock, 2014). Emotional disturbance, such as depression and affect, was measured in five studies. Overall, these studies showed that person-centered dementia care interventions helped to produce more positive affections but did not reduce depression symptoms (Li & Porock, 2014). Psychotropic drug use was evaluated in three studies, and a reduction of neuroleptic or antipsychotic use by the intervention groups was found in two of the three studies (Li & Porock, 2014). Lastly, four validated QoL measurements for people with dementia were used in two studies. However, the effect of person-centered dementia care on QoL in residents with dementia cannot be determined due to inconsistent findings (Li & Porock, 2014).
In short, of all the culture change studies, the Eden Alternative seemed to have some beneficial effects on residents’ psychological wellbeing, including depression, loneliness, helplessness, and boredom (Li & Porock, 2014). Studies also showed positive outcomes for effectiveness of culture change models in terms of QoL, ADL function, restraint use, and other outcomes, however more research is needed. In relation to person-centered dementia care studies, interventions had significant effects on decreasing behavioral symptoms, producing positive affect, and reducing psychotropic medication use in residents living with dementia in long-term care (Li & Porock, 2014). However, the effects of person-centered intervention on residents’ living with dementia QoL, depression, sleep, and other physiological outcomes cannot be determined based on the inconsistent results of the reviewed studies (Li & Porock, 2014).
Effects of Person-Centered Care Approaches on Staff
Barbosa, Sousa, Nolan, & Figueiredo (2015) conducted a review to assess the impact of person-centered care approaches on stress, burnout, and job satisfaction of staff caring for people with dementia in residential care communities. The review was limited to experimental and quasiexperimental studies, published in English and involving direct care workers. Seven studies were included and addressed different person-centered care approaches, including DCM; stimulation-oriented approaches, such as recreational therapy (storytelling) or multisensory stimulation (Snoezelen); emotion-oriented; and behavioral-oriented approaches. Of the seven studies, five assessed burnout, four measured staff’s stress, and three measured job satisfaction.
van Weert and colleagues, as cited by Barbosa et al. (2015), investigated the effectiveness of integrated Snoezelen on work-related outcomes of staff in nursing homes. Fritsch and colleagues, as cited by Barbosa et al. (2015), evaluated the impact of a group storytelling approach on people with dementia and care assistants. Finnema and colleagues, as cited by Barbosa et al. (2015), examined the effect of integrated emotion-oriented care (validation in combination with other interventions such as reminiscence and sensory stimulation) on both nursing home residents living with dementia and staff. Schrijnemaekers and colleagues, as cited by Barbosa et al. (2015), studied the effect of emotion-oriented care on staff through a pre–post randomized controlled trial (RCT). Wells and colleagues, as cited by Barbosa et al. (2015), implemented a behavioral approach consisting of training staff through five educational sessions to use an abilities-focused morning care routine with residents. Jeon and colleagues, as cited by Barbosa et al. (2015), implemented DCM through an RCT conducted in 15 care communities assessed the efficacy of DCM and person-centered care on staff stress and burnout.
Barbosa and colleagues (2015) stated that methodological weaknesses and heterogeneity among studies make it difficult to draw firm conclusions. However, five of seven studies reported benefits on dementia care workers, suggesting a tendency toward the effectiveness of person-centered care on staff. Each of the two RCTs that assessed emotion oriented approaches were successful in reducing direct care workers’ stress, burnout, and job dissatisfaction (Barbosa et al., 2015). However, emotion-oriented approaches were comprised of multiple components (e.g., validation and reminiscence), making it difficult to understand which one was the most effective (Barbosa et al., 2015). An additional RCT found that DCM positively affected direct care workers’ stress and burnout, and a nonrandomized controlled study based on multisensory stimulation showed immediate significant positive impacts on the three outcomes of interest (Barbosa et al., 2015). Finally, one of two behavioral-oriented approaches, which adopted a nonrandomized design, showed a reduced burnout in direct care workers (Barbosa et al., 2015). The remaining two studies reported no effects on staff’s psychological outcomes (Barbosa et al., 2015). As a group, these studies provide some of the strongest evidence available as the staff-related benefits of person-centered care models. Additionally, reduction in stress, burnout and job dissatisfaction may also lead to reduced staff turnover—a significant challenge within long-term care.
incorporated a range of different outcome measures to evaluate the impact of person-centered interventions on residents and staff. Brownie and Nancarrow (2013) found that person-centered culture change interventions were not homogeneous or single-element interventions. Instead, they incorporated several features including: environmental enhancement; opportunities for social stimulation and fulfilling relationships; continuity of resident care by assigning residents to the same care staff; changes in management and leadership approaches, with the introduction of democratized approaches to decision making that involve residents and staff; changes to staffing models focused on staff empowerment; and individualized humanistic philosophy of care (Brownie & Nancarrow, 2013). Brownie and Nancarrow (2013) found that the Eden Alternative was the only intervention identified in this review that articulated a framework (incorporating all features) for a person-centered approach to caring for older residents, and improving staff working conditions. In contrast, other types of person-centered interventions were community specific that focused on one or two features.
Three Eden Alternative studies met the inclusion criteria for this review. Two studies reported improvements in residents’ psychological well-being as measured by the prevalence of feelings of boredom, loneliness, helplessness, and depression in Eden Alternative communities (Brownie & Nancarrow, 2013). These studies found statistically significant reductions in these feelings (except loneliness) for residents in Eden Alternative communities when using validated psychological assessment tools (Brownie & Nancarrow, 2013). Coleman and colleagues, as cited by Brownie and Nancarrow (2013), found that environmental enhancement was actually associated with adverse outcomes for residents in an Eden Alternative community, compared with residents in a traditional (control) nursing home. They found that residents in the Eden Alternative community had a higher rate of falls (31% within a 30-day period) compared with controls (17%). In this study, the residents in the Eden Alternative community were on average younger than those in the control community (82.6 years of age vs 88 years of age), with fewer impediments in relation to functional status (Brownie & Nancarrow, 2013).
One Green House model study met the inclusion criteria for this review. This 2-year study compared residents in four 10-bed Green House homes with two comparison sites (Brownie & Nancarrow, 2013). The aim of the study was to determine the effects of the Green House model on residents’ quality of life (via interviews) and quality of care (via MDS data). After controlling for baseline characteristics, there was a statistically significant improvement in Green House residents’ perception of their quality of life, compared with the control groups (Brownie & Nancarrow, 2013).
Three community-specific person-centered care studies met the inclusion criteria for this review. Two of these community-specific approaches evaluated the impact of person-centered interventions on organizational and workplace characteristics in addition to residents’ well-being (Brownie & Nancarrow, 2013). According to Brownie and Nancarrow (2013), one study confirmed that personcentered care positively impacted nurses’ job satisfaction and work conditions, as well as improving their capacity to meet the individual needs of residents with dignity and respect. Furthermore, these person-centered approaches improved the continuity of residents’ care because they were more likely to be assigned to the same nursing staff and also led to increased social interaction between residents (Brownie & Nancarrow, 2013).
Lastly, Brownie and Nancarrow (2013) described a large Australian study that randomly assigned 289 residents across 15 care communities to receive person-centered care, dementia care mapping, or usual care. The communities were selected because they used a task-focused, rather than a person-centered, approach to care and were similar in terms of management structures, staffing, standards, and size. Agitation was significantly lower with both person-centered and dementia care mapping than usual care. However, the incidence of falls was higher in person-centered care than in usual care (Brownie & Nancarrow, 2013).
Brownie and Nancarrow (2013) concluded that forming accurate conclusions about the impact of personcentered interventions on residents and staff is hampered by the heterogeneity of the interventions and significant methodological differences between studies. However, person-centered interventions are associated with positive influences on staff outcomes (satisfaction and capacity to provide individualized care); improvement in the psychological status of residents (lower rates of boredom and feelings of helplessness); and reduced levels of agitation in residents living with dementia. However, it did appear that some person-centered interventions might be associated with an increased risk of falls in aged-care residents (Brownie & Nancarrow, 2013). While more research into the cause of increased risk for falls is needed, it may be possible that residents are more at risk for falls when they are ambulatory and active as opposed to being sedentary and prone to sitting or laying down for much of the day.
Shifts in Organizational Culture
As noted, person-centered care exists within the larger movement of culture change, a broad-based effort to transform nursing homes from interpersonal health care institutions into true person-centered homes offering long-term care services (Koren, 2010). After much work in the early 1980s among various organizations and advocates, the Pioneer Network took the lead in fostering the culturechange movement within nursing homes. Koren (2010) stated that culture change movement’s overarching goals are to individualize care for residents, making communities more homelike and less “institutional.” “It promotes person-centered care through reorientation of the community’s culture—its values, attitudes, and norms—along with its supporting core systems (such as breaking down departmental hierarchies, creating flexible job descriptions, and giving front-line workers more control over work environments)” (p2). In addition, it strives to honor residents’ individual rights, offering them quality of life and quality of care in equal measure. Culture change also recognizes the importance of all staff members’ contributions to the pursuit of excellence (Koren, 2010).
The culture-change movement espouses a set of principles, instead of offering a prescriptive set of practices or dictating conformance to a model. Early in the culture-change movement, there was a lack of agreement as to precisely how all of these changes would manifest themselves in a nursing home transformed by culture change. A gathering of stakeholders came together to develop a consensus that the “ideal” community would feature the following components: resident direction, homelike atmosphere, close relationships, staff empowerment, collaborative decision making, and quality-improvement processes (Koren, 2010). Over the years, various models have been evaluated and research has demonstrated results. However, there is still much work to be done to identify outcomes and support the overall business model.
Koren (2010) stated that several aspects of the nursing home field, including its workforce, regulation, and reimbursement, limit the initiation of culture-change practices. Culture change requires dedicated leadership over a period of years, a stable workforce, the buy-in of nursing, and funds for environmental improvements (Koren, 2010). Koren (2010) concluded that “With a policy environment conducive to innovation, and supportive of both initial and sustained adoption of new models, it is possible that—before the baby-boom generation needs long-term care—nursing homes will have become a better value proposition” (p3). The culture-change movement has shown that provision of high-quality nursing home care, individualized to meet each resident’s needs in a setting that maximizes self-determination and well-being, can be a vision made real—with person-centered care as the central focus.
In Closing: Making Recommendations for Quality Care
What this literature review establishes is that there is nothing clear-cut about demonstrating scientific evidence for complicated, individualized, psychosocial interventions such as person-centered care. Overall, the research has limitations including sample sizes, varied interventions within person-centered care models and finally, a paucity of funding and incentives for psychosocial research. Most certainly, more research is needed to continue to understand how to effectively measure person-centered care, what elements are required to make a difference and how does all of this translate into everyday care delivery practices.
However, when examining person centered care through the combined aspects of available evidence (mostly in residential communities), current best practices, expert opinion and common decency, it becomes clear that providing care based on knowing the person within the context of an interpersonal relationship in a way that supports individualized choice and dignity is difficult to argue against. While the evidence in support of person-centered care models and interventions may not be wholly conclusive, there is sufficient evidence to support the following recommendations.
Practice Recommendations for Person-Centered Care
- Know the person living with dementia.
The individual living with dementia is more than a diagnosis. It is important to know the unique and complete person, including his/her values, beliefs, interests, abilities, likes and dislikes—both past and present. This information should inform every interaction and experience. - Recognize and accept the person’s reality.
It is important to see the world from the perspective of the individual living with dementia. Doing so recognizes behavior as a form of communication, thereby promoting effective and empathetic communication that validates feelings and connects with the individual in his/her reality. - Identify and support ongoing opportunities for meaningful engagement.
Every experience and interaction can be seen as an opportunity for engagement. Engagement should be meaningful to, and purposeful for, the individual living with dementia. It should support interests and preferences, allow for choice and success, and recognize that even when the dementia is most severe, the person can experience joy, comfort, and meaning in life. - Build and nurture authentic, caring relationships.
Persons living with dementia should be part of relationships that treat them with dignity and respect, and where their individuality is always supported. This type of caring relationship is about being present and concentrating on the interaction, rather than the task. It is about “doing with” rather than “doing for,” as part of a supportive and mutually beneficial relationship. - Create and maintain a supportive community for individuals, families, and staff.
A supportive community allows for comfort and creates opportunities for success. It is a community that values each person and respects individual differences, celebrates accomplishments and occasions, and provides access to and opportunities for autonomy, engagement, and shared experiences. - Evaluate care practices regularly and make appropriate changes.
Several tools are available to assess person-centered care practices for people living with dementia. It is important to regularly evaluate practices and models, share findings, and make changes to interactions, programs, and practices as needed.

hen, S. (2022). Addressing behaviours of concern: The interplay of health, communication limitation, and psychosocial factors. The Singapore Family Physician, 48(6), 26-33.
Introduction
Persons with intellectual disability (ID) commonly present with behavioural issues, and various terms have been used to describe these behaviours. These include “problem behaviours”, “difficult behaviours”, and in more recent times, “challenging behaviours” and “behaviours of concern”. Jeffrey Chan et al advocated the adoption of the latter phrase “behaviours of concern” to describe these behavioural issues in order to reduce the perception that these behaviours are inherent as problems or challenges in persons with ID, but rather to emphasise the importance of responding to these behaviours with understanding and support. For the purposes of this article, we will therefore refer to these behavioural issues as “behaviours of concern” (BOC).
There have been several definitions for BOC but one that is commonly quoted describes BOC as “culturally abnormal behaviour(s) of such an intensity, frequency or duration that the physical safety of the person or others is likely to be placed in serious jeopardy, or behaviour which is likely to seriously limit use of, or result in the person being denied access to, ordinary community facilities’’. These BOC can include agitation, aggression, self-injurious behaviours, stereotypical behaviours, and/or behaviours directed towards objects. Though widely recognised as being common, the exact prevalence of BOC in persons with ID has been difficult to estimate accurately due to inconsistent definitions and study methodology over the years, with studies reporting rates ranging from 5.7 percent to 17 percent. One particular challenge clinicians encounter is the difficulty in differentiating a BOC unrelated to a psychiatric disorder from behaviours that are atypical presentations of a mental health disorder. The diagnosis is also complicated by the prevalent use of psychotropics in managing BOC, with 14-30 percent of persons with ID presenting with BOC reported to be receiving these medications even in the absence of a diagnosed psychiatric disorder. This occurs partially because the presentation of BOC is often determined by a number of complex factors, including organic conditions, psychiatric disorders, psychosocial and environmental influences, or a combination of all of these, making diagnoses challenging. As a result, a comprehensive and thorough assessment of the possible causes of the BOC is a critical first step and may require input not only from various healthcare providers but also from both formal and informal caregivers. This is important as the impact of BOC is significant not only for the individuals but also for their caregivers and families.
Therefore, it is crucial to obtain detailed histories from the caregivers and families, to ensure that their ability to cope with the behaviours can be assessed concurrently. It has been well reported that there are significantly higher levels of caregiver stress, reduced caregiver satisfaction, reduced self-efficacy, and increased institutionalisation risk when individuals have BOC. Therefore, it is imperative that BOC be addressed in a timely manner so as to reduce caregiver stress and improve the quality of lives of persons with ID and their families. Consequently, the interventions required to address these BOCs also often need to be multidisciplinary and should cover medical, psychiatric, psychological, social, and environmental issues.
In this article, we will outline an approach to assessing BOC and highlight the health, communication, and psychosocial-environmental issues that may contribute to it. Finally, we will briefly discuss the management principles including the usage of psychotropics.
Causes of and assessment of behaviours of concern
The primary objective of assessing BOC in persons with ID should be to not regard the behaviour as a problem but to strive to identify and address the underlying causes of or reasons for the behaviour. Health as defined by the World Health Organisation (WHO) is “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’’.
Putting this definition of health alongside the definition of BOC, it is clear that the presence of BOC impacts the quality of life of persons with ID negatively and does not signify positive health or well-being. Consequently, if BOC are regarded as signs that the health status of the individual is not optimal, it is reasonable that the role of healthcare providers will be to ascertain the underlying cause of this health issue and institute interventions and treatment accordingly.
Bearing this in mind, the biopsychosocial (BPS) framework commonly used in healthcare can be used to assess the BOC the person with ID is presenting with (refer to Figure 1 for the BPS model). Using the BPS model and placing the BOC right in the centre of the diagram, we can see that there could be a number of interrelated reasons for a BOC.
These would include:
- Biological
- A physical health problem, e.g., constipation
- A mental health problem, e.g., depression
- An oral health problem, e.g., dental cavities
- Psychological
- Beliefs, attitudes, and values
- Self-esteem and motivation
- Coping and social skills
- Social
- Family dynamics
- Social relationships
- Work and recreational circumstances
It is important to highlight at this juncture that BOC in persons with ID are also closely intertwined with the cognitive and communication limitations encountered by these individuals.
All individuals with ID experience life in a distinct manner compared to the general population, and moreover, due to the heterogeneity of this population group, each individual also experiences life differently from another. For example, an individual with mild ID working in a supermarket and active in the community will experience life very differently from a person with severe ID who may be non-verbal and mostly homebound, but yet be able to engage meaningfully with his/her family and caregivers. The presentation of BOC in these two distinct groups will also naturally be different.
Using the BPS as a guide, and bearing in mind the cognitive and communication challenges faced by persons with ID, it is evident that BOC are often multifactorial in their causes. For example, a person with ID who is non-verbal but able to vocalise may shout repeatedly when experiencing physical discomfort or pain. This pain could stem from constipation, reflux, a toothache, or even from disturbing hallucinations. Although initially predominantly related to physical or mental health problems, the inability of the individual to express this pain and/or discomfort adequately to caregivers and healthcare professionals could lead to increased anxiety and distress, which could consequently increase the intensity and persistence of the shouting. The frustration and helplessness experienced by the caregivers due to their inability to understand the cause of the shouting could result in even higher levels of stress and escalating anxiety on their part, which would inadvertently lead to reduced caregiver capacity, which in turn could translate to poorer care and increased discomfort resulting in even more agitation in the individual affected. This is a vicious cycle.
The above example illustrates how biological causes can present with a BOC, and the importance of evaluating for and treating these before the condition and circumstances worsen and a vicious cycle ensues. However, once biological causes are ruled out, the next step will be to ask if the BOC being assessed is related to psychological causes.
For example, an individual suffering from grief and confusion from losing a beloved long-time caregiver could present with frequent night awakening and/or restlessness. A person with mild ID might be able to express these emotions verbally to healthcare professionals but individuals with more severe ID might neither be able to process these feelings nor express them in a manner that others understand. As a result, these emotions could be very easily overlooked, and the resulting behaviour manifestation misunderstood. Another example encountered fairly frequently would be in evaluating why an individual is resistive towards certain activities, such as performing specific tasks at an individual’s sheltered workshop. This could be due to a multitude of reasons, including but not exclusive to boredom with or dislike of the task on hand or because he/she is not keen to sit near a particular participant.
As can be seen in the above examples, psychological issues are often closely related to social situations, and these should be examined hand-in-hand with psychological factors.
It is important to understand the individual’s family circumstances and social networks, as well as the daily activities the individual partakes in his/her daily life. These could pertain to their routines at home, or that in their day centre or workplace. Complaints of wandering behaviour could be a result of a reluctance to return to a negative home environment. Conversely, a refusal to let caregivers out of their sight could occur as a result of anxiety due to a fear of abandonment and loss. Particularly for persons with more severe disability, who are highly or fully dependent on their caregivers to be sensitive to and attend to their every need, the social and physical environment becomes critical. Simple things like inappropriate bath water temperature could lead to discomfort, or overstimulating or noisy environments could lead to distress for persons with ID with sensory processing disorders, and manifest as agitation and aggression.
A common point highlighted by all the examples above is that a thorough and holistic assessment with the aid of the BPS framework is an absolute prerequisite in managing any BOC.
As part of the assessment, clear documentation of the BOC is important and should include the following steps:
- A list of the target BOC to be managed, which includes a precise description of the BOC
- The frequency and severity of the BC
- An assessment of the possible causes (using the BPS framework) giving rise to the BOC 4. An evaluation of the triggers and outcomes of the BOC
A simple method of keeping track of point (4) would be to use the ABC recording method. This is a simple way of collecting information about behaviours.
Antecedents (A): what happened directly before the behaviour occurred
Behaviour (B): the specific behaviour of interest
Consequences (C): what happened directly after the behaviour occurred
It is important when using the ABC chart to focus on descriptions of ABC, rather than indicate any interpretations. Refer to Figure 2 below for an example of an ABC chart.
| ABC Chart | ||||
|---|---|---|---|---|
| Name: | ||||
| Date | Time | Antecedent What specific activity or event occured before the behaviour? |
Behavior What specifically did the person do or say? |
Consequence What happened after or as a result of the behaviour? |
| XX | XX | Not getting food he wanted | Head banging against the wall | Giving him the food he wants |
Encouraging caregivers to note down the behaviours in the ABC chart can help tremendously in undercovering the reasons for the behaviours. A clear pattern may emerge, for example, demonstrating that the BOC occur predominantly during meal times, which will give further clues with regards to the possible causes.
However, one important point to highlight at this juncture is that it is not always possible to find a cause for every BOC. If indeed a cause cannot be found after all effort has been made to consider the various possibilities, including allowing a period of observation and actively consulting formal and informal caregivers, then the strategy employed should be to minimise the impact of the behaviour on the individual and the people around him/her, as well as on his/ her environment.
In the next section, some potential health issues that may occur in persons with ID and present with BOC, as well as some pitfalls in making diagnoses, will be shared.
Health Conditions
In addition to being mindful of the presence of health conditions common to the general population, it will also be important for healthcare professionals to bear in mind that certain groups of individuals with ID have the propensity to develop specific health conditions, and to keep a lookout for them when assessing BOC. Refer to Table 1 for some of these examples:
| Syndrome | Common Health Conditions |
|---|---|
| Down Syndrome | Thyroid disease, early onset dementia, obesity, obstructive sleep apnoea, oral health issues, visual impairment, eczema |
| Tuberous sclerosis | Seizures, benign tumours in various organs, e.g., eye, heart, lung, kidney |
| Angelman Syndrome | Seizures, sleep issues |
| Cornelia de Lange syndrome | Cardiac defects, increased risk of respiratory infections, hearing problems |
| Williams syndrome | Chronic ear infections, hearing loss, hypothyroidism, diabetes mellitus |
| Lowe syndrome | Visual impairment, kidney abnormalities, seizures, increased risk of fractures, degenerative bone disease |
Table 1. Common health conditions in individuals with specific syndromes.
Other than these specific health conditions, it is also well recognised that there are certain behavioural phenotypes associated with specific syndromes. These refer to observable characteristics that occur more often in individuals with specific genetic syndromes than in individuals without that syndrome. It will also be helpful for healthcare providers to be aware of these. Refer to Table 2 for some of these examples.
| Syndrome | Behaviour Phenotype |
|---|---|
| Down Syndrome | Positive in mood, distractable |
| Fragile X | Gaze avoidance, hand biting, tics |
| Tuberous sclerosis | Obsessive-compulsive behaviour, repetitive behaviours, nonverbal and autistic behaviours |
| Angelman Syndrome | Head-banging, hand biting, picking at skin, sores, nails, pulling off fingernails and toenails, explosive outbursts tantrums, destructive and aggressive behaviour, excitability, arm hugging/ hand squeezing, reduced sensitivity to heat/pain |
| Prader Willi | Hyperphagia, hyperactivity |
| Lesch-Nyhan Syndrome | Self-injurious behaviour |
| Cornelia de Lange Syndrome | Self-injurious behaviour particularly directed to the hands |
| Williams Syndrome | Reduces fear of strangers and excessive friendless towards other |
Table 2. Behavioural phenotypes in individuals with specific syndromes.
These specific health conditions and behaviour phenotypes are important to note for healthcare professionals, but clinicians must first and foremost remember that not all individuals with specific syndromes show all the possible health conditions or behaviour phenotypes. These merely serve as a guide. Another common pitfall is that of “diagnostic overshadowing”, which refers to the phenomenon in which behavioural or emotional difficulties seen in people with ID are attributed to the ID itself. An example would be the caregiver of an adult with Down Syndrome complaining that he/she is requiring more prompting in doing his/her activities, and the healthcare professional consulted viewing this as part of his/her ID when this might be the initial presentation of early onset Alzheimer’s disease dementia or a frontal lobe tumour impairing motivation.
Other associated phenomena seen in persons with ID that can make it more challenging during assessments include “psychosocial masking”, which refers to an individual’s limited social experiences impacting on their ability to give a clear history of their symptoms or “baseline exaggeration”, which refers to how increasing severity or intensity of symptoms could be viewed as part of the individual’s inherent challenges with adaptive functioning. Healthcare professionals need to be aware of these potential pitfalls and be intentionally mindful and reflective in practice when assessing persons with ID. Many of these phenomena affect how persons with ID communicate their symptoms and emotions to the people around them, and this brings us to the next section, which will highlight some of the communication challenges they face.
Communication Limitations
Communication is an essential life skill, and in the general population, occurs through the five key modalities of listening, watching, speaking, reading, and writing. However, persons with ID face difficulties with all these different aspects of communication and these challenges have been well recognised as contributing significantly to many of the BOC they present with. Between milder to more severe levels of ID is a spectrum of communication profiles. Those with mild ID are likely to communicate with speech, but their ability to understand abstract concepts, their use of vocabulary, and their ability to read and write may be limited. Individuals with moderate ID often also communicate verbally, but these may be in the form of short phrases or single words, which may go hand-inhand with other forms of communication methods such as using sign language. Those with severe to profound ID may not be able to communicate using speech at all and may rely on their caregivers to interpret their body language, vocalisations, or facial expressions. Moreover, it is common for persons with ID, in particular those with more severe levels of ID, to have sensory impairments such as visual and hearing impairment, which will understandably pose further communication difficulties.
With all these barriers to the usual methods of communication, it is evident that persons with ID will have to find alternative methods to communicate their needs and their wants. Behaviours therefore often becomes a mode that is employed. Simply put, behaviours can often be used as a means of communication. For example, a person who is nonverbal and has no other means to communicate may scream and hit out when they are in pain or in distress because they have no other way of conveying their pain to the people around them. Similarly, he/she may also use behaviour such as pushing or spitting to communicate his/ her likes or dislikes with regards to other people or food, simply because they have no other means to communicate.
The critical role communication plays in BOC is supported by a number of studies that report BOC being more common in those with more severe ID, as the increasing difficulties with communication add additional challenges and complexities to expression of needs, wishes, and desires. When a BOC is used as a form of communication, the principle underpinning the management of such a behaviour will be to replace the functional but inappropriate behaviour with one that is more appropriate. This could involve using an alternative method of communication, such as using pictures or teaching the person with ID to express their frustration in a different manner.
In addition to having difficulties expressing themselves, an important point that cannot be overemphasised about communication is that it is a two-way process. The difficulties persons with ID face with communication also make it harder for the individuals to understand information that is conveyed to them, which may consequently lead to inappropriate responses presenting as a BOC. In order to reduce the possibilities of such BOC in persons with ID, it is important that information is communicated clearly to them in a manner they comprehend, and all attempts must be made to get their consent or assent. For example, when performing venepuncture or even checking the blood pressure for a person with ID, it is important that the intent and steps are explained clearly to them, so that their cooperation and agreement can be sought. Resources such as pictures, videos, and easy-read formats can be used to help in the explanation. Easy-read materials refer to the presentation of text in an accessible, clear, and easy to understand format. Refer to Figure 3 for an example of an easy-read material.
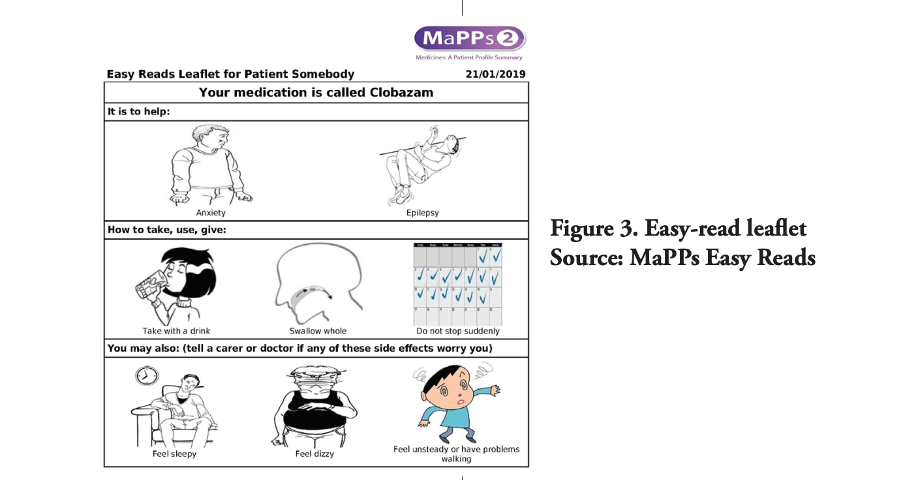
Overall, it is key that attempts be made by healthcare professionals to understand the communication profiles of the individuals with ID who present to them. Effort must also be undertaken to convey information to them in a manner that they understand. All of these will need to be carried out in a supportive environment, which brings us to the next section.
Psycho-Social-Environmental Factors
Research on the social networks of the general population suggests that those who have friends and diverse networks tend to have better outcomes for their health, mental health, and well-being. Studies however show that persons with ID have smaller social networks and less interpersonal relationships compared to people who do not have ID. Furthermore, it is interesting to note that when asked, persons with ID state that support staff make up 43 percent of their social networks, fellow centre participants with ID made up 25 percent, family members 14 percent, and others 11 percent.
This tells us that the composition of their social networks are distinct from that of the general population, and also the critical roles that support staff and families play in the lives of persons with ID. This becomes even more pertinent as persons with ID and their caregivers age, resulting in caregivers passing on before their adult child. When that happens, the persons with ID inevitably start relying even more heavily on support staff. This, however, is a precarious situation, as support staff may regularly change, which will be significant and disruptive for persons with ID due to their already small social networks. The important roles family and support staff play in providing emotional support and in engaging the individuals in activities can be expected to lead to BOC if there are disruptions in these important relationships.
The number of social relationships persons with ID have has also been shown to relate to their level of ID, with more severely disabled individuals having smaller networks. This makes the situation even more challenging, as persons with more severe levels of ID are already known to have higher risk of BOC and greater care needs, as well as their caregivers having higher levels of stress. Moreover, with fewer interpersonal relationships and a higher risk of their social network breaking down, it makes them even more susceptible to suffering the ill effects of psycho-emotional-social losses. These may manifest as new BOC or worsening of existing behaviours. In essence, the families of persons with ID are crucial in providing physical, emotional, and social support to them.
However, the impact of lifelong caregiving on the health, social, and financial well-being of caregivers of persons with ID cannot be overemphasised. As roles and responsibilities change over the course of life, many parents of persons with ID eventually face dual or even triple responsibilities of caregiving. They care not only for their adult child with ID, but also for their own ageing parents, and/or ailing spouse. This is termed compound caregiving. With increasing life expectancy in both the person with ID and his/her caregiver, the ageing caregiver ends up having to care for his/her adult ID child who is also starting to develop his/her health issues as they age. This is an extremely challenging situation.
Consider this example: An adult with moderate ID in his 40s who was previously able to manage his basic activities of daily living himself, but now suffers from declining mobility and recurrent falls, will start requiring more physical care from his father. However, his ageing father would be struggling with his own deteriorating health and may have difficulties providing increased physical care for his adult son. Assisting his son during bath times or during transfers could be challenging, resulting in further near falls during these episodes. Due to the fear, anxiety, and uncertainty that relate around these care episodes, the individual with ID could become resistive to his father’s attempts to care-give, and may express this by pushing him away or even hitting him. His father could then end up more frustrated and even more insistent, which worsens the tension and stress. A vicious cycle could ensue with increased resistive behaviour and agitation, and ultimately, result in institutionalisation.
As the above example illustrates, it is therefore of vital importance to institute the appropriate interventions for BOC as soon as possible in order to break the vicious cycle. The next section will give a brief outline on the approach to management.
Pharmacological and Non-Pharmacological Management of Behaviours
After a comprehensive assessment, if there is an obvious physical or psychiatric cause for the BOC, this should be managed appropriately and promptly, with regular monitoring of the interventions, any potential adverse effects, and the effectiveness of the treatment plan.
However, if no distinct or treatable physical or psychiatric disorder is found, then non-pharmacological management should be considered and employed first. These management strategies should aim to address the psychosocial or environmental issues faced by the individuals that might be contributing to the BOC. For example, if the behaviour is potentially emerging out of boredom, attempts to engage the person more meaningfully will be required. If the assessment suggests that there is an environmental issue that may be contributing to the BOC, for example, excessively warm or cold temperatures in their activity centre, adjustments should be made if practical as far as possible. After interventions have been implemented, a period of observation needs to ensue, to monitor and review the effectiveness of these non-pharmacological treatments, as they often take time. Attempts to address psycho-emotional needs of persons with intellectual disability through counselling where appropriate should also be actively carried out.
Sometimes, after giving a sufficient duration of trial of nonpharmacological management, medication may be needed either on its own or as an adjunct to non-pharmacological based management. The usage of medications in these circumstances may be viewed as an interim strategy, sometimes to allow time for the non-pharmacological interventions to work. It is important to remember that the lack of adequate caregiver support for the use of nonpharmacological management should not be the only reason for using medication, although in practice this may happen due to high and severe levels of caregiver stress, leading to imminent care breakdown. Under such circumstances, the patient needs to be reviewed closely and medication should be used for as short a period as possible. Other resources such as respite care may also need to be organised to support the caregiver and the family in coping with the high behavioural care needs of the person with ID.
Listed below are some of the situations under which the clinicians may consider using medication:
- To treat an underlying mental health disorder
- Failure of non-pharmacological interventions
- Significant risk/evidence of harm/distress to self, others, or property
- To calm the person to enable implementation of nonpharmacological interventions
- Risk of care or placement breakdown
When used, medications should always be prescribed at the lowest possible dose and for the shortest possible duration. The reduction or withdrawal of medication and additional implementation of non-pharmacological strategies should always be considered at regular intervals.
The effectiveness and possible adverse effects of all the interventions should be monitored at regular intervals, which will include collecting subjective and objective information from the persons with ID themselves, their family members, formal and informal caregivers, and from members of the medical team caring for the patient. Physical examination and relevant investigations such as blood investigations and electrocardiograms should also be performed when necessary.
Overall, the choice and decision as to which pharmacological and/or non-pharmacological interventions should be implemented and prioritised will depend on each individual and family’s unique circumstances. Ultimately, the approach needs to be person-centred, which refers to a “process of continual listening, and learning; focused on what is important to someone now, and for the future; and acting upon this in alliance with their family and friends.’’48 The person-centred approach demands that the person with ID be placed right in the centre of any plan, and to consider first and foremost his/her values, priorities, and wishes.
With these in mind, the interventions are then formulated to facilitate the achievement of these goals and aspirations, if appropriate. Not only is the person-centred approach crucial, caregiver and family support are critical and cannot be overemphasised. Lifelong caregiving is already beset with numerous health, psycho-emotional, and financial challenges, what more when family relationships and quality of life is impacted and threatened by stressful and sometimes disruptive BOC. As such, the needs of the caregivers must be addressed and catered to, so as to support and sustain them in their caregiving role. Studies have shown that meaning and fulfilment can be derived from caregiving and can even bring about better mental health outcomes and positive wellbeing, as well as greater life satisfaction in the caregivers themselves. Therefore, with proper support, the relationships and mutual interdependence between the person with ID and his/her caregiver can be enhanced, with persons with ID providing caregiving and companionship in turn to their ageing parents.
This person-centred and family-centric approach strives not only to focus centrally on the needs of the individuals and their caregivers but also requires that the management plan be communicated clearly to the person with ID, their families, and all other relevant professionals involved in his/ her care. This helps to ensure that all parties are aligned and in agreement with the goals that have been set. It will also allow for timely feedback in monitoring for adverse effects and efficacy.
Once a management plan has been initiated, a clear timeline for review should be set. If the improvement of the BOC is unsatisfactory at the point of review, an attempt should be made to re-assess and review the diagnosis and management plan. At any point along the way, if there are concerns or if challenges with the diagnosis and/or management persist, a referral to a psychiatrist should be considered.
Conclusion
Persons with ID commonly present to healthcare professionals with BOC, which often result from a combination of complex factors. These include physical and mental health conditions, as well as psycho-emotional and social-environmental difficulties, and are made more challenging by their inherent cognitive and communication difficulties.
Health as defined by the World Health Organisation (WHO) is “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.’’ Bearing this is mind, the presence of BOC can be regarded as a sign that health and wellbeing are not at their optimum for the person with ID, and the BPS framework can be used by healthcare professionals to guide the comprehensive assessment of BOC in persons with ID. Specific health conditions, the communication profiles of the individuals, and the psycho-emotional and social circumstances surrounding the individual and his/her family need to be considered carefully.
Depending on the underlying cause(s) ascertained, pharmacological and/or non-pharmacological treatment will have to be implemented promptly and appropriately in a person-centred manner, taking into consideration the individual’s wishes and needs. As BOC not only have a significant impact on the quality of life of the individuals with ID, but also on the lives of their caregivers, it is essential to engage and support caregivers actively from the onset. Their wellbeing relates directly to their caregiving capacity, and consequently also contributes significantly to determining the outcomes of the interventions implemented. Interventions for the individual with ID therefore cannot be carried out in isolation without the close support of his/her families.
The overall management plan must be communicated clearly to the person with ID, his/her family, and all other relevant professionals involved in his/her care. Regular monitoring and review of the effectiveness of the interventions will need to be carried out, with reassessments and adjustments of management conducted in a timely manner.
Ultimately, if healthcare professionals can successfully identify the underlying causes of BOC and address the issues appropriately, this will improve the quality of life of many individuals with ID and their families.

