Kia ora, nau mai hoki mai, welcome to week 19 of study! This week, we will jump back into our exploration of Te Tiriti o Waitangi (and the implications of it for the pharmaceutical industry), as well as continue with compliance packaging, and delve into the health condition, arthritis.
Working ethically and professionally
Last week, we discussed the concepts of equity and health inequities. We investigated the history of two important documents; He Whakaputanga (Declaration of Independence) and Te Tiriti o Waitangi (The Treaty of Waitangi).
To help you retain and reinforce your knowledge, let’s start this lesson by circling back to check and update your knowledge from last week. As you will remember, you created a list of what you already knew about Te Tiriti o Waitangi and what you wanted to know/ questions you had about the Treaty and posted it to your journal.
The list may have looked something like this:
Te Tiriti o Waitangi |
|
|---|---|
|
What I currently know Facts, ideas, things I have read, learnt, experienced, my understandings |
What I would like to know Gaps in my knowledge or understanding, what I wonder about, what I want to know more about |
Find and re-read your list now. Have your questions been answered? Perhaps our last session made you think about other things you want to know. Take a few minutes now to update your journal post by answering any questions you had or writing any new questions/ thoughts/ comments that have arisen.
Note:
If you haven’t already, it’s a good idea to add your journal post permalinks to your Index of Journal Posts document so you can find these easily. You can download and save this template.
The Principles of Te Tiriti o Waitangi
As we know, the differences in translations between the Māori and the English versions of the Treaty have created much controversy and confusion. One of the roles of the Waitangi Tribunal is to act as the:
exclusive authority to determine the meaning and effect of the Treaty. It can decide on issues raised by the differences between the Māori and English texts of the Treaty.Waitangi Tribunal 2023
This means that we now have a way to better understand the intentions and meaning of the Treaty. You may also recall from your level 3 study that the meaning of the Treaty can also be understood from the viewpoint of the underlying three principles. These were referred to as the 3Ps.
They are:
- Protection
- Participation
- Partnership
However, in the 2019 Hauora Report from the Waitangi Tribunal inquiry, the tribunal stated that the 3Ps are not an accurate reflection of Te Tiriti o Waitangi and its principles. Instead, the tribunal recommended the incorporation of the following five principles into the primary health care system:
- Tino rangatiratanga (Māori self-determination)
- Equity
- Active protection
- Options
- Partnership
This and other recommendations from the 2019 Hauora Report were included in the health reforms in 2022 when our country moved to a new national health system.
Activity
health reforms
- Read this short passage on the health reforms (and watch the 3-minute video).
- Apply this new learning! Use the information from the webpage to fill in the blanks in the sentences below.
- Follow this link to download and save this 2-page document from the Ministry of Health - “Our Te Tiriti o Waitangi framework”. The document outlines how the principles and articles of Te Tiriti o Waitangi are being applied in health.
- Take some time to read and understand this document. We encourage you to make your own notes. To support your learning, you may like to copy and paste the te reo words into Te Aka (the online Māori dictionary) to hear the correct pronunciation. You can listen to the words and then say them aloud to yourself.
By following the tribunal’s recommendations and focusing on how best to provide health services to Māori, the government can work towards meeting their obligations under Te Tiriti o Waitangi and provide a more equitable health care system.
Applying the principles to practice
As a pharmacy technician, there are many ways you can provide pharmacy technician services to Māori in accordance with Te Tiriti o Waitangi principles.
Click on each of the (+) symbols or the five Treaty principles to read examples of what this might look like in the workplace.
Respect the autonomy and choices of Māori patients regarding their healthcare. This includes discussing treatment options and involving them and their whānau in decision-making processes.
- Ensure that all patients, regardless of their ethnic background, have equal access to pharmacy services.
- Be proactive in identifying and addressing health disparities by providing extra support, information and resources to patients who may face barriers to healthcare access.
- Ensure patients are aware of and can access any subsidised pharmacy services they are eligible for.
- Understanding and protecting the Māori culture, language, and worldview, including the use of Rongoā Māori.
- Be aware of and understand the different Māori models of health, customary practices, and Māori philosophy.
- Be aware of and respect the importance of including whānau in supporting the health and well-being of the individual patient.
- Actively advocate for Māori patients' health needs and rights within the healthcare system, ensuring they receive equitable care.
- Continuously educate yourself and colleagues on the unique health challenges faced by Māori communities and the steps needed to address them.
- Offer Māori patients culturally sensitive treatment options that align with their beliefs and values.
- Understand and support the use of Rongoā Māori.
- Be aware of and refer patients to kaupapa Māori health services when appropriate, recognising their cultural significance.
- Provide advice and information to support informed decision-making.
- Collaborate with Māori patients and their whānau in decision-making and care planning.
- Take time to get to know patients and build trusting relationships.
- Actively listen and respond to the Māori patient’s needs.
- Create a physical and emotional environment for clear, open communication.
- Engage with local Māori communities and health organisations to foster a sense of partnership and mutual support.
Working with Māori patients
The Pharmacy Council Statement on Cultural Competence (2011) and Competence Standards for the Pharmacy Profession (2015) both provide helpful guidance for pharmacy technicians for working with Māori patients. You will be familiar with these documents from your previous learning. Now is a good time to revisit these documents and think about how you can apply them to your day-to-day work with Māori patients.
Let’s refresh your knowledge now with the two documents:
| The Pharmacy Council Statement on Cultural Competence (2011) | The Pharmacy Council and Competence Standards for the Pharmacy Profession (2015) |
|---|---|
|
|
Journal activity:
Applying the principles to practice
- Read pages 12- 15 of the Competency Standards for the Pharmacy Profession (2015).
- Focus on the behaviours described that you could apply to your practice.
- In your journal, note down:
- one behaviour that you think you already do well in your practice.
- one behaviour that you think you would like to improve, and what steps you might take to do this.
Watch: Kina Kina (1:31 minutes)
Before we move on, let’s take a BRAIN BREAK! This short break involves engaging both your mind and body in a different activity. It's a moment to pause, recharge, and prepare to continue your learning journey. We encourage you to participate even if you feel a little silly.
So, e tū (stand up) and press play to begin!
We hope you gave the brain break a go and had a little fun. It might seem silly, but it’s proven that taking little breaks throughout your study increases your focus and retention. Ka pai, let’s get back into the mahi!
Meeting the needs of Māori
Now let’s look at this article by Kiwi pharmacist Deborah Bassett-Clarke, who discusses meeting the needs of Māori in pharmacy practice. Although the article is quite long, it has many valuable insights, so we recommend grabbing a cuppa and taking the time to read it.
The article starts with comments on the Treaty and equity and has a brief overview of the results from her own cross-cultural study on attitudes and perceptions to medicine taking. Deborah then goes on to discuss barriers to medicine taking for Māori and Māori concepts and how they relate to health outcomes.
These concepts are:
- Whakapapa
- Whanaungatanga
- Manaakitanga
- Mauri
- Mana
- Tapu
Note:
To hear how these words are correctly pronounced, go to the online Māori dictionary Te Aka. You can also read further definitions of the concepts to strengthen your understanding.
Rongoā Māori
As mentioned earlier in this session (and in the article above), understanding and supporting Rongoā Māori is a way that pharmacy staff can adhere to the principles of Te Tiriti o Waitangi. If you’d like an explanation of Rongoā Māori, read this great article - Demystifying Rongoā Māori: Traditional Māori Healing.
Forum activity
Rongōa Māori
Do you or your family use Rongoā Māori or other traditional cultural healing methods? Perhaps your family follows unique practices to promote health and well-being that are unrelated to culture or religion?
- In the class forum, Week 19 – Professional Practice: Rongōa Māori, share a short description of any traditional or family-based health and healing practices that you’re aware of and feel comfortable sharing.
- Respond briefly to at least one peer’s post, sharing your thoughts or asking a follow-up question.
- Reflect on what you’ve learned from the diverse practices shared in the forum. Ask yourself what new insights you have gained.
By sharing our experiences, we can broaden our awareness of the diversity of health and well-being practices in our communities. Please approach this activity with respect and an open mind, as you may encounter practices different from yours.
Hauora Māori
| Earlier, you looked at The Pharmacy Council and Competence Standards. You read about the expected behaviours for meeting competency M1.5 – ‘Understand Hauora Māori’, as shown here. |  PCNZ (2015) pg.12 |
Hauora is the Māori view of health and well-being. (Click here for the pronunciation). Now, let’s dig a bit deeper into what hauora Māori means in terms of understanding Māori perspectives of health.
Watch – Overview of Te Whare Tapa Whā (1:08 minutes)
You may be familiar with the Te Whare Tapa Whā model of health that describes hauora and wellbeing as a wharenui (meeting house). Sir Mason Durie developed this model in 1984 to encourage people to develop well-being.
Watch this video from the Ministry of Health (MOH) as he gives an overview of his model:
Now that you have a general overview, deepen your understanding of each aspect or domain of Te Whare Tapa Whā.
Click on each of the labels/ elements in the graphic below to watch six short videos explaining each aspect. You can also navigate by using the arrows at the bottom of the activity.
Other Māori health models
Te Whare Tapa Whā is not the only Māori model of health. You can read about the Te Wheke (Octopus) model and the Te Pae Mahutonga (Southern Cross Star Constellation) model here on the Ministry of Health website.
Self-directed learning activities
It's time to consolidate your learning and insights from this session and apply them to this week’s three SDL tasks. This week, you can fire up your creative flair as much as you want!
Activity 1
- Illustrate how a pharmacy technician can incorporate the principles of Te Tiriti o Waitangi into the services they provide. You can create a brainstorm (see the example below), draw a picture or write bullet points.
- Consider working with a classmate on this activity. You'll be amazed by the multitude of ideas that can surface through collaborative learning!
- Share your thoughts or image of your brainstorm to the forum – Week 19 – Professional Practice: Self-directed Learning Activities. (Save your work to an easily accessible location on your device, too.)
- Have a look at your classmates’ responses and respond to at least one example that you find interesting and would like to incorporate into your own practices as a pharmacy technician. The beauty of shared learning is that you may pick up some ideas and methods you hadn’t thought of. Knowledge shared is knowledge multiplied!
The brainstorm image below is an example of how you may wish to make your own. You can replace the placeholder 'idea' bullet points with your own examples.
Activity 2
Watch: Fill My Whare Tapa Whā (3:30 minutes)
Attending to your own well-being is an important step in being prepared and ready to take on the challenges of assisting others with their health and well-being. Here is an activity for you to do for your own hauora.
- Watch this video and then fill your own Whare Tapa Whā as demonstrated.
- Keep your own Whare Tapa Whā somewhere visible (on your computer desktop or physically taped to the wall in your bedroom) so that it becomes part of your daily life. Having a balanced well-being is a continual journey of small steps – use your poster as a kete of well-being ideas to draw from when needed.
Activity 3
Now that you have completed your online learning on Te Tiriti o Waitangi, it’s time to pause and reflect on your current knowledge and what gaps (if any) you might still have.
- Find your journal post from last week (Week 18 – Professional Practice), with the list of ‘what I currently know’ and ‘what I would like to know’. You can use your Index of Journal Posts to find the permalink.
- Reflect on your learning up to this point and consider:
- What new knowledge can you add to ‘what I currently know’?
- Has your ‘what I would like to know’ list been answered? If not, how can you answer the remaining questions? (For example, by talking to your peers and tutor or by conducting your own research.)
- Do you have any more questions that you would like to add?
- Consider what steps you can take to keep your learning going and to continue developing your understanding and skills in providing pharmacy technician services to Māori in accordance with Te Tiriti o Waitangi principles.
We have now come to the end of week 19, and our topic of working ethically and professionally. Kia pai mai hoki! That’s fantastic!

Fakaalofa atu, hello and welcome back. In our last session, we discussed the features, benefits and limitations of the following types of compliance packaging:
- Hard packs/ pill organisers
- Sachet packaging
- Blister/ Medico paks
We also looked at the assembling of compliance packaging, with a focus on:
- hygiene and environment
- general process – the steps from receiving through to collection of a compliance packaged prescription.
This week, we will continue our exploration of compliance packaging.
Considerations for compliance packaging
Medications are often packaged in specific containers and materials that help maintain their stability, including protection from light, moisture, and temperature fluctuations. When preparing packaging, you will remove medicine from stock bottles and other original packaging, such as foil sheets. Drug manufacturers cannot guarantee the stability of medicines once they are removed from their original packaging; therefore, you need to be aware of the properties of different medications and their special considerations when preparing compliance packaging.
The properties of medicine to consider are their temperature sensitivity, photosensitivity, hygroscopic and deliquescent properties.
Read the descriptions for these properties and then complete the following activity to find examples for each.
| Temperature Sensitive Substances | Many medications are recommended to be stored at controlled room temperature, typically between 20°C to 25°C. This environment ensures that most drugs maintain their potency and effectiveness throughout their shelf life. However, it's important to note that certain medicines may require lower temperatures, around 2-8°C, and therefore should be stored in a refrigerator. Additionally, it's important to avoid subjecting medications to extreme temperature variations, as this can impact their quality and efficacy. |
|---|---|
| Photosensitive Substances | A substance that can become activated or cause adverse reactions when exposed to light, particularly sunlight or certain types of artificial light. These drugs contain molecules that can absorb light energy and undergo chemical reactions, leading to various effects, which can be therapeutic or harmful. |
| Hygroscopic Substances | A substance that strongly attracts moisture or water vapour in the air. When exposed to even low levels of humidity, hygroscopic substances tend to absorb water molecules from the surrounding environment but do not change their physical state. |
| Deliquescent Substances | A substance that absorbs water vapour in the air but can also absorb so much water that it dissolves in the absorbed moisture, forming a solution. This changes the substance's physical state from a solid to a liquid. |
Special consideration
The following are examples of three medications that require special consideration when dispensing for compliance packaging.
Click on each label or the (+) symbol to read more.
Sodium valproate is a commonly used antiepileptic medication. It is unstable in the presence of moisture due to its hygroscopic and deliquescent nature. The picture shows changes in the tablets stored under various temperature and humidity conditions. One of the changes was a change in the weight of the medicine. This can impact the accuracy of the dose. Accurate dosing is critical for medications used in conditions like epilepsy, where effectiveness and consistency are vital. There was also a change in the dissolution profile of the tablets (changes in how the tablets dissolve in the body). Variations in dissolution can affect the rate and extent of drug absorption, potentially impacting its effectiveness.
![[ADD IMAGE'S ALT TEXT]](/sites/default/files/Sodium%20Valproate.png)
Dispensing:
The recommendation for sodium valproate is to dispense it in its original foil by cutting around the tablet before placing it in the compliance pack and/ or dispensing it in a 7-day pack. Pack this drug last and then seal the compliance pack immediately in low humidity conditions. Ensure the backing is sealed tightly to the tray to prevent moisture from getting in.
Furosemide is a medication commonly used in the treatment of cardiac failure and hypertension and is often repacked into compliance packaging. It is a photosensitive drug. The picture below shows the results of a ‘home environment” where the compliance packaging was stored blister-side up in a bathroom. The pack was exposed to a standard 60W tungsten bulb and indoor indirect daylight through a window.
![[ADD IMAGE'S ALT TEXT]](/sites/default/files/Frusemide%20Tables.png)
As a result of the way the pack was stored, the colour of the tablets changed, and there was a potential breakdown in the medicine’s chemical structure, which can lead to reduced effectiveness of the medication. It can also shorten the shelf life of the tablets.
Storage:
It is recommended that furosemide is stored at or below 25°C and is protected from light.
Chlorambucil is a medicine in tablet form that is used in the treatment of some types of cancer and some types of kidney conditions.
Storage:
Store tablets in the fridge. Do not freeze. Therefore, these tablets will need to be in their own compliance packaging that the patient keeps in their fridge at home.
Self-directed learning activities
Activity 1:
- Read this webpage from Medsafe about medicine storage and repackaging.
- Create a journal post titled ‘Medicine Storage’ and answer the following questions:
- What group of medicines does Pradaxa belong to, and what is it typically prescribed for?
- What occurred to a patient as a result of repackaging Pradaxa into their weekly pill box?
- What occurred once the patient stopped repackaging their Pradaxa and kept them in their original container?
- What is a ‘desiccant’?
- Save the permalink for the journal post to your Index of Journal Posts.
As a pharmacy technician, you will need to find out the considerations and recommendations on how to package specific medications for compliance packaging. You can source this information by referring to the individual drug data sheets on the Medsafe website.
Activity 2:
- Read this Australian journal article on the appropriate use of dose administration aids.
- Create a journal post titled, ‘Dose Administration Aids’ and answer the following questions:
- What practical aids and strategies should be considered before dose administration aids are implemented?
- In what patient situations are dose administration aids effective, and when are they not effective?
- The article notes that regular medicine reconciliation is a way to avoid problems with dose administration aids. What do you think is meant by ‘medicine reconciliation’?
- When may medicines not be suitable for repacking into a dose administration aid?
- Save the permalink for the journal post to your Index of Journal Posts.
You have now completed week 19. Kei runga noa atu! - Outstanding! Great work.

Mālō e lava mai, welcome to Week 19 of Patient Care. Throughout level 3 and level 4 of this programme we have explored many different health conditions. In this session, we continue to develop and build on your knowledge of health conditions by focusing on arthritis.
Arthritis isn't a single disease; instead, it includes a range of disorders that affect joints and their surrounding tissues. We will focus on the following three types that you may already have some knowledge and experience of.
These types are:
- Gout (Mate waikawa kai kōiwi)
- Osteoarthritis (Pona ngoikore)
- Rheumatoid arthritis (Mate rumatiki)
Understanding arthritis is crucial for pharmacy technicians, as it's a condition that many individuals encounter. This knowledge will empower you to better assist and support your pharmacy patients in managing arthritis, ultimately contributing to their well-being and quality of life.
Gout (Mate waikawa kai kōiwi)
| In this medical illustration, you can see gout affecting the joint at the base of the big toe. | 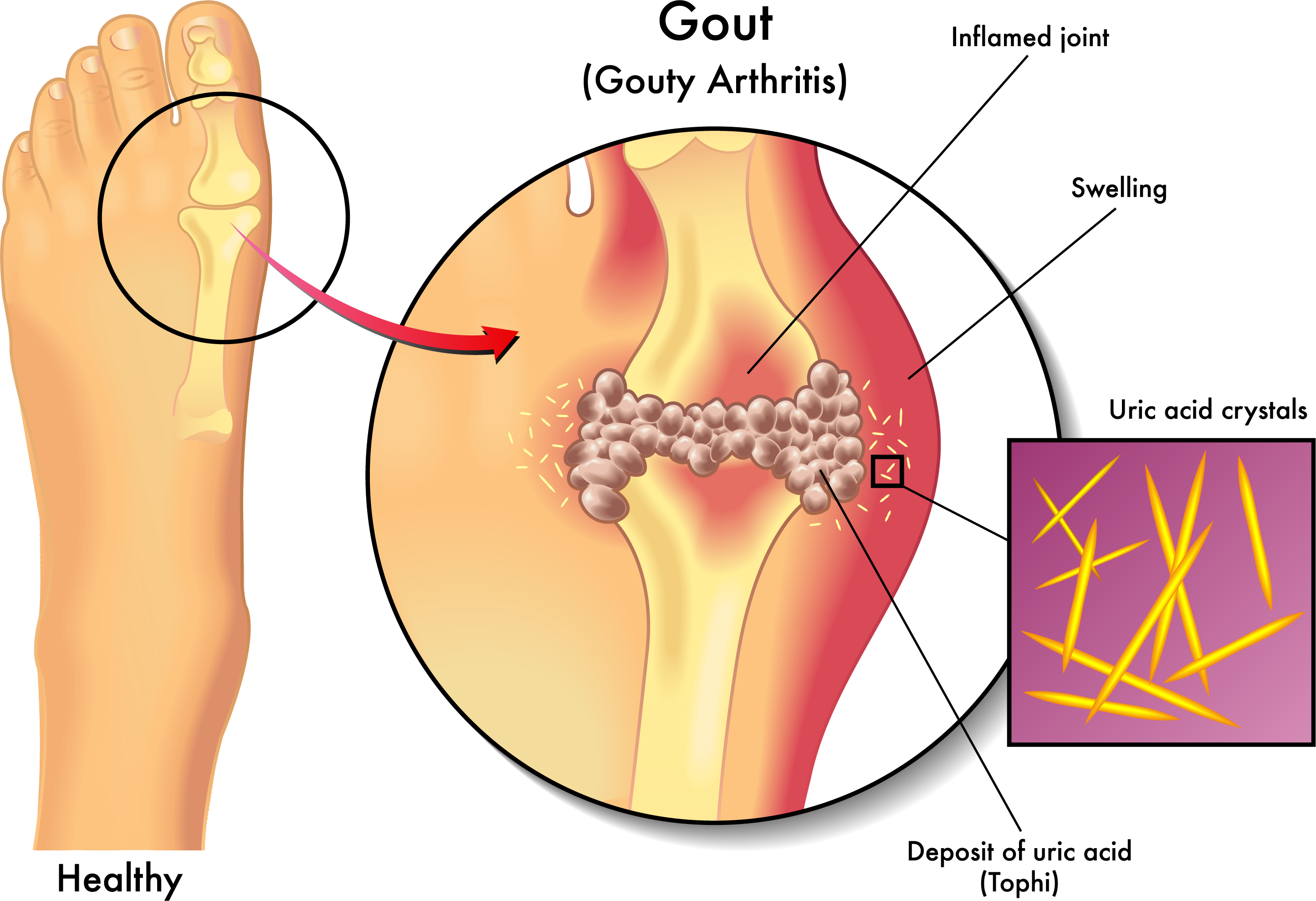 |
Watch: Gout: Visual Explanation for Students (2:22 minutes)
Watch this video for a simple overview of what gout is, including the risk factors for developing this condition and how to manage it. You might like to take your own notes as you watch. After you have viewed the video, answer the following four questions.
Journal post
health conditions: gout
For the following learning activity on the treatment of gout, you may like to use these reliable sources of information as well as any you find yourself:
- New Zealand Medicine Formulary (NZMF): Musculoskeletal and joint diseases page
- Healthify website: Health A-Z tab and Medicines A-Z tab
- Ministry of Health website: Conditions and treatments page
- Arthritis NZ: Mateponapona Aotearoa
- Pharmacy Today Health Care Handbook: Hard copies on campus
- Create a journal post titled ‘Health Conditions: Gout’ and answer the following questions:
- For what population in Aotearoa New Zealand, is gout more common and more severe?
- As a pharmacy technician, if you encounter a customer with gout-like symptoms or who wants pain relief for gout symptoms, what should you do?
- Is gout an acute, chronic, or other type of condition?
- How is gout prevented?
- Give a brief overview of lifestyle and self-care strategies.
- Name any preventative medicines and briefly describe how they work in the body.
- How is gout treated?
- Give a brief overview of lifestyle and self-care strategies.
- Name any preventative medicines and briefly describe how they work in the body.
- Save the permalink for the journal post to your Index of Journal Posts.
Rheumatoid Arthritis (RA) and Osteoarthritis (OA)
| RA and OA are both types of arthritis. In this illustration, you can compare a healthy joint to one that has been affected by OA and RA. | 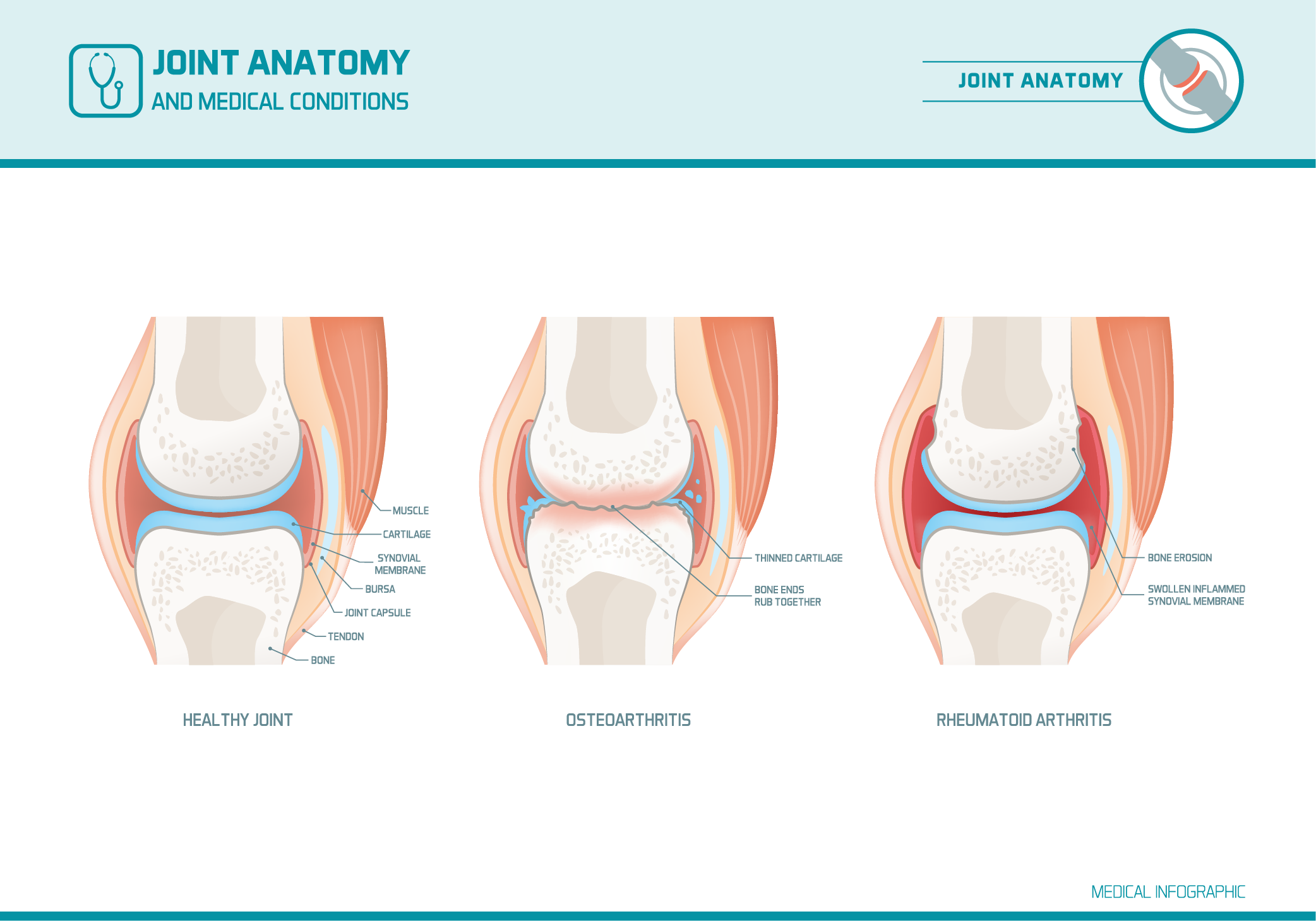 |
Watch: Osteoarthritis vs rheumatoid arthritis symptoms (8:52 minutes)
Watch this video for an explanation and comparison of the causes, signs, and symptoms of these conditions. We encourage you to take notes as you go and to pause the video when you need a moment to absorb the information.
Check your understanding and answer the following seven questions.
How did you get on? If there were any answers that you got stuck on, make sure to note down the correct answer in your notes to help your learning.
Forum activity
OA & RA Graphic resource
In this tūmahi (activity), you are going to get a little bit creative! Once again, you may like to use the same reliable resources that you used for your activity on gout. These were:
- New Zealand Medicine Formulary (NZMF): Musculoskeletal and joint diseases page
- Healthify website: Health A-Z tab and Medicines A-Z tab
- Ministry of Health website: Conditions and treatments page
- Arthritis NZ: Mateponapona Aotearoa
- Pharmacy Today Health Care Handbook: Hard copies on campus
This learning activity allows you to get your creative juices flowing! Remember, the more effort you put into activities now, the larger your portfolio of learning materials and resources grows!
- Create a one to two-page graphic resource for pharmacy customers about osteoarthritis and rheumatoid arthritis. The graphic should be A4 in size and a combination of text and pictures. It may be in any format you wish, for example, handcrafted, or digital using Word, PowerPoint, or any other application you have available.
- The graphic must contain the following information for each condition:
- The cause of the condition
- The population most likely to be affected by the condition
- The typical signs and symptoms
- The typical medicines used to treat the condition- the dose form, route of administration and a brief explanation of how the medication acts in the body.
- Preventative measures (as applicable) and self-care/non-pharmaceutical treatments
- Upload an image of your completed graphic to the class forum - Week 19 – Introduction to Patient Care: OA & RA Graphic Resource. If you have handcrafted your graphic, take a photo and upload it.
- Check out the work that your peers share and take note of any information that is new to you.
- Save your work somewhere easily accessible on your computer – you may want to refer to it later in your studies.
Great work building up your own portfolio of resources! And, to finish your studies this week, we, of course, have your SDL.
Self-directed learning activity
This week, we’d like you to extend your learning on different types of arthritis.
- Visit the Arthritis NZ webpage and investigate the other forms of arthritis listed.
- Choose ONE type of arthritis that we have not already explored.
- Create a journal post titled, ‘Health Conditions: Types of Arthritis’ and include the following in your notes:
- The type of arthritis/ condition that you have chosen
- The cause/s
- Typical signs and symptoms
- Typical medicines used in the treatment of the condition
- Prevention and self-care strategies
- Save the permalink for the journal post to your Index of Journal Posts.
- Review the conditions that your classmates have made notes on. This is a great way to learn from each other.
You have come to the end of another week and the end of this module. Ka mutu pea - you are doing awesome! Please complete the Learning Check-in quiz to move onto Module 7.
