In this section you will learn to:
- Implement personal hygiene practices in the work setting.
- Practice hand hygiene in accordance with national standards and guidelines.
- Follow current national standards and guidelines for selection and correct use of Personal Protection Equipment (PPE) as required.
- Follow procedures for environmental cleaning and management of waste.
- Identify and respond to situations where transmission-based precautions or enhanced cleaning is required.
- Follow processes for management of spills and exposure to blood or body fluids
Supplementary materials relevant to this section:
- Reading C: Disinfection and Sterilisation in Health Care Facilities
- Reading D: Infection and Prevention and Control in Allied Health Practice
In the previous section of this module, you were given a path of frameworks and guidelines that will assist you in your duty and care as a helping professional. We now move further into the setting of organisational structure and professional practice in the industry.

Hand hygiene is a clear focus in the Allied Health field. Following the practices highlighted in this Study Guide means that you are using professional practice in your role as a helping professional within the community. Hygiene is not only about hand washing; it is the fundamental of infection prevention and control. Now let’s look at personal hygiene where many diseases and conditions can be prevented or controlled through regularly washing parts of the body and hair with soap and water.
Nail hygiene

Appropriate hand hygiene includes diligently cleaning and trimming fingernails, which may harbor dirt and germs and can contribute to the spread of some infections.
To help prevent the spread of germs and nail infections:
- Keep nails short and trim them often.
- Scrub the underside of nails with soap and water (or a nail brush) every time you wash your hands.
- Avoid biting or chewing nails.
- Avoid cutting cuticles, as they act as barriers to prevent infection.
- Never rip or bite a hangnail. Instead, clip it with a clean, sanitised nail trimmer.
- Do not wear nail polish, particularly as chipped nail polish may support the growth of organisms on the fingernail.
Facial cleanliness

Facial cleanliness is important to your health. Use soap and clean, running water to remove dirt, oil, and unwanted debris from your face.
Protect yourself by:
- Washing your hands at keys times (such as before touching your face or putting in contact lenses)
- Using a tissue for your nose
- Using a tissue to scratch or rub your eyes or to adjust your glasses
- Preventing itchiness by using facial moisturiser for dry skin and eye drops for dry eyes
Respiratory etiquette

You will always be around patients that would have the common cold and cough symptoms. It is wise that a clinic has a display of the ideal respiratory etiquette for both patients and the HCWs to be aware of. Respiratory etiquette refers to practices that reduce the potential for transmission of diseases from coughing and sneezing and includes:
- covering the mouth and nose when coughing and sneezing
- using tissues to contain secretions, and disposing of tissues after use in bin provided, if you do not have a tissue, cough or sneeze int your elbow, not your hands. Always remember to throw used tissues in the trash.
- attending to hand hygiene with soap and using water and disposable towels to dry hands, or using an alcohol-based hand rub.
It is useful and appropriate to have posters prominently displayed in patient and staff areas relating to respiratory etiquette. This becomes essential in pandemics.
Remember to immediately wash your hands after blowing your nose, coughing or sneezing. Washing your hands is one of the most effective ways to prevent yourself and your loved ones from getting sick, especially at key times when you are likely to get and spread germs.
- Wash your hands with soap and water for at least 20 seconds.
- If soap and water are not readily available, use an alcohol-based hand sanitizer that contains at least 60% alcohol to clean hands.
To help prevent the spread of respiratory disease, you can also avoid close contact with people who are sick. If you are ill, you should try to distance yourself from others, so you do not spread your germs. Distancing includes staying home from work or school when possible.
Find out more
Health care workers will always have to assist patients that need assistance with containment of respiratory secretions. Take a look at section 3.2.3 of the Australian Guidelines for the Prevention and Control of Infection in Healthcare for more information.
Working uniforms and clothing

Linen and clothing used in health care facilities are disinfected during laundering and generally rendered free of vegetative pathogens (hygienically clean), but they are not sterile. Hygienically clean linen is suitable for neonatal intensive care units.
Healthcare workers should wear a clean uniform for each shift. Uniforms should be washed at home, separately from other items. A typical washing cycle consists of three main phases, i.e., pre-wash, main wash, and rinse cycle. For used and infected linen, the washing process should have a disinfection cycle in which the temperature in the load is maintained at 65 ° C for not less than 10 min or, preferably, at 71 ° C for not less than 3 min. Additional time is recommended to allow mixing and heat penetration.
At the end of the day, it’s vital that uniforms and scrubs are adequately cleaned. If employees buy their own uniforms or clean them at home, there is a risk it is not done correctly. In allied health, uniforms will vary depending on where you work. In some settings, uniforms might be colour coded to indicate the role or department each HCW is placed in. In other settings, such as private practice, the dress code for allied health professionals may be more flexible. However, they might still be required to follow certain guidelines, such as wearing professional attire.
Remember you would still be required to follow the policies and procedures for uniform laundering/dress code put into place by the healthcare facility you are employed at. However, the basic procedures to align with are as follows:
- Staff might be required to wear their usual clothes if using public transport to travel to and from work and then put on uniforms once at work.
- There would be a dress code policy in place which might mention that uniforms need to be changed daily.
- Always wash the attire you have worn following a shift, this can be washed as usual, using normal laundry detergent using hot water to ensure complete removal of bacteria and other infectious agents.
- Staff can choose to dry their clothing in the sun or use a tumble dryer.
- Lastly. follow the instructions on the care label attached to the uniform to determine the appropriate water temperature, washing cycle, and drying instructions.
Reflect
Take a look at Section 5.3 p. 233 in the following document - Education in practice – hand hygiene where you will see focus on the National Hand Hygiene Initiative.
Make notes on your findings on the basis of this question of ‘why is it an important initiative and how it could be used in the Allied Health field?’

Standard precautions are the primary strategy for minimising the transmission of healthcare-associated infections. Standard precautions must be used when providing care to all patients, regardless of whether they have an infection or not. Standard precautions involve:
- hand hygiene, as consistent with the 5 moments for hand hygiene
- the use of appropriate personal protective equipment
- the safe use and disposal of sharps
- routine environmental cleaning
- reprocessing of reusable medical equipment and instruments
- respiratory hygiene and cough etiquette
- Aseptic technique
- waste management
- appropriate handling of linen
In certain situations, the use of standard precautions alone may not be enough to limit the spread of infection. When this occurs, transmission-based precautions are required. There are three types of transmission-based precautions: contact, droplet, and airborne precautions. One or more types of transmission-based precautions may be required, depending on how an infection is spread between people. A local risk assessment should always be undertaken to determine the most appropriate requirements to maintain patient and staff safety. Let’s take a look at the basic yet general aspect of hand hygiene.
Jewellery and wrist watches
As a health administrator, you might enjoy dressing up to work and that includes wearing jewellery which can affect hand hygiene. The skin under rings may be more heavily colonised than comparable skin without rings and rings can interfere with hand-hygiene techniques. Hence, jewellery should be kept to a minimum when at work.
Although there is less evidence concerning the impact of jewelry on the effectiveness of hand hygiene, rings can interfere with the technique used to perform hand hygiene resulting in higher total bacterial counts. Hand contamination with infectious agents is increased with ring wearing, although no studies have related this practice to healthcare worker-to patient transmission. The consensus recommendation is to strongly discourage the wearing of watches, rings or other jewelry during health care; however, if jewelry must be worn in clinical areas it should be limited to a plain band (e.g. wedding ring) and this should be moved about on the finger during hand hygiene practices. In high-risk settings such as operating suites/rooms, any jewelry, even a plain band, should not be worn.
(Australian Government, 2019)
Intact skin
Your skin is a natural defence against infection, cuts and abrasions. Breaks or lesions of the skin are possible sources of entry for infectious agents and may also be a source of them. Similarly, the presence of fingernail disease may reduce the efficacy of hand hygiene and result in the transmission of pathogens. To reduce the risk of cross-transmission of infectious agents, cuts and abrasions should be cleaned with a good antiseptic and covered with waterproof dressings.
Reflect
Take a look at Section 5.4 p. 234 Here you will see the Case study for the prevention of needlestick injury.
Make notes on your findings with the reflective question of ‘why is it important to consider needlestick injury in your work role in the Allied Health industry?’
The Australian Commission on Safety and Quality in Health Care established the National Hand Hygiene Initiative (NHHI) in 2008 as part of a suite of initiatives to prevent and reduce healthcare-associated infections in Australian healthcare settings. The National Safety and Quality Health Services (NSQHS) Standards require health service organisations to have a hand hygiene program consistent with the NHHI and jurisdictional requirements.
The NHHI uses a multimodal approach to improving hand hygiene. Implementation of the NHHI is led by states, territories, and health service organisations (public and private), and includes:
- The use alcohol-based hand rub at the point-of-care
- Ensuring uniform hand hygiene and infection prevention and control education
- Monitoring hand hygiene compliance and performance feedback
- Using hand hygiene programs that ensure culture change
Effective hand hygiene is essential for infection prevention and control and patient and healthcare worker safety.
As a helping professional, you will constantly be interacting with patients, those who are both unwell and well; therefore, hand hygiene is a core strategy in the prevention of health care associated infections. Hand hygiene has a dual role in that it protects both patients and healthcare workers from acquiring microorganisms which may cause them harm, and it results in a significant reduction in the carriage of potential pathogens on the hands. This can be readily achieved by using liquid soap and water with an effective technique, or by using an alcohol hand rub or gel on visibly clean hands.
Microorganisms on hands
Resident organisms can be found on the skin’s surface, which is deep-seated in the epidermis (the outer layer of the skin) and cannot be easily removed by a single hand washing procedure. Transient organisms colonise in the superficial layers of the skin and are microbes that are impermanent and stay on the skin for short periods of time. It is often acquired by the HCWs during direct contact with patients or by contaminated environmental surfaces. These microorganisms usually survive only for a limited period of time and are easily removed by hand washing or use of alcoholic hand rub on physically clean hands.
Find out more
Hand washing is not just a basic fundamental value to follow in health care, it is quite comprehensive. If you are interested to understand the concept of handwashing in detail read through this document: National Hand Hygiene Initiative | Australian Commission on Safety and Quality in Health Care
Hand hygiene products

Now that you understand the two different kinds of microbes that might live on our hands, let’s take a look at the products we need to use for efficient hand washing. Hand washing refers to the application of soap (plain or antimicrobial) and water on the hands. Despite the fact that plain soap has minimal antimicrobial activity, it can be used for routine hand washing (WHO, 2009).
- Water - although water is considered the ‘universal solvent’, water alone is not suitable for cleaning dirty hands. Despite common belief, water temperature does not appear to be a critical factor for removal of microorganisms from hands being washed. However, use of very hot water for hand washing should be avoided as it increases skin irritation and may cause damage. After hand washing, thorough rinsing and drying is necessary.
- Soap - plain, neutral pH soap can be used for routine hand washing. Added substances, (including antimicrobial agents) should be avoided as they have no added benefit and may cause allergies, irritation, or dryness of the skin. If a bar of soap is used, then the bar should be small in size to allow frequent changing since all HCWs might be using the same bar of soap, causing it to be exposed to other. In order to avoid contamination with microorganisms, it should be kept dry (in a soap rack or on a magnet or ring) to promote drainage of water. Liquid soap should be stored in closed containers and the dispensers should be regularly cleaned. If liquid soap is dispensed from reusable containers, these must be cleaned when empty and dried before refilling with fresh soap to avoid microbial contamination. Special attention should be taken to clean pump mechanisms as these have been implicated as sources of cross-infection.
- Antiseptic preparations - preparations containing antiseptics such as iodine solution or chlorhexidine are usually used to clean the skin after an injury before a surgery or before an injection.
- Hand drying - ideally, hands should be dried using individual good quality paper towels. Reusing or sharing of cloth/fabric towels must be avoided in health care facilities as they are recognised as a source of cross-infection. If cloth/fabric towels are used, then they must be single-use and sent to the laundry. When towels (paper or fabric) are used to dry hands, it is important to pat the skin rather than rub it, to avoid cracking of skin.
- Nailbrushes - routine use of nailbrushes is not recommended because they damage the skin, encouraging the proliferation and persistence of microorganisms on the skin.
Hand hygiene technique
Alcohol-based hand rub
Alcohol-based hand rubs have become popular due to the recent global pandemic COVID-19. The use of alcohol hand rubs has now become the ‘gold standard’ for routine hand decontamination, and they should be used routinely when hands are not visibly soiled (i.e., most of the time). The rapid efficacy of alcohol-based solutions and their availability at the patient’s bedside and point of use have made these products an ideal substitute for conventional hand washing, addressing the real and perceived constraints associated with hand washing, and substantially increasing hand hygiene compliance rates. They remove microorganisms more effectively, take less time to apply and are less likely to lead to skin irritation.
The hygienic hand rub method is convenient and useful especially in areas where a hand-wash basin is not readily available:
- Emergency situations where there may be insufficient time and/or hand washing facilities.
- When hand washing facilities are inadequate.
- In the community or when return to a hand-wash basin is impractical.
- During a ward round where, there is a need for rapid hand disinfection.
Precautions for skin reactions

Frequent and repeated use of soaps and other detergents are responsible for chronic dermatitis among HCWs, and this can be reduced by the addition of humectants, for example, ingredient(s) added to hand hygiene products to moisturise the skin. In addition, skin irritation is also found due to the presence of antimicrobial agents and other ingredients present in the soaps of the formulation.
Two major types of skin reactions are associated with hand hygiene:
- Irritant contact dermatitis - is extremely common and is caused by frequent use of hand hygiene products. This can be reduced by using moisturising skin care products and by avoiding soap and water hand washing before or after an alcohol-based product is used.
- Allergic contact dermatitis - is very rare and is present as delayed type reactions or less commonly as immediate reactions. The most common causes of contact allergies are fragrances and preservatives present in the hand hygiene products. Exposure to irritating soaps and detergents can be minimised by promoting the use of alcohol-based hand rubs containing humectants. These products are well tolerated and are associated with a better skin condition when compared with either plain or antimicrobial soap.
The 5 moments of hand hygiene

The WHO (2009) have simplified the recommended indications to perform hand hygiene into the concept of ‘My Five Moments’. Let us look at how the ‘5 moments’ of hand washing that you can incorporate as a HCW within a clinical setting. You must always remember that, although you will be considered a health administrator, there will be occasions that arise when you would need to assist patients.
| The Five Moments | Examples |
|---|---|
| 1. Before touching a patient |
|
| 2. Before clean/aseptic procedure |
|
| 3. After body fluid exposure risk |
|
| 4. After touching a patient |
|
| 5. After touching patient's surrounding |
|
Reflect
Take a look at Section 5.2 p. 232 Risk Management Case study. Here you will see identifying risks, using a risk management approach, with focus on the 5 moments for hand hygiene. Make notes on your findings with the reflective question of ‘what are my strategies to remember and use the 5 moments for hand hygiene?’

Now that you have an understanding of the main hygiene protocols such as personal and hand hygiene, let’s take a look at personal protective equipment (PPE). The primary aim of using personal protective equipment (PPE) in health care settings is to protect the skin and mucous membranes of HCWs from exposure to blood and/ or body fluid. It also prevents contamination of clothing and reduces the opportunity of spread of microorganisms from patients and/or fomites to other patients, staff, and environments.
Masks

Masks may be used by unimmunised staff when there is a risk of droplet or airborne spread of disease, although it is recommended for all HCWs to wear. Masks may also be worn by patients to prevent the spread of a disease (suspected or known) that is transmissible by droplet or airborne spread. There are two types of masks, the surgical and the N95 respirators. The correct type of mask must be chosen according to the situation.
All masks need to be fluid repellent and disposable. Precautions include:
- Do not touch the front of the mask while being worn.
- Remove and replace the mask if it becomes wet or soiled.
- Do not wear a mask around your neck.
- Do not reapply a mask after it has been removed.
Hand hygiene should be performed upon touching or disposing of a used mask.
P2/N95 masks
P2/N95 masks, also known as respirators or particulate filter masks, are special masks designed to filter out small particle aerosols and large droplets. P2/N95 masks must comply with AS/NZS1716:2012 Respiratory protective devices and need to be fitted correctly to be effective. Wearers need to be appropriately trained in their use. A risk-management approach should be applied to ensure that staff performing high-risk duties are fit tested and aware of how to perform a fit check.
Correct handling of used masks is important to prevent the risk of infection to the staff member and patient. When removing the mask, handle only the elastic or strings. Dispose of the mask into the appropriate waste stream.
Reflect
Let’s take a moment to think about the beginning of COVID-19 when it was at its peak. Try and recall the face mask guidelines. Were there any exceptions to this?
Gloves

Gloves give added protection in situations where heavy contamination occurs and simply washing hands is unlikely to remove the bacteria effectively. As a HCW you need to remember that gloves will not entirely protect you fully and decontamination is still necessary because gloves may get punctured or leak. When wearing gloves, gloves need to be changed:
- after contact with each patient
- in between procedures on the same patient
- if gloves are damaged during a procedure
- on completion of tasks
- before handling notes, telephones.
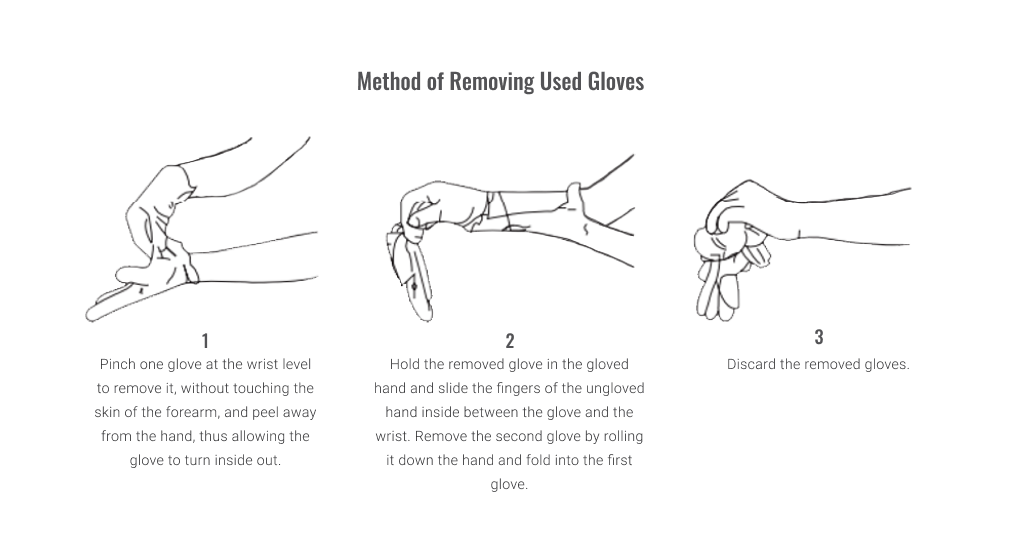
Removing and disposing of gloves
As a health administrator, you might not be required to wear gloves; this really depends on the facility you are employed at. However, understanding the appropriate method of handling used gloves is important to reduce the risk of infection to yourself. Remove gloves inside out and hold by the edge to minimise contamination of hands. Dispose of gloves into the appropriate waste stream as soon as they are removed. Lastly you must perform hand hygiene after removing gloves, as mentioned before gloves DO NOT protect you contamination fully. Take a look at the image below illustrating the appropriate method of removing used gloves.
Protective eyewear and face shields

The aim of protective eyewear (glasses, goggles, or face-shields) is to help guard the mucous membranes of the eyes, nose, and mouth of the HCW from exposure to blood and/or body fluids that may be splashed, sprayed, or splattered into the face during clinical procedures. Protective eyewear must be worn during procedures that are likely to generate droplets or aerosols of blood and/or high-risk body fluids. They should comply with approved standards, must be close fitting, optically clear, anti-fog, distortion free, and shielded at the side.
Face shields may be used to provide additional face and mouth protection. When removing and disposing of goggles:
- Take care to remove using the stems only.
- If disposable, discard into the appropriate waste basket.
- If reusable, wash with soap and water, disinfection with a hospital grade disinfectant can then follow, and dry before reuse.
Correct handling of used goggles/face shields is important in preventing the risk of infection to staff members.
Gowns and aprons

Single-use disposable plastic aprons are recommended for general use and should be worn when there is a risk that clothing or uniforms may become exposed to blood and/or body fluids. Plastic aprons should be worn as single-use items for one procedure or episode of patient care only. Once the task is performed, they must be removed immediately after use by tearing the neck strap and waist tie and gently rolling it inwards to minimise contamination of microorganisms during disposal.
Clean, non-sterile gowns should be worn during procedures which are likely to expose HCWs to spraying or splashing of blood and/or body fluids. Gowns should be impermeable and water repellent or have water-repellent panels in the areas most prone to exposure. If the gown is expected to become wet during the procedure and if a water-repellent gown is not available, a plastic apron should be worn over the gown.
Fitting a protective gown
Put on the gown with the opening at the back and secure the tapes to prevent the gown opening and clothes becoming contaminated.
Removing aprons and gowns
Remove aprons and gowns in a manner that prevents contamination of clothing or skin. Undo tapes and remove the gown inside out, taking care not to touch the outside of the gown. Roll the gown into a bundle and, if disposable, dispose of it into the appropriate waste container. If reusable, place the gown into a designated linen container so it can be washed and dried appropriately before reuse.
Applying and removing PPE

Applying and removing PPE in the correct order is essential to prevent transmission of disease to the staff member. Before putting on PPE, explain to the patient that it is a routine part of infection prevention and control and done for everyone’s safety. Hand hygiene must be performed before putting on PPE and after removing PPE.
Applying PPE
PPE should be applied in the following order:
- Long-sleeved gown, tied up at the back
- Mask
- Goggles
- Gloves, taking care to tuck the cuffs of the gown into the gloves*.
*Gloves must always be put on last.
Removing PPE
PPE needs to be removed in the following order:
- Remove gloves inside out and dispose of into the appropriate waste stream.
- Perform hand hygiene.
- Remove goggles. Place disposable goggles into the appropriate waste stream. Reusable goggles are cleaned and disinfected before reuse.
- Remove gown, taking care not to touch surfaces exposed to contamination.
- Dispose of disposable gown into the appropriate waste stream. Reusable gowns are placed into a linen bag marked ‘contaminated’.
- Remove mask, taking care to handle by the strings only. Dispose of mask into the appropriate waste stream.
- Perform hand hygiene.
|
Sequence for putting on PPE Put on PPE before patient contact and generally before entering the patient room |
|
|---|---|
|
HAND HYGIENE
|
|
|
GOWN
|
|
|
MASK
|
|
|
PROTECTIVE EYEWEAR OR FACE SHIELD
|
|
|
GLOVES
|
|
|
Sequence for removing PPE Remove PPE at doorway or in anteroom |
|
|---|---|
|
GLOVES
|
|
|
HAND HYGIENE
|
|
|
PROTECTIVE EYEWEAR OR FACE SHIELD
|
|
|
GOWN
|
|
|
MASK
|
|
|
HAND HYGIENE
|
|
(Center for Disease Control and Prevention, 2007)
According to Safe Work Australia, 2023:
‘A person conducting a business or undertaking (PCBU) has a primary duty to ensure the health and safety of workers while they are at work in the business or undertaking and others who may be affected by the carrying out of work, such as visitors.’
(Safe Work South Australia, 2023)
The choice of PPE appropriate for the circumstances should be determined by a risk assessment. The Australian Government (2022) has key guidance on the PPE relevant to the Allied Health industry. This is particularly relevant to inform you further on the types and uses of PPE for health workers.
This Wearing Personal Protective Equipment in Allied Health video is an overview of PPE in use as a professional in the Allied Health industry. The video runs for just over 8 minutes but it is well worth watching for picking up the key issues and relevant equipment.

Now that you are aware of the equipment you would need as a HCW and how to use that equipment effectively, let’s take a look at making sure the area we work in or where the patient is staying is clean to the best standards. As you may already know hospitals and clinics are visited daily by patients that may have an infectious disease, hence why WHO recommends a few protocols to follow in order to prevention and control infection.
Disinfection and sterilisation are essential for ensuring that medical and surgical instruments do not transmit infectious pathogens to patients. Because sterilisation of all patient-care items is not necessary, health-care policies must identify, primarily on the basis of the items’ intended use, whether cleaning, disinfection, or sterilisation is indicated.
Sterilisation

It is a process that destroys or eliminates all forms of microbial life and is carried out in health-care facilities by physical or chemical methods. You can implement steam under pressure, dry heat, and liquid chemicals as the principal sterilising agents in your health-care facility. Always bear in mind that these are not limited to and that some clinics may have other chemicals to sterilise equipment and areas around the health facility.
Disinfection

This is a process that eliminates many or all pathogenic microorganisms, except bacterial spores, on inanimate objects. In health-care settings, objects usually are disinfected by liquid chemicals or wet pasteurisation. Each of the various factors that affect the efficacy of disinfection can nullify or limit the efficacy of the process.
Cleaning

The cleaning policy in your healthcare facility should identify each HCWs responsibilities, work health and safety issues, procedures for routine scheduled cleaning, unscheduled cleaning and monitoring of effectiveness. A risk analysis would determine the methods, frequency and thoroughness of cleaning and the products used.
Specific cleaning requirements will vary for each practice. However, all practices need a cleaning policy that includes both:
- Routine and scheduled cleaning of all surfaces and equipment to reduce dust and dirt which can harbour microorganisms
- Unscheduled cleaning for blood, body fluid and other spills.
Environmental cleaning
The room and its items/equipment should be cleaned according to local cleaning procedures. Hot water and detergent are sufficient for most purposes, however ‘hand-touch’ surfaces and patient care items/equipment must be cleaned and disinfected using appropriate disinfection on a daily basis to reduce the bioburden of microorganisms. All baths and shower facilities and associated equipment must be decontaminated after each patient use. The methods and frequency for these processes, and the products used should be according to local policy. Staff employed for these purposes should receive specific training in the relevant aspects of infection control, which includes issues for specific areas such as isolation rooms.
Spillage of blood and body fluids should be disinfected and cleaned promptly using a safe method. Appropriate personal protective clothing should be worn, and waste should be discarded as clinical waste. When the patient is discharged from an isolation room, the room must be thoroughly cleaned. Single-use items must be discarded, and other items/equipment must be decontaminated as per local policy. Items which require high-level disinfection/ sterilisation must be sent to the sterile supply department for sterilisation. After cleaning, once the room is dry, it can be occupied by the next patient.
Equipment cleaning
You must use a designate area for processing all instruments and equipment for reuse. It is essential to establish a workflow pattern systematically moving from ‘dirty to clean’ within the designated area. A one-way workflow will ensure that dirty reusable medical devices do not come into contact with clean reusable medical devices.
Ideally, as a health administrator, you must remember that hand hygiene should be performed in the following instances:
- When moving from dirty to clean areas
- After handling soiled equipment
- Before handling or packaging clean equipment.
In the case where you have been asked to handle contaminated reusable medical devices make sure you have the appropriate gloves (e.g., utility or puncture resistant, heavy duty) to wear. If you come across none, request for an order to be placed for purchasing these through your supervisor.
Sinks
Within a health care facility an equipment processing area needs to have two sinks: one ‘dirty’ sink designated for washing and one ‘clean’ (or cleaner) sink for rinsing washed reusable medical devices. If separate sinks are not available for washing and rinsing then you can use clearly labelled, suitably sized container and inform the other HCWs of the same.
All sinks and any containers used need to be cleaned after use with water and detergent as well as regularly cleaned and dried to reduce contamination. A laundry sink can be considered for disposing off wastewater from cleaning, rinsing linen that had blood and cleaning buckets and mops. The laundry sink is best located in the practice laundry or utility room.
Bench tops
Bench tops should be regularly cleaned and kept clean. If space is restricted, an area can be made temporarily clean by placing a sheet of disposable plastic-backed paper or a suitably labelled tray or container in the area. Packaging of items must take place on a clean, dry surface away from contaminated items. The bench top must be cleaned and dried between uses.
Enhanced cleaning
The table below derived from the Australian Guidelines outlines the recommended minimum frequencies for routine cleaning of various items in healthcare facilities. First, as a health care worker you would be required to identify the level of risk of the objects or area:
- Very high risk: outbreak in high-risk areas
- High risk: intensive care unit, high dependency unit, burns unit, renal units, operating suite, emergency department
- Significant risk: general wards
- Low risk: rehabilitation, long-term care, office-based, domiciliary nursing services.
| Element | Very high risk | High risk | Significant risk | Low risk | Method |
|---|---|---|---|---|---|
| Bed |
Clean frame daily |
Clean frame daily Clean underneath weekly Clean whole on discharge |
Clean frame daily Clean underneath weekly Clean whole on discharge |
When visibly soiled & whole on discharge | Detergent Detergent + disinfectant for multi- resistant organism (MRO) |
| Blood pressure cuff | Clean after use | Clean after use | Clean after use | Clean after use | Detergent |
| Carpets | Clean twice daily | Clean daily | Clean daily | Clean weekly | Vacuum with high efficiency particulate air filter |
| Catheter stand/bracket | Clean daily & after use | Clean daily & after use | Clean before initial use, after use & monthly | Clean before initial use, after use & monthly | Detergent |
| Chairs | Clean twice daily | Clean twice daily | Clean daily | Clean weekly | Detergent Detergent + disinfectant for MRO |
| Drips/intravenous stands | Clean contact points after use | Clean contact points after use | Clean contact points after use | Clean contact points after use | Detergent Detergent + disinfectant for MRO |
| Doorknobs/ handles, patient room | Clean twice daily | Clean daily | Clean daily | Clean daily | Detergent Detergent + disinfectant for MRO |
| Mattress | Clean when visibly soiled/ bodily fluids & after discharge | Clean when visibly soiled/ bodily fluids & after discharge | Clean when visibly soiled/ bodily fluids & after discharge | Clean when visibly soiled/ bodily fluids & after discharge | Detergent + disinfectant for MRO Preferable that entire mattress has waterproof cover |
| Medical equipment (e.g., IV infusion pumps, pulse oximeters) | Clean daily | Clean daily | Clean daily | Clean weekly | Detergent Detergent + disinfectant for MRO |
| Nebulisers | Clean daily & after use | Clean daily & after use | Clean monthly & after use & before initial use | Clean bi-monthly & after use & before initial use | Detergent |
| Oxygen equipment | Clean daily & after use | Clean daily & after use | Clean monthly & after discharge & before initial use | Clean monthly & after discharge & before initial use | Detergent |
| Medical gas equipment | Clean daily | Clean daily | Clean daily | Clean daily | Detergent |
| Sharps bin trolley | Clean daily | Clean twice weekly | Clean weekly | Clean monthly | Detergent |
| Surfaces (general horizontal) in patient room | Clean twice daily & spot clean after use | Clean twice daily & spot clean after use | Clean daily & after discharge | Clean weekly & after discharge | Detergent + disinfectant for MRO |
| Wheelchairs | Clean daily and after use | Clean daily and after use | Clean monthly and after use | Clean monthly and after use | Detergent |
Reading C - Disinfection and Sterilisation in Health Care Facilities
Reading C describes the proper use of disinfection and sterilisation processes are presented, based on well-designed studies assessing the efficacy and effectiveness of disinfection and sterilisation.
Managing blood or body fluid spill

You must deal with any spillage of blood and body fluids immediately and remember to always wear gloves and an apron. Here are the steps to managing an exposure to blood or body fluid:
- Decontaminate the exposed area and treat the wound.
- Report the exposure to the infection prevention and control coordinator so that appropriate investigations and treatment are initiated immediately.
- Test the source for Hepatitis C virus and HIV.
- Test the exposed person for HBV, HCV and HIV.
- Assess risk of transmission of infection to the exposed person.
- Initiate treatment according to risk.
- Document exposure to allow investigation of the cause to take place.
- Refer to an infectious diseases consultant if the exposure is high risk.
Subsequently, these are the steps to cleaning body fluid spill:
- Wipe the area immediately with paper towels.
- Clean with warm water and detergent (possibility a hospital-grade disinfectant).
- Rinse and dry the area. Drying should be done properly as wet areas attract contaminants.
- Dispose contaminated waste into either:
- appropriate biohazard containers or bags (always identify the container through the symbol
- general waste container or
- sanitary waste bins
- Wash hands thoroughly with soap and water, dry with paper towels and sanitise hands using an alcohol-based rub or gel.
Remember emergencies are unavoidable, and it is inevitable that accidental exposure to blood or body fluids wills occasionally occur. Routine good practice enables HCWs to cope in these situations, therefore try and have a few hands-on trainings occasionally.
Management of linen

Health care practices should have a policy on the management of linen. HCWs need to be educated about when to change linen, the use of appropriate precautions during handling, and the washing, drying and storage of linen. The following outline will give you a brief overview of how often linen needs to be changed, this can be the bedding or clothing of the patient and yourself as a HCW. Once again, remember that, although you might be a health administrator, the facility you are employed at might require you to perform the following duties in the event of sickness, emergencies, or staff absenteeism.
Frequency
Linen needs to be changed if:
- A patient requires the use of contact precautions, for example, is known or suspected of having scabies or lice
- There has been a blood or body fluid spill on the linen
- The linen is visibly soiled
- The linen has absorbed odour.
Precautions
Practices should:
- Use appropriate PPE as required. If soiled, use gloves, and if dripping with fluid or body substances
- Wear a mask, apron and safety glasses
- Check that sharps or other items are not caught up in linen and never shake linen
- Place used linen into a covered, lined container while awaiting cleaning
- Store used-linen containers away from clean linen, preferably in a ‘dirty’ utility area.
Linen that contains expressible blood or body fluids needs to be collected into a plastic bag before being placed in the used linen receptacle.
The National Safety and Quality Health Service Standards require health service organisations to have processes in place to maintain a clean and hygienic environment, in line with the current edition of the Australian Guidelines for the Prevention and Control of infection in healthcare. The Commission has produced the following suite of environmental cleaning resources to support health service organisations in meeting Action 3.13 of the Preventing and Controlling Infections Standard and implementing the environmental cleaning requirements of the Australian Guidelines for the Prevention and Control of Infection in Healthcare.
Reading D - Infection and Prevention and Control in Allied Health Practice
The intention of Reading D is to provide guidance to support the safe continuation of essential services as required during the current and future pandemics. This reading is taken from a very informative set of guidelines; therefore, a link will be provided in your Book of Readings for this unit, where you can access and read the document at your pleasure.

Now that you are aware of all the cleaning protocols that a HCW must adhere to, let’s take a look at the prevention of microbial contamination by removal, exclusion, or destruction of microorganisms, better known as asepsis.
Notice that the standard precautions are once again the same:
- Hand hygiene
- Aseptic technique
- Use of personal protective equipment (PPE)
- Respiratory hygiene and cough etiquette
- Safe use of sharps
- Environmental cleaning
- Reprocessing of medical equipment
- Appropriate handling of linen and waste management.
Aseptic in different settings
| Settings | Examples |
|---|---|
| Clinic |
|
| Pharmacy |
|
| Laboratory |
|
Essential principles
As a health administrator, it might not come off as a mandatory requirement to understand the following principles; however, it’s best to know what needs to be done prior to a procedure and the aseptic techniques alongside these. These principles are:
1. Sequencing
Sequencing involves a series of actions that ensure each procedure is performed in a safe and appropriate order. Sequencing includes assessing for risks to patient safety and the HCW and identifying strategies to mitigate these risks prior to starting the procedure.
2. Environmental control
There are many factors in the clinical environment which can increase the risk of infection and patient harm during a procedure. Therefore, all HCWs need to make sure the area/environment they are working in, is clean and free of any hazards, risks, and all the equipment are damage and contaminate free.
3. Hand hygiene
There are critical moments before, during and after an invasive procedure or a procedure requiring aseptic technique when hand hygiene should be performed.
4. Maintenance of aseptic fields
The HCW should ensure that the aseptic field, the key parts, and key sites are always protected.
5. Personal Protective Equipment (PPE)
PPE is important for protecting both the patient and HCW during aseptic procedures.
The table below gives you some examples to consider at each principle stage of asepsis:
| Essential Principles | Factors to be considered |
|---|---|
| 1. Sequencing | Perform a risk assessment:
|
| 2. Environmental control |
|
| 3. Hand hygiene |
|
| 4. Maintenance of aseptic fields |
|
| 5. Personal protective equipment (PPE) |
|

You should now be more familiar with all the equipment and cleaning protocols that you as a HCW would need to adhere to. In this section we will look at the most practical approach to clinical waste management. As a HCW you must identify waste that represents a sufficient risk of causing infection during handling and after disposal and for which some precautions are necessary to prevent any significant potential risk of infection.
Disposal of general waste
Firstly, we look at general waste which is any waste that does not fall into the clinical and related waste categories. It includes:
- Office waste
- Kitchen waste
- Urine, faeces, teeth, hair, nails
- Disposable nappies
- Used tongue depressors
- Non-hazardous ‘pharmaceutical’ waste (e.g., out-of-date saline)
- Items contaminated with blood or body substances not to an extent considered clinical waste (for example - not contaminated with expressible blood) – practices need to check their relevant state or territory environment protection agency definition and requirements.
General waste can further be divided into recyclable and non-recyclable material, which you might be aware of when it comes to your own general waste produce at home. Practices should consider their waste segregation and decide on what type of containers are required. Practices may provide receptacles for disposal of:
- Recyclables (e.g., separate waste and confidential waste bins under desk, glass and plastic recyclables bin in the kitchen)
- Waste contaminated with blood or body fluids that is not clinical waste (e.g., for disposing of tongue)
- Depressors, using a small bin mounted on a wall inaccessible to small children
General waste must be disposed into a rigid-walled, puncture resistant container.
Safe handling and disposal of contaminated waste

Remember as a HCW you will come across clinical waste on a daily basis, discarding this waste might take place few times in day depending on the health care facility. This clinical waste must be handled, stored, packaged, labelled and transported appropriately to minimise the potential contact with the waste and to reduce the risk to the environment from accidental release. The following are regarded as clinical waste:
- Discarded sharps
- Human blood, fluids and tissue (excludes teeth, hair, nails, urine and faeces)
- Any waste from patients known to have, or expected of having, an epidemiologically significant
- Communicable disease (e.g., influenza) or are suspected or known to be colonised/infected with an antibiotic resistant organism
- Material that contains free flowing or expressible blood.
Clinical waste containers
Always remember that clinical waste need to be:
- Rigid walled
- Sealable with a secure lid
- Easily handled: ideally, they should have hands-free operation
- Appropriately labelled: yellow in colour, biohazard symbol displayed and be labelled as ‘clinical waste’.
Liquid clinical waste should be absorbed using ‘kitty litter’ or polymerising beads, then bagged to avoid leakage and potential for splash. Sharps containers are a particular type of clinical waste container that need to meet Australian Standards requirements.
Storage of waste
The waste collection might not visit the healthcare facility daily; therefore, you need to be aware that before collection and disposal, clinical and related waste should be appropriately stored as follows:
- The storage area should be dedicated to clinical and related waste storage (no mixing with other stored materials such as supplies).
- The storage area should be appropriately signed.
- Clinical waste needs to be double bagged, with the outer bag being yellow (or purple) to identify the contents for appropriate disposal.
- Bags need to remain within secure outer containers that are appropriately labelled.
- The waste storage area needs to be secure (not accessible to the public).
Disposal of waste
Clinical and related waste must be transported by a licensed transport and disposal company that will take it for appropriate treatment and disposal. The generator of the waste (the practice) is responsible for it until it has been rendered safe. The transport/disposal company may refuse to collect from overflowing, wrongly segregated or unlabelled bins.
It is worthwhile remembering the following clinical and related waste design rules, derived from the Department of Environment and Science.
| Waste | Container | Symbol Colour | Symbol | Identification |
|---|---|---|---|---|
| CLINICAL | Yellow | Black |
Biohazard symbol |
Clinical waste |
| CYTOTOXIC | Purple | White |
Cell in telophase |
Cytotoxic waste Incinerate at 1100oC |
| RADIOACTIVE | Red | Black |
Radioactive symbol |
Radioactive waste |
Responsible person
Your health care practice should nominate a person responsible for waste management. The responsibilities of this person may include:
- Monitoring for appropriate waste disposal (e.g., that waste is being appropriately segregated)
- Being the contact person for waste transport/disposal companies
- Providing task-specific waste management education for staff.
It is always best to remember which state or territory your practice belongs to. Therefore, you can check the relevant state or territory requirements placed by the relevant environmental protection agencies for the management of clinical waste as the related requirements can differ between jurisdictions.
| State or territory | Legislation for waste management |
|---|---|
| Australian Capital Territory | http://www.legislation.act.gov.au/a/1990-5/ |
| New South Wales | http://www.health.nsw.gov.au/environment/clinicalwaste/Pages/default.aspx |
| Northern Territory | https://legislation.nt.gov.au/Legislation/WASTE-MANAGEMENT-AND POLLUTION-CONTROL-ACT-1998 |
| Queensland | https://www.ehp.qld.gov.au/assets/documents/regulation/pr-gl-clinical-and-related-waste.pdf |
| South Australia | http://www.epa.sa.gov.au/community/waste_and_recycling/medical_waste |
| Tasmania | https://www.legislation.tas.gov.au/view/html/inforce/current/sr-2020-015 |
| Victoria | https://www.health.vic.gov.au/sites/default/files/migrated/files/collections/policies-and-guidelines/s/solid-waste-mngmnt-guide---pdf.pdf |
| Western Australia | https://ww2.health.wa.gov.au/~/media/Corp/Documents/Health-for/Public-health-act/Code-of-practice-for-clinical-and-related-waste-management.pdf |
This section of the module outlined the key personal hygiene practices such as care and cleanliness, use of clean clothing and laundering processes, sickness policy at work and respiratory etiquette. You learned the principles of hand hygiene and how it does not revolve around soap and water, but how health care workers need to identify when hand hygiene is required and the correct technique. You were also introduced to the procedure of alcohol-based rub versus soap and water, each having its own purpose. You learned the safe and effective use of personal protective equipment (PPE) such as gloves and apron and the acceptable technique of applying, fitting and removing PPE. Lastly, you were introduced to cleaning procedures and waste management. You learned about cleaning and managing environment and equipment cleaning, body fluid spills and linen. Likewise, you were introduced to how health care workers should dispose general and contaminated waste.
In the next section, we will look at how we can monitor infection prevention and control through management of work processes, infection control measures and hierarchy of control measures. We will also look into organisational policies and procedures for risks and incidents in healthcare facilities.
Australian Government. (2019). Australian guidelines for the prevention and control of infection in health. https://app.magicapp.org/#/guideline/6572
Australian Government. (2022). Guidance on the use of personal protective equipment (PPE) for health care workers in the context of COVID-19. https://www.health.gov.au/resources/publications/guidance-on-the-use-of-personal-protective-equipment-ppe-for-health-care-workers-in-the-context-of-covid-19
Centre for Disease Control and Prevention. (2007). Example of safe donning and removal of personal protective equipment (PPE). https://www.cdc.gov/infectioncontrol/guidelines/isolation/appendix/ppe.html
Houston Methodist. (2020). [Photograph of someone washing their hands under a running tap.] https://www.houstonmethodist.org/blog/articles/2020/mar/hand-washing-why-it-matters/
Maskmedicare Shop. (2021). Medical staff washing hands. [Photograph]. Unsplash. https://unsplash.com/photos/56GvuA8PkyI
Minimalist. (2020). [Photograph of a woman splashing water on her face]. https://beminimalist.co/blogs/skin-care/do-s-and-don-ts-for-washing-your-face-how-often-should-you-wash-your-face
Safe Work South Australia. (2023). Primary duty of Care. https://www.safework.sa.gov.au/workers/primary-duty-of-care#:~:text=The%20PCBU%20has%20a%20primary%20duty%20of%20care,work%20carried%20out%2C%20eg%20visitors%20and%20the%20public.
Siegel, J. D., Rhinehart, E., Jackson, M., & Chiarello, L. (2007). Guidelines for isolation precautions: Preventing transmission of infectious agents in health care settings. Centre for Disease Control and Prevention.
South Australia Health. (2020). Aseptic technique: Staff training, self-assessment and competency workbook. https://www.sahealth.sa.gov.au/wps/wcm/connect/97aa2638-5fe1-469e-8032-090a2dfd2890/AT+workbook+-+combined_v1.0+%28Nov2020%29_FINAL+.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-97aa2638-5fe1-469e-8032-090a2dfd2890-nRi8VFh
Weston, D. (2013). Fundamentals of infection prevention and control: Theory and practice. Wiley Blackwell.
World Health Organisation. (2009). Guidelines on hand hygiene in health care: First global patient safety challenge. Geneva.
