In this section you will learn to:
- Gain access to patient records to facilitate visit
- Check currency and accuracy of patient information
- Create new records according to workplace protocols
- Storing patient records according to workplace policy and procedures
Supplementary materials relevant to this section:
- Reading C: Electronic Administrative Record Keeping Checklist

Before the patient’s arrival for their appointment, you would need to access the patient’s record and information to facilitate their visit. Depending on the specific setting you work in, this can be important information such as:
- Medical history
- Pathology test results
- X-ray scan results
- Updated treatment or care plan
- Previous diagnoses
Having access to this information is important because you could assist the healthcare professional to provide better care for the patient by having a better understanding of the patient’s health situation. They are also able to provide more person-centred care for the patient during their visit, and improve efficiency as they are able to quickly retrieve the necessary information when seeing the patient. For example, a general practitioner can explain a patient’s pathology results when they see the patient instead of only reading and interpreting the test result when the patient is in the appointment room. Depending on your workplace protocol, you may also be tasked to contact patients ahead of their appointment time - usually a day before - to confirm their appointment.
While most healthcare settings use electronic health records which are easier to access patient records such as searching for the patient’s last name, there are still some practices that use physical records. If your workplace has not digitalise patient records, then you would need to find the patient’s physical file. It is also your responsibility to have a clear understanding of your workplace’s filing system. This can be in alphabetical order according to the patient's last name or a colour coding system whereby a colour is allocated for the first alphabet of the patient’s last name, e.g., green for K, black for D.
Watch
Watch
Coding system
To improve information sharing and communication among healthcare workers, coding systems are used to standardise medical terminologies and concepts, and it is typically used for administrative purposes such as billing and insurance. Sometimes, this information is also coded for research purposes.
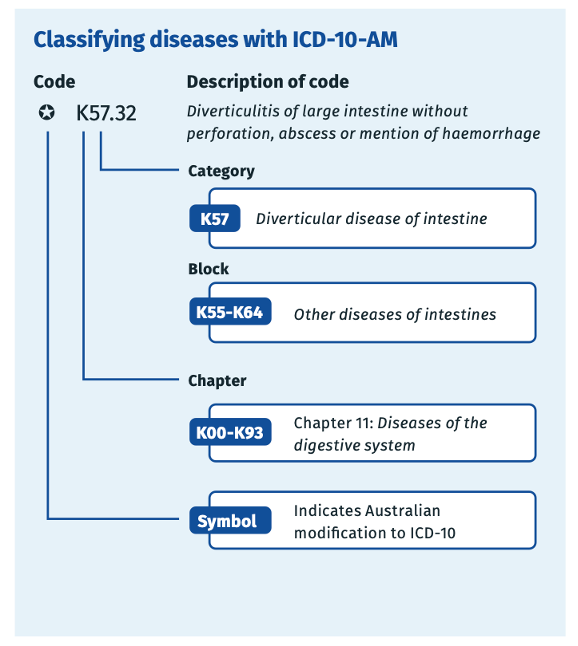
The clinical coding system that is used in Australia is the ICD-10-AM (The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification). It is a classification of diseases based on the World Health Organisation International Statistical Classification of Diseases and Related Health Problems (ICD-10). The codes in this coding system are alphanumeric codes and its length is three to five characters, excluding any punctuation (Queensland Health, n.d.). This coding system is used to classify diseases, injuries, and related health problems. See the diagram below for an example of a code (Independent Health and Aged Care Pricing Authority, 2023, p. 2):
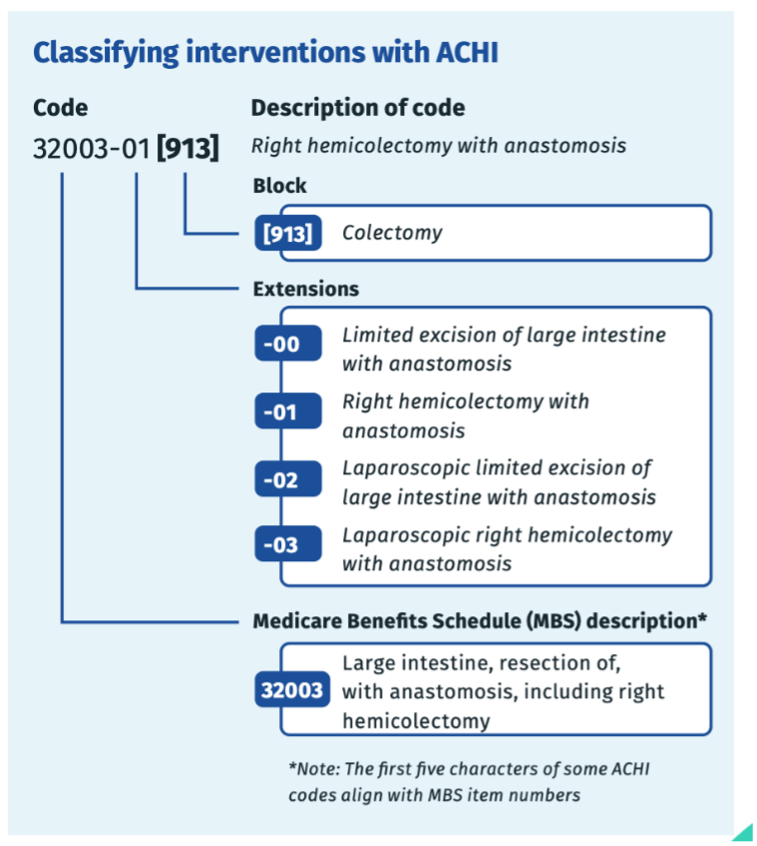
Australian Classification of Health Interventions (ACHI) is a coding system that is used to classify surgeries, therapies, and health interventions. See the diagram below for an example of the ACHI coding system (Independent Health and Aged Care Pricing Authority, 2023, p. 2):
As a health worker, you are not expected and responsible for coding patient records, as it is often undertaken by a qualified clinical coder who is professionally trained. However, it will be beneficial for you to understand the different coding systems so that you know how to access and retrieve patient information from the health information system quickly by using the clinical code. It can also help to minimise error when entering a patient’s diagnosis and treatment received into their patient record. That said, if your workplace involves a coding system (e.g., medical centre), then your workplace would most likely have a manual or classification book that lists the code and corresponding description. Further, you will also receive relevant training and instructions from your supervisor.
Tip
Find Out More
If you are interested to learn more about the clinical coding system, you could take some time to look through the online learning module about ICD-10-AM here: https://learn.ihacpa.gov.au/.

When patients arrive for their appointment at the practice and you are checking them in, you would need to check that their information is current and accurate, such as their phone number and address. For example, “Morning Jane, thank you for coming in today. Can I just check whether your phone number is ending 123 and you’re still at Grey Street?” You can then verify this against the information in their patient record, and update any changes accordingly.
Depending on your workplace protocol, there may be additional circumstances and information that you need to verify patient information. According to Royal Australian College of General Practitioners (2023), a general practice is expected to identify a patient using three approved patient identifiers each time they attend or call the practice, which include:
- Name (family and given names together are one identifier)
- Date of birth
- Gender (as identified by the patient)
- Address
- Patient health record number where it exists
- Individual Healthcare Identifier
A patient’s Medicare number is not an approved patient identifier, as some Australian residents and visitors do not have a Medicare number and others may share numbers if they belong to the same family.
(Royal Australian College of General Practitioners, 2023)
This is an important step when checking currency and accuracy of patient information because it can reduce the risk of misidentification. Not only that, but healthcare professionals will also have the correct patient record for the appointment to avoid any potentially life-threatening consequences for the patient.
While it is important to ensure that the patient information is correct and recent, it is also vital to respect and protect the privacy and confidentiality of the patient. To do so, you may want to adopt the following methods when verifying information with them:
- Lower your volume to avoid the information being overheard by others in the practice.
- Avoid saying all the digits in the phone numbers, e.g., verify the last four digits or the street that the patient lives in.
- Respect the patient’s wish to remain anonymous, e.g., they may be at risk in domestic violence situations.
Your workplace will also have relevant protocols to help protect patient’s privacy and confidentiality, which you are expected to familarise yourself with and actively apply in your role.
Watch
Watch
Next watch this video about a Dental Practice explaining how to do small talk with patients.

When a patient is attending your practice for the first time, you will need to create a new patient record for them. The record usually includes the patient’s personal information such as their contact details, medical history, allergy information, and any information relevant to their visit to the practice. This is usually collected via a physical form, and you will then enter the information into respective fields on the record management system. When you are entering information, make sure that you are entering the correct information in the correct fields. You should also review the patient information entered against the form and ensure they are accurate and complete, and make any necessary corrections, as a small mistake may have serious consequences.
Depending on your practice’s protocol, you may assign a unique patient tag or ID on the record system. This will be useful to identify the patient in the future. Also, some places use electronic devices such as tablets for patients to fill in the form instead. Regardless, you should make sure you are creating records according to the practice’s protocol and policies so that these records can be accessed efficiently by other workers too.

Privacy Policy
When you are creating a new patient record, you are collecting a patient’s health information. You should do so only with the patient’s informed consent - the patient should understand what will happen to the information they provide and what they are consenting to. Generally, this consent is explicitly provided by the patient, i.e., when they provide their signature and agree to the practice’s privacy policy when filling in the patient form.
While the patient form would include details about how the patient’s information will be collected and used, and who has access to it, there may be some patients who require further clarification. In those cases, you are expected to provide the relevant information and clarify your practice’s privacy policy with them. Remember, you should never coerce the patient to provide consent - it should be provided voluntarily.
See below an example of information that may be collected to create a new patient record.

After the patient’s appointment, you should review their record and check whether there are any instructions from health care professionals. These instructions usually include:
- Schedule follow-up appointments
- Referrals to other health professionals
- Requests for pathology tests or x-ray scans
- Setting up reminders for follow-up actions such as immunisation schedules or routine tests.
You should also check whether the healthcare professional’s notes or observations are complete and accurate, for example, if there are any missing fields or fields incorrectly entered. You should then inform and clarify the healthcare professional immediately to make the corrections.
If you are instructed to schedule follow-up appointments with the patient, you should assist the patient to do so and ensure they are informed of the correct date and time. For example, “Jane, Dr. Koh recommended that you schedule a follow-up appointment in six weeks’ time, would you like to schedule an appointment then? Would the same day and time work for you?”. Some patients may not want to schedule the next appointment on the spot, and depending on your practice protocol, you could offer to schedule a follow-up call closer to the date and schedule an appointment then.
Sometimes, patients might be confused or want further clarification about follow-up instructions and may ask you about certain instructions. You could read the note or instructions left by the healthcare professional and explain further to the patient. However, if you are unsure, you should always clarify with the healthcare professional instead of making your own assumptions.
As mentioned, it is vital to protect patients’ privacy, especially their health information. Therefore, you must adhere to your practice’s policies and protocols regarding information storing. This way, you also ensure you and your practice are compliant with the privacy legislations. While your practice will have policies and protocols about information storage, read the extract below that summarises some key steps to be taken to ensure the security and safety of patient record:
- keeps all records (not just clinical records) secure
- ensures that only the appropriate staff have access to these records
- keeps records, storage areas clean and clear of clutter
- makes sure staff understand policies on storage, damage and alteration of records and
- take the appropriate action if a breach occurs
- checks records regularly for unauthorised alteration or deliberate damage
- makes sure all staff are aware of the consequences of fraud
- makes sure all staff are aware that records are checked for accuracy and all suspected
- cases of Medicare fraud are reported
- has a disaster recovery plan in place, in case of the loss or destruction of
- records, and
- makes sure all electronic records are backed-up and that the integrity of the back-up data
- is also checked.
(Department of Health, 2021, p. 9)
In addition, you should be aware that different staff members would have different staff access levels to access different patient information. You should respect your practice’s policies regarding this and not access information that you are not authorised to, e.g., asking a staff member to show you patient information that you have no access to.
Read
Reading C – Electronic Administrative Record Keeping Checklist
Most practices use electronic patient information management systems, which may require additional steps to ensure patient data are secured. Reading C provides a checklist of how to practise good electronic record keeping, which you can refer to.
This section looked at how you could access patient records. We first looked at how to check patient information for accuracy and currency and how to create new patient records. This section also looked at how you could check on patient information for any follow-up actions that needs to be taken. Lastly, you learned about the storage of patient record such that it adheres to the legislative requirements and your workplace’s privacy policies and protocols.
