Reading A: AAPM's Code of Ethical Conduct
Reading B: Roles and Responsibilities
Reading C: Universal Declaration of Human Rights
Reading D: A Quick Guide to Australian Discrimination Laws
Reading E: Informed Consent
Reading F: Statutory Schemes
Reading G: Mandatory Reporting of Child Abuse and Neglect
Reading H: WHS Code of Practice
Reading I: Ethical Decision-Making in Confidentiality Dilemmas
Reading J: Protections at Work
Important note to students: The Readings contained in these Readings are a collection of extracts from various books, articles and other publications. The Readings have been replicated exactly from their original source, meaning that any errors in the original document will be transferred into these Readings. In addition, if a Reading originates from an American source, it will maintain its American spelling and terminology. IAH is committed to providing you with high quality study materials and trusts that you will find these Readings beneficial and enjoyable.

Fundamental Principles
Following a comprehensive consultation process, Members of AAPM have identified the following fundamental ethical principles as central to their professional practice:
1. Principles of Justice and Fairness
• Honesty – to be truthful, trustworthy, straightforward, fair, and sincere in all professional and business relationships.
• Integrity - to be consistent in action, values, methods, measures, principles, expectations, and outcomes.
• Respect – to acknowledge that every human being, regardless of race, religion, gender, age, sexual and gender diversity, or other individual differences is entitled to unconditional respect and has a right to maximise his or her potential providing it does not infringe upon the rights of others.
• Good Faith - to exercise his or her responsibilities reasonably and not arbitrarily or for some irrelevant purpose, having regard to the legitimate interests of other affected parties.
2. Principles of Care and Empathic Understanding
• Empowerment – to facilitate autonomy, independence, and self-determination in people and communities by providing appropriate resources and support
• Dignity –to value the uniqueness of every individual and uphold the responsibility to provide services around each individual and their specific needs.
• Privacy – to value the privacy of individuals as an inherent right and acknowledge the right to privacy by maintaining confidentiality of information shared by patients and other stakeholders.
• Communication – to value communicating with individuals in ways that are meaningful to them and enables them to understand and clarify the issues at stake.
Justice and Fairness
The ethical principle of Justice asserts that people ought to be treated equally, while recognising the unique circumstances of individuals. This standard requires that everyone is afforded their basic rights and can participate in any decision-making process that might affect those rights. Fairness refers to the expectation that we are acting impartially, whatever our own emotions and interests regarding the issues in question, as well as to the outcomes of the process.
Honesty
Honesty is a principle that is closely related to justice. It means that all of the facts related to any particular issue are conveyed to others. It also means that nothing of relevance to any dealings with others are deliberately omitted or hidden. In order to observe this principle, Members of AAPM strive to be truthful, trustworthy, straightforward, fair, and sincere in their professional conduct.
They:
• Recognise that honesty forms the foundation of trust, which is essential in all their professional relations.
• Adhere to the highest standards of accuracy and transparency in their communications.
• Comply with all relevant privacy laws and laws regarding the management of health records in the protection of personal information received from clients in a healthcare practice.
• o Ensure that their employees and associates also comply with this provision and monitor employee activities to ensure privacy and confidentiality standards are maintained.
Integrity
Acting with integrity means understanding, accepting, and choosing to live in accordance with one's principles. It is the practice of showing a consistent and uncompromising adherence to an internally consistent moral and ethical framework. It requires the avoidance of any arbitrary choices that make exceptions for a particular person or group. The sense of wholeness accompanying integrity communicates an impression of trustworthiness to others, facilitating professional relationships. To ensure integrity, Members of AAPM aim to be consistent in action, values, methods, measures, principles, expectations, and outcomes.
They:
• Act according to the values, beliefs and principles that are expected of Members.
• Fulfil their promises and commitments to their clients, employees, and colleagues.
• Show leadership in their relations with clients, employees, and colleagues by working to resolve issues constructively and in mutually acceptable ways.
Respect
The principle of respect is based on the assumption that all competent humans are autonomous and have the right to make their own decisions freely without fear of interference. Autonomous people are considered to have the capacity to determine their own destiny, and as such must be respected unconditionally. Members of AAPM acknowledge that every human being, regardless of race, religion, gender, age, sexual and gender diversity, or other individual differences is entitled to unconditional respect and has a right to maximise his or her potential, and exercise their right to free choice, providing it does not infringe upon the rights of others.
They:
• Ensure people who can responsibly make their own decisions, are given serious consideration and people who are not able to take responsibility for their own decisions are supported appropriately.
• o Have regard for others’ personal space, opinions, and privacy, ensuring that harassment or bullying in any form is not tolerated.
Good Faith
Members of AAPM endeavour to exercise their responsibilities reasonably and not arbitrarily or for some irrelevant purpose, having regard to the legitimate interests of other affected parties.
• Act with honesty and impartiality when providing service or advice to others
• Provide comprehensive information that others need to know in order to make informed decisions.
Care and Empathic Understanding
Principles of care and empathic understanding reflect the view that relationships form the context in which sound ethical decisions are made. It requires that ethical decision-makers are mindful of the well-being of others and seek to act benevolently wherever possible. They emphasise the importance of each individual and the degree of interdependence between those involved in an ethical dilemma.
Care and empathic understanding imply a responsiveness to the lived experience of those in vulnerable positions rather than understanding how we might experience similar situations. Competence in providing care, not simply the awareness or acknowledgment that care is needed, becomes an imperative. Attentiveness to specific details of the context help moral agents to determine how they might safeguard and even promote the interests of those involved in such situations.
Empowerment
Members of AAPM aim to facilitate autonomy, independence and self-determination in people and communities by providing appropriate resources and support in relation to their professional undertakings.
They:
• Presume that individuals are competent in assessing and acting on their interests.
• Support individuals to make informed decisions that are in their own best interests.
Dignity
Members of AAPM value the uniqueness of every individual and uphold the responsibility to provide services around each individual and their specific needs.
They:
• Respect the inherent dignity, worth, and unique attributes of every person.
• Acknowledge the rights of each individual and engage in positive, unbiased interactions that observe those rights.
Privacy and Confidentiality
Members of AAPM value the privacy of individuals as an inherent right and acknowledge the right to privacy by maintaining confidentiality of information shared by patients and other stakeholders.
They:
• Respect and maintain the confidentiality of information acquired in the course of their professional duties and ensure policies are in place to prevent disclosure of such information, except when authorised or legally required to do so.
• Refrain from using information obtained in the course of their work for unethical or illegal advantage, personally or through a third party.
Communication
Members of AAPM aim to communicate with individuals in ways that are meaningful to them and enables them to understand and clarify the issues at stake.
They:
• Communicate truthfully, concisely, and responsibly with others.
• Listen non-judgementally to others and identify their unique perspectives and points of view.
• Communicate information to other parties fairly and objectively.
• Ensure their communications have been understood and clarify any ambiguities or address any questions that might arise.
Conflicts of Interest
A conflict of interest occurs when a member’s personal interests’ conflict with their responsibility to act in the best interests of AAPM and any of their fiduciary and social obligations. It may also be unlawful. AAPM members:
• Identify potential conflicts of interest and manage them appropriately.
• Consult other members, particularly senior and more experience Practice Managers regarding potential conflicts of interest.
N.B. The issue of conflicts of interest is complex, and further discussion of some of the many aspects involved is provided in the appendix.
What to do if you have concerns
If informal methods of dealing with ethical concerns are deemed to be unsatisfactory by any of the parties concerned, including patients, healthcare practitioners, members of the public and fellow Members, formal complaints about the conduct of AAPM members can be raised with the Association.
This Code and the Rules and Procedures for managing complaints raised may be reviewed and updated from time to time by the National Board. The current version is provided in Appendix A. Anyone with concerns about AAPM members is encouraged to read both documents before contacting the AAPM for further information.
AAPM aims to:
1. deliver an effective complaint handling system founded on the principles of fairness, accessibility, responsiveness, and efficiency.
2. ensure individuals who make a complaint are respected and aware of the process of consideration of their complaint and the outcome.
3. provide transparency around AAPM’s process for receiving, handling, and investigating complaints. 4. enable AAPM to apply lessons learnt from complaints received for continuous improvement.
A formal complaint may be made in any form of writing including on paper, received electronically via email or through the contact form available at https://www.aapm.org.au/About-Us/Contact-Us;
Complaint Handling Policy
1. Purpose
This document sets out the AAPM Complaint Handling Policy. A complaint about an AAPM Member is subject to the AAPM By-laws for handling complaints about AAPM Members which is available at the AAPM website. The purpose of this policy is: 1. to deliver an effective complaint handling system founded on the principles of fairness, accessibility, responsiveness, and efficiency. 2. to ensure individuals who make a complaint are respected and aware of the process of consideration of their complaint and the outcome. 3. to provide transparency around AAPM’s process for receiving, handling, and investigating complaints; and 4. to enable AAPM to apply lessons learnt from complaints received for continuous improvement.
2. Who this Policy Applies to
Any person can make a complaint to AAPM regarding any aspect of AAPM’s operations. AAPM can only consider complaints that have some connection to AAPM’s operations. This policy must be considered alongside other AAPM policies. A complaint that more appropriately falls within the AAPM Whistle-blower Policy, Code of Ethical Conduct or another applicable policy, will be dealt with in accordance with the appropriate policy.
3. Matters that can be considered under this Policy
AAPM will consider any complaint that has some connection to AAPM and in respect of which it has the necessary authority or ability to enforce a decision, including complaints made about: o AAPM operations or activities. o conduct of officers, employees, agents, or contractors of AAPM; or o conduct of Members of AAPM. This policy may also be applied for consideration of work-related grievances and other complaints personal to an individual.
4. Where to make a Complaint
Where a complaint should be sent depends on the nature of the complaint:
• Complaints about Members of AAPM
AAPM has a policy and process for complaints about members which is available from the AAPM website. Information about how to make a complaint about an AAPM Member is set out in that policy.
• Complaints about AAPM staff
Complaints about AAPM staff should be marked “confidential” and sent directly to the office of AAPM’s CEO at ceo@aapm.org.au
• Complaints about the AAPM CEO or a Board member
Complaints about the CEO or a Board member should be marked “confidential” and sent directly to the Chair of the AAPM Board at president@aapm.org.au
• Complaints about the President or Chair
Complaints about the President should be marked “confidential” and sent directly to the office of AAPM’s CEO at ceo@aapm.org.au
• Other complaints can be made via email addressed to any one of the following:
o State committee – ceo@aapm.org.au
o CEO - ceo@aapm.org.au
o Board - president@aapm.org.au
Any complaints received at a State Branch Committee level should be referred to the AAPM National Office promptly for management to promote national consistency in complaints handling. Any complaint received can be escalated to the CEO or the Board at the discretion of an AAPM National Office employee who received the complaint.
5. How to Make a Complaint
Complaints should be made in writing to assist in record keeping, assessment and investigation. AAPM may decline to consider any verbally received complaint.
A complaint:
• may be in any form of writing including on paper, received electronically via fax or email or through the contact form available at https://www.aapm.org.au/About-Us/Contact-Us;
• must include sufficient information to enable AAPM to property assess the complaint. o may include any additional information the complainant considers relevant; and
• must include the name and contact details of the complainant, and a statement about whether the complainant wishes to remain anonymous. o must state the outcome being sought.
Complaints that do not include the name and contact details of the complainant may not be investigated.
Details such as dates, times, locations, and other persons present may be necessary information to enable a person who is the subject of a complaint to properly respond, and for AAPM to properly investigate the complaint.
Where a complaint is made about operations or activities of AAPM, a complainant should be encouraged to provide alternative options to any issues raised, rather than simply identifying a problem.
6. Acknowledging a complaint
AAPM aims to acknowledge receipt of a complaint within three (3) business days of receipt, and to provide to the complainant a copy of this policy for reference.
7. Assessing a complaint
Within seven (7) business days of receipt, the recipient of the complaint will assess the complaint to:
• identify that AAPM has the necessary authority or power to consider the complaint and enforce any decision made in respect of the complaint.
• determine whether the complaint should be handled in accordance with this policy or another more appropriate AAPM policy.
• identify whether another person or entity is mentioned in the complaint and should be provided an opportunity to respond.
• determine who is best positioned to investigate and respond to the complaint.
Having assessed the complaint, the person then designated to handle the complaint must notify the complainant and any person or entity required to respond to the complaint of their findings and the process and timing to be followed from that point forward.
Where the assessor’s finding is that AAPM has no authority or power to consider the complaint, the complainant must be notified of that finding and advised that the complaint process is then at an end.
Where a person or entity impacted by the complaint is given an opportunity to respond, they will be requested to provide their written response to the complaint within seven (7) days of receipt of that notice.
8. Responding to a complaint
Anyone responding to a complaint must provide a written response to the complaint within seven (7) business days of the request for their response.
A written response to the complaint:
• should be succinct and factual o must be addressed to the person requesting the response o must be in writing o must address the complaint
• may include any information the respondent considers relevant
• may include supporting statements from other people, and
• may request further time to respond, provided that a fixed date for the response is nominated at the time of that request and is not more than 30 days later than the original date to respond.
9. Investigation
If additional information is required by the investigator, that person may request that information from any person, seeking a response within seven (7) days, and notifying the person from whom information is requested that the complaint will be considered without that information if it cannot be provided within that timeframe.
10. Fair assessment and investigation of a complaint
AAPM acknowledges that this policy will not be meaningful and effective unless it is implemented and applied consistently throughout AAPM in practice.
A complainant must be treated fairly. Fairness comprises three qualities—impartiality, confidentiality, and transparency.
Impartiality – a person receiving, assessing, or investigating a complaint must aim to:
• avoid a conflict of interest
• avoid defensiveness
• avoid seeking to prove right or wrong
• avoid bias (conscious or unconscious) or prejudice o remain open minded o remain objective
• give equal consideration to information received from different sources
• disregard any prior complaints from, or relationship with, the complainant
Confidentiality – a person receiving, assessing, or investigating a complaint must aim to:
• keep the complaint confidential and secure
• limit access to the complaint to those directly involved and required to assess or investigate the complaint
• not share or discuss the complaint other than in accordance with this policy
Transparency - a person receiving, assessing, or investigating a complaint must aim to:
• inform any person impacted by the complaint of the process and timing of for handling the complaint
• ensure the complainant and any person impacted have contact details of the person handling the complaint
• keep the complainant and any person impacted reasonably informed of the progress of the complaint handling process
• provide an explanation of the outcome of the complaint handling process
The principles of natural justice and procedural fairness should be applied in the receipt and consideration of any complaint, and as part of the investigation process before any adverse action is taken against person or entity that may be the subject of a complaint.
Procedural fairness involves being afforded the opportunity to respond to a comment or allegation made, within a reasonable time. This means that if any complaint is received in respect of a person or entity, that person or entity must be notified promptly, and given reasonable opportunity to present their response to the complaint. Procedural fairness does not require the decision maker to find any information provided to it as factual, true, or persuasive.
To ensure that these principles can be adhered to, a complainant may be advised that their complaint cannot be properly investigated or responded to if they decline to share sufficient details for a person named, to respond.
AAPM may appoint an independent third party to investigate a complaint at its discretion.
11. Determination of a complaint
Initial Findings – The investigator will prepare initial findings about the complaint and provide those findings to the complainant and any respondent. Either or both the complainant a respondent may respond in writing to the initial findings within fourteen (14) business days.
Final Determination – The investigator will consider all responses to the initial findings received within the required timeframe and prepare a final determination of the complaint.
The final determination is final and there will be no avenue of appeal from that decision.
Any actions required as a result of the final determination will take effect at the times noted in the final determination.
The investigator is under no obligation to provide reasons to any party other than the complainant or a respondent.
12. Reviewing the complaint handling process
AAPM will keep a record of complaints received including the nature of the complaint, whether the complaint was investigated and the final determination.
At the conclusion of each complaint process, the person handling the complaint will complete a short report that includes:
• the timing of the complaint and complaint handling process
• whether any unexpected problems arose in the process and how they were managed
• what worked well
• what did not work well o what could be done better – and how?
A report will be provided to the Board at least annually identifying any areas of improvement implemented as a result of the above complaint review process.
13. Ensuring the Policy is Easily Accessible
This policy is displayed on the AAPM website, in the Member’s portal of the AAPM website, and included with AAPM employment policies.
By-laws for handling complaints about AAPM Members - Complaints regarding a breach of code
1. Making a complaint
1.1 The National Board can only investigate a written complaint about a member. Verbal complaints will not be treated as a complaint for the purpose of these bylaws.
1.2 Upon receipt of a written complaint, the National Board (through the CEO) will investigate the complaint and the conduct of the Member being complained about.
1.3 If a complaint is received from an eligible whistle-blower about a disclosable matter, then the complaint will be dealt with in accordance with the AAPM Whistle-blowers Policy rather than these by-laws and the complainant will be advised accordingly.
1.4 A written complaint:
• must be addressed to the CEO or the AAPM National Board and received at the principal place of business of AAPM.
• may be in any form of writing including on paper, received electronically via fax or email or through the contact form available at https://www.aapm.org.au/About-Us/Contact-Us;
• must include the name of the Member about whom the complaint is made.
• must summarise the behaviour complained about, including the date and location where the behaviour occurred.
• where possible, should make reference to the particular provision in the AAPM Code of Ethical Conduct which it is alleged the Member has contravened;
• may include any additional information the complainant (the person making the complaint) deems relevant to the National Board’s investigation of the complaint and
• must include the name and contact details of the complainant, and a statement about whether the complainant wishes to remain anonymous. Complaints that do not include the name and contact details of the complainant will not be treated as a complaint under these bylaws.
2. Principles for investigating complaints
2.1 The complaint and investigation process will be conducted by the National Board in accordance with the following five principles:
• Confidentiality for all parties, where practicable and appropriate, until the investigation process is completed.
• Investigations will be handled expeditiously.
• Procedural fairness for both the complainant and the Member. Procedural fairness involves being afforded the opportunity to respond to a comment or allegation made, within a reasonable time. Procedural fairness does not require the decision maker to find any information provided to it as factual, true, or persuasive. V9 Updated 12 October 2022
• The National Board may inform itself as it sees fit, including seeking external expert opinion or delegating any part of whole of the investigation to nominated AAPM staff members or consultants engaged for the purpose. The National Board is not bound by any rules of evidence.
• The National Board may expand or limit the scope of its investigation as it sees fit.
3. Remaining anonymous
3.1 If a complainant asks to remain anonymous (i.e., unidentified to the member about whom the complaint is made), the National Board or its delegate will make a determination as to whether the Member complained about will have sufficient ability to address and respond to the complaint without the disclosure of the identity of the complainant, if the complainant remains anonymous.
3.2 If the determination of the National Board is that the Member complained about will have sufficient ability to respond to the complaint, the details of the complainant will not be provided to the Member complained about.
3.3 If the determination of the National Board is that the Member complained about will not have fair opportunity to respond to the complaint without the identity of the complainant being disclosed, the National Board will advise the complainant that the complaint cannot be investigated and will come to an end unless the complainant is prepared to be identified as the complainant.
3.4 The National Board may at any time throughout the investigation process close any complaint without further investigation or determination, and notify the complainant accordingly, where the complainant refuses to be identified and the Member complained about cannot adequately respond without that information.
4. Procedure for investigating complaints
4.1 Within 3 business days of receipt of a written complaint:
o a written acknowledgment of receipt will be provided to the complainant and
o the National Board will be notified that the complaint has been received.
4.2 Within 7 business days of receipt of a written complaint:
• a copy of the complaint will be provided to the National Board.
• the CEO or other delegate of the National Board will provide a report to the National Board that:
- confirms the person complained about is a financial Member of AAPM or was a financial member of the AAPM at the time the alleged conduct occurred.
- identifies the category of membership of the Member.
- identifies what provisions of this Code may have contravened.
- identifies any other Members or third parties who may be involved in the investigation process,
• where the complaint has been received about a current or former Member, a copy of the complaint will be provided to that person via post and electronic means sent to the address details on record at AAPM.
4.3 If the person complained about is not a current Member or was not a member at the time of the alleged conduct, the complainant must be promptly notified that the National Board has no authority to consider the complaint. This will bring the complaint to a close.
4.4 At the same time as acknowledging receipt of the complaint or providing a copy of the complaint to the Member complained about, the parties will be provided with an information statement outlining the investigative process and likely timeframes.
5. Responding to a complaint
5.1 The Member complained about must provide a written response to the complaint within 7 business days of his/her receipt of the complaint.
5.2 The written response to the complaint:
• must be addressed to the CEO or the AAPM National Board and received at the principal place of business of AAPM. o may be in any form of writing including on paper, received electronically via fax or email or through the contact form available at https://www.aapm.org.au/About-Us/Contact-Us;
• must include the name of the Member who the complaint is about and refer to the complaint.
• must include an introductory summary of the Member’s response including any aspects of the complaint the Member agrees with.
• may include any information the Member deems relevant to the National Board’s investigation of the complaint.
• may include supporting statements from other people, and o may request further time to respond, provided that a fixed date for the response is nominated at the time of that request and is not more than 30 days later than the original date to respond.
6. Considering the complaint material
6.1 Upon receipt of the response, the National Board or its delegate will review and consider the information received from the complainant and in the response and determine whether any further additional information is required or should be obtained in order to determine the complaint.
6.2 If additional information is required the National Board may request that information from any person, seeking a response within 7 days, and notifying the person from whom information is requested (whether the complainant, the Member complained about or another person) that the complaint will be considered without that information if it cannot be provided within that timeframe.
6.3 Where additional information requested under 6.2 is not provided within the 7-day deadline, the Board will proceed with the complaint based on the information to hand.
7. Initial Findings
7.1 The National Board or its delegate will prepare initial findings about the complaint and provide those findings to the complainant and the Member complained about. Either or both the complainant and the Member complained about may respond in writing to the initial findings within fourteen (14) business days. Provision of initial findings are deemed to satisfy the requirements of rule 10.5(b) of the Constitution.
8. Final Determination
8.1 The National Board or its delegate will consider all responses to the initial findings received within the required timeframe and prepare a final determination of the complaint. The National Board or its delegate may publish a final determination that is the same as the initial findings, despite receipt of information in response to the initial findings.
8.2 The final determination is final and there will be no avenue of appeal from that decision.
8.3 Any actions required as a result of the final determination (e.g., Member suspension) will take effect immediately. The National Board may notify the AAPM membership of the results of its determination but is under no obligation to provide reasons to any party other than the complainant or the Member complained about.
9. Consequences of finding a contravention of the Code
9.1 Where the National Board determines that there has been a contravention of this Code by a Member, the National Board may do any one or more of the following:
• take no action.
• issue a warning to the Member.
• suspend the Member’s rights as a member for a period of time of no more than twelve (12) months, meaning the Member will be excluded from access to all member benefits, and not able to hold themselves out as being a Member of AAPM during the period of suspension, as well as being excluded from AAPM events.
• suspend the Member’s ability to access any one or more of the benefits of membership (e.g., nominating to serve on a state committee, nominating for a particular category of membership etc.) for a specified period of time of no more than twelve (12) months, and for period of suspension no fees will be refunded or extended.
• place conditions on the Member’s membership, including requiring the Member to repeat or undertake additional education or training within a specified timeframe.
• change or revoke a category of membership previously awarded to that Member.
• expel the Member from AAPM.
• refer the decision to an unbiased, independent person on conditions that the Board consider appropriate (however, the independent person can only make a decision that the Board could have made pursuant to these by-laws), and o make a recommendation on how AAPM Members can be educated to avoid the misconduct or breach of the Code of Ethical Conduct in the future.
10. Complaint process – likely time frames
0 days Receipt of written complaint by AAPM.
+3 business days from AAPM’s receipt of complaint Written acknowledgement of receipt of complaint to complainant with information statement about process. National Board notified that a written complaint is received.
+ 7 business days from AAPM’s receipt of complaint Copy of complaint provided to National Board with confirmation of Membership status of person complained about. Copy of complaint provided to Member complained about, with information statement about process
+ 14 business days from AAPM’s receipt of complaint Member complained about provides written response to the complaint.
+ 17 business days from AAPM’s receipt of complaint National Board considers complaint and response and the Board or its delegate may request additional information from any person
+ 21 business days from AAPM’s receipt of complaint Additional information received by National Board and considered.
+ 23 business days from AAPM’s receipt of complaint National Board prepares initial findings and provides to complainant and Member complained about for consideration.
+ 37 business days from AAPM’s receipt of complaint Complainant and Member complained about may provide a response to the initial findings of the National Board.
+ 40 business days from AAPM’s receipt of complaint National Board considers responses to initial findings and prepares final determination of complaint
+ 45 business days from AAPM’s receipt of complaint Final determination of complaint is provided to complainant and Member complained about, with notification of any aspects of the complaint that will published (e.g., Member sanctioned).
APPENDIX
Conflict of interest:
Conflicts of interest form a particularly fraught area of ethical debate for Practice Managers. It requires specific consideration in the Code of Ethics.
A conflict of interest occurs when a member’s personal interests’ conflict with their responsibility to act in the best interests of AAPM, clients, colleagues, and other professionals. Personal interests include those of family, friends, or other organisations a person may be involved with (for example, as a consultant). It also includes a divergence between a member’s responsibilities as a member of AAPM and another duty that the Member has, for example, to another organisation.
A conflict of interest may be actual, potential, or perceived. It may be financial or non-financial. It represents potential risks to reputation, good governance, accountability, transparency, and organisational dynamics. It may also be unlawful.
• The impact of a potential or perceived conflict of interest may well be as damaging to the reputation or management of AAPM as an actual conflict of interest. Each potential event must be assessed and managed accordingly.
• A perceived conflict of interest requires input from impartial third parties. Careful consideration of the perspective of someone who is not directly involved in the perceived conflict is vital. One possible course of action is to undertake consultation and discussion with other members, particularly senior and more experience Practice Managers. Promoting a culture of disclosure helps facilitate constructive consultations.
• A perceived conflict of interest can often be best addressed by removal or avoidance of the perceived conflict itself.
Members of AAPM:
• Conduct relationships in a manner which gives assurance to all parties concerned that their position will not be compromised, and their interests given fair consideration.
• Disclose to potential clients or employers any direct or indirect personal interest which might cause conflict, either real or perceived.
• Neither accept nor offer gifts or benefits with the expectation, or likely consequence of influencing, decision making.
• Do not promote themselves in a self-laudatory manner.
• Do not publicly criticise other members of AAPM.
For more detailed discussion, members are recommended to consult the following document: Australian Charities and Not-for-profits Commission (2015). Conflicts of Interest. Download from: www.acnc.gov.au
Case Studies
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
|
A Patient who has engaged in selfharming behaviours has been referred to see a psychologist but is refusing to do so. The patient’s family is unaware of the self-harming behaviour. The patient states they only trust the GP and refuses to see anyone else. Despite the best efforts of the GP, the patient continues to selfharm and refuse referrals. |
• You are concerned that the patient, without effective treatment, may eventually die. This raises issues around principles of Care and Empathy. • The stress on the GP is understandable and might affect other patients. This also raises issues of Care, as well as Justice Principles, as first we must “do no harm”. • The Practice has responsibility for the patient’s treatment. Refusing to continue treatment, because of noncompliance with the GP’s recommendations, might amount to withdrawing the only current source of treatment. Justice principles are again invoked because it is unfair to withdraw treatment without valid reasons. • There are legal implications for the GP and for the practice if treatment is suspended or if it is continued for the noncompliant patient. These might raise further issues impacting on staff and patients. |
• Engage the patient in a strategic conversation, exploring all points of view. As well as understanding the patient’s reluctance better, it also allows the needs of the Practice to be considered, including: • Inviting the patient to see another GP in the Practice for a second opinion. This would protect the patient’s dignity and respect their autonomy, while • Explaining again to the patient why it is essential they receive specialist treatment from a psychologist. This would ensure the patient makes fully informed decision about their health care options. • Advising the patient that the Practice has a policy that a condition of continuing to treat them as a patient is contingent upon a patient following the GP’s treatment recommendations. • Carefully document all conversations with the patient to record all efforts to persuade the patient to get specialist help. • Discuss the issues with the GP and consider ways that the GP could empower the patient to engage with other health professionals. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| A doctor is requesting the Practice Manager allow a patient to bulk bill a telehealth care plan, even though this would be incorrect. |
• The doctor is aware of the patient’s financial and clinical circumstances and is trying to help. • The care plan item number activates access to other MBS services from other providers potentially contributing to patient health outcomes. The patient may miss any opportunity for allied health care if the patient cannot pay privately for all services. • The principle of Beneficence is raised in this case, as the doctor is motivated by the intention to “do good” for the patient. The principle of care and empathy is apparently driving the doctor’s decision making, blurring the importance of other principles. • Aspects of Integrity are also raised by the implications of the course of action proposed by the doctor. |
• One approach might be to initiate a conversation with the GP to discuss the decision-making process. • It can provide an opportunity to review the ethical issues: • It can provide opportunities for information sharing – e.g.: • Suggest the GP has a conversation with patient about costs and relevant rebates - as per RACGP and MBS requirements. • Document any conversation that occurs and spell out the billing instructions of GP. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| A current patient’s parent is seeking access to Medicare rebates for a Mental Health Care Plan and referred Better Health via Telehealth for the patient who is not presently in Australia. |
• The Patient is affected by Covid restrictions, and his mental health is deteriorating, creating issues of care and empathy for the patient, parents, and health professionals. • Access to Psychology/Psychiatrist services through referral would minimise the cost services through the Medicare rebate. It introduces aspects of Justice Principles. • Legal constraints on the Practice Manager raise ethical issues around Integrity and trustworthiness. |
• Practice Managers will probably feel concern and empathy for the patient yet will realise they cannot comply with the parents’ request. Nevertheless, they are able to discuss their dilemma with them and provide clarification. • Explain the Medicare requirements in plain language to ensure they are understood effectively. • Discuss accessing service providers local to the patient’s current location overseas. • Explore the possibility of the parents offering financial support for patient’s immediate care. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| An employee reports that a colleague is experiencing workplace harassment and bullying from a doctor within the practice. The colleague is reluctant to approach the Practice Manager directly but is distressed and unsure what to do |
• There is potential for deleterious impact on employee physical, mental, emotional wellbeing, raising issues of Care and Empathy. • There is potential for deleterious impact on employee workplace performance and absence, raising concerns of fairness for all employees. • There is impetus for an impartial investigation of allegation invoking the principle of Justice. • Possible legal claims against doctor and practice arise, e.g. a WH&S claim. • The employee is reticent to report the claim due to concern of its impact on future workplace opportunities and treatment by employer and colleagues. Raising equity and fairness concerns. • A formal complaint could impact on the GP’s physical, mental, emotional wellbeing raising concerns of care and empathy for the GP. • There is potential impact on the practice reputation, prompting concerns for the welfare of all practice associates. |
• Provide support to the employee as they encourage the colleague to approach you for a confidential interview. • Having interviewed the colleague, consider all claims of workplace bullying as serious and take immediate action to investigate and resolve quickly and fairly while ensuring support for the colleague and the GP from appropriate individuals throughout the process. • Contact Professional Practice Indemnity Provider for advice. • Review/Develop a practice Code of Conduct that clearly details the policy regarding response to bullying claims. • Ensure all doctor and employees are aware of and have agreed to abide by the practice Code of Conduct • Nominate impartial individuals/parties to investigate the veracity of claim. • Manage the expectations of all parties, ensuring clear communication regarding the process for investigation, and potential actions in response to the findings. • Respond to the findings of the investigation in accordance with the practice Code of Conduct. • Provide and facilitate access to educational resources regarding bullying for practice associates. • Provide and facilitate access to wellbeing supports as required (e.g., the use of an Employee Assistance Program) • Take reasonable steps to ensure that if parties are required to work together that neither experiences difficulties at work as a result of any claim and subsequent process. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
|
A daughter was appointed as a power of attorney for her mother who suffered from dementia. Two other daughters came to speak to the Doctor concerned that the first daughter was not fit to have hold the power of attorney. They were wanting to access the mother’s funds and her daughter would refuse access as the costs were not related to the mother’s expenses. The daughter holding the power of attorney was not a regular patient of the practice, although the two daughters and their mother were long-term patients of the Doctor. |
• The Doctor had to decide where her alliance was regarding this request by the other two daughters. She had to process the principles of confidentiality and privacy while at the same time wishing to assist her patients, touching on principles of care and empathic understanding. • The principles of Justice also require consideration, as the mother could not make autonomous decisions. What is fair treatment for the mother in this context must be determined. |
• While the doctor might feel a great deal of sympathy and concern for her patients, any attempts to “do good” might cause ethical and legal complications and managed accordingly. • Recognising and honouring the complex boundaries between the doctor, the patients, and the third sister is critical to the doctor being able to resolve this ethical dilemma effectively • The outcome was that as legally the GP could not provide any assistance regarding her patients’ wish to access their mother’s funds, she informed the others of the limits of her professional responsibilities. The mother had granted power of attorney to the third daughter and that decision must be honoured. She suggested that the two patient/daughters could consider starting a discussion with their Solicitor. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| A long term elderly patient asks the Practice Manager to help them lodge a complaint about one of the doctors, who the patient claims has been rude to them. |
• Principles of care and empathic understanding are raised in this case. The patient will benefit from support while they explain their concerns. • Both the patient and the doctor are entitled to be treated fairly and impartially in regard to this dilemma. Even if the patient has proved to be difficult in the past, or if other patients have raised concerns, the matter cannot be prejudged in any way. |
• Providing the patient with the opportunity to explain her concerns and listening non-judgmentally might allow the Practice Manager to defuse the conflict and reassure the patient. • Documenting the specifics of the issues involved might provide clarity and options for resolving the patient’s concerns effectively without pursuing a formal complaint • Hearing the doctor’s side of the story might also shed valuable light on the matters at hand and assist the Practice Manager in any attempts to reconcile the differing perspectives. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| An elderly patient has contacted the practice, asking for a driving medical. A member of the family later contacts the practice to say the patient is “unfit to drive and the doctor needs to know that fact when assessing the relative”. |
• The patient is entitled to be treated fairly and impartially, as the principles of Justice would indicate. Providing the patient with the benefit of presumed capacity to drive, unless the evidence proves otherwise, is an essential aspect of this process. • The relative might have details regarding the patient’s driving history and any documentary evidence, such as facts of a recent accident, might be invaluable. The relative must therefore not be dismissed out of hand but given a chance to contribute to the process. • To ensure impartiality, the doctor has to assess the case on its merits and not be biased by the relative’s opinions. |
• The relative could be invited to submit any documentary evidence that might assist the doctor in her assessment of the patient. • The patient can be supported through the medical assessment process, to minimise any stress and the subsequent impact that might have on performance. • If the doctor has a Iong-standing relationship with the patient, there might be an unintentional bias towards assessing the patient favourably. Informing the doctor of the call from the relative and providing any documentation that the relative is able to provide can perhaps help ensure that the doctor is able to evaluate the patient’s performance more impartially. • The patient might react negatively to losing his licence and grieve the loss of independence. Appropriate referrals to support services might be an option worth exploring with the patient once the assessment is completed. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| One patient has offered a gift of more than minor value to staff at the practice. Initially, the patient gave a small bunch of flowers to the reception to thank them for being so helpful with changing the patient’s appointment times. Over time, this gesture grew to bouquets of flowers for the reception desk and a box of chocolates to be shared by the staff members. This time, the patient has suggested buying a few bottles of champagne for the annual break-up lunch |
• It might be helpful to establish the patient’s motivation for donating presents in this manner. Principles of care and empathic understanding come into focus here. A respectful, supportive conversation can help the Practice Manager understand the patient’s point of view more comprehensively. • Concerns regarding conflicts of interest for staff members are worth considering. While small gifts may seem harmless and a refusal might offend the patient, the Practice Manager has to be conscious of the ‘slippery slope’ that can arise from accepting gifts that cross the line and lead to boundary violations. The integrity of the Practice Manager could then come into question. • The wellbeing of the patient is an aspect to consider in this dilemma. Feeling obliged to keep giving better gifts could cause emotional or financial concerns. |
• Conducting a respectful and supportive conversation with the patient might assisting the Practice Manager in understanding the patient’s motivation and understanding of the issues involved. • Clear boundary setting and explicit statements regarding the acceptability of presents and gifts could help the patient understand why gift-giving in this context might not be as beneficial as perhaps intended. While the patient might be well-meaning, it is important to distinguish between doing good for others and such gestures having adverse consequences even if unintended. • Explaining the legal and ethical constraints that the practice would face if this gift was accepted. If done in a way that does not embarrass or shame the patient, it might open up opportunities for exploring other ways in which the patient can express gratitude to the staff without compromising their ethical and legal standards. |
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| An elderly doctor who has been a member of the practice for many years has been reported by several patients to be out of date and appearing senile during some consultations, forgetting details, and losing track of the conversation. The doctor has needed to retire for several years now but there is a shortage of doctors in this particular region of rural Australia |
• The primary ethical consideration in this scenario would be to ensure that no harms occur to patients. The risk of harm is unknown at present, although there is circumstantial evidence suggesting the doctor is creating a hazardous situation. • There is also risk of harm to the community, as the shortage of appropriate health care might be exacerbated if the doctor is prematurely prevented from practising. • The wellbeing of the doctor and of patients happy with their care are factors that need to be considered. Principles of care and empathic understanding can be invoked. |
A timely conversation with the doctor raising the concerns voiced by the patients in question and addressing the doctors’ capacity to practise at this time, could be initiated by the Practice Manager. • All or none solution might not be called for at this point. It might be appropriate, for example, to negotiate with the doctor about voluntarily adopting restrictions on limits to practice. The doctor might then find a valuable niche role within the practice that does not overly deplete its professional resources. • Organising, with the doctor’s cooperation, a comprehensive assessment of the doctor’s current capabilities would offer reassurance to the practice members that the doctor is not placing patients at risk. On the other hand, it can potentially open discussions for a more formal investigative process to commence.
|
| Initial Problem creating Ethical Concern | Clarifying The Ethical Considerations | Exploring Possible Strategies & Solutions |
|---|---|---|
| A doctor is refusing to see a patient who is an adult sex worker and there are no other suitable referrals that can be made for the patient. |
• It is possible that the doctor is refusing to see the patient because of their own moral concerns. Understanding the doctor’s point of view would benefit suitable management of this conflict, suggesting that Principles of care and empathic understanding are involved. • There might be other reasons why the doctor is refusing to treat the patient, and this possibility can be fruitfully explored in a frank and open discussion with the doctor. Principles of Justice and fairness also apply to the doctor, and need to be considered. • Ultimately, the patient has a right to be treated fairly, without moral judgement on the part of health care workers. This consideration has to be borne in mind throughout the process, as matters of justice and fairness for the patient do come into the equation. • There is also the aspect of health and welling of the community. Failing to treat this patient might potentially lead to increased prevalence of sexually transmitted infections in the community. Thus, questions of justice and fairness for others are also raised by the facts of this case. |
• Initiating a conversation with the doctor to establish more clearly the basis for their refusal to see this patient would be valuable. If the refusal is based on moral grounds such as religious values, then the process might involve inviting the doctor to consider the implications of their position on treatment options for these patients. • It might also be possible to explore other issues that could be affecting the doctor’s decision. For example, it might be worth considering the possibility that unconscious biases, e.g. based on gender, are at play here. • The doctor’s wellbeing also needs to be considered in any such conversations. They might be deeply distressed by having to confront difficult decisions of this sort, and appropriate support and understanding would be appropriate in such circumstances. • There is opportunity for creative problem-solving here and the answer might not be a single yes or no decision. For example, a solution might be as straightforward as a referral to another doctor in the practice who is prepared to take on the patient’s care. • It would be important not to neglect the patient in a scenario such as this. Depending on how the initial refusal was communicated to the patient, if it has been, they might be feeling shamed by the decision, or desperate to seek essential health treatment. If the patient is aware of the doctor’s initial position on providing treatment to them, an interview with the patient might help with short-term problem solving to ensure the health and wellbeing of the patient. |

Medical Administration Training. (n.d.). Roles and Responsibilities. https://mathealthclinic.com/wp-content/uploads/2019/05/roles-and-responsibilities-of-a-med-recept.pdf
RESPONSIBILITIES OF A MEDICAL RECEPTIONIST
A medical receptionist is an integral part of a healthcare team. Doctors, nurses and other medical and administrative staff members rely on the medical receptionist to create a friendly, welcoming and well-organised front office for patients.
As a medical receptionist, you will be responsible for optimising the patient’s satisfaction, keeping the reception and waiting areas running smoothly, maintaining the confidentiality of all doctor, staff and patient information and all administrative matters relating to patient records.
All workers, regardless of their field or profession, operate within a legal and ethical framework of some kind. This simply means that we all work within the boundaries defined by applicable laws and ethical standards.
Some legislation that guide practices within the medical industry include:
► The Privacy Act
► Australian Privacy Principles
► Anti-Discrimination legislation
► Freedom of Information Act
► Occupational Health and Safety Act
Legislation, privacy and confidentiality is an in depth subject. As part of this course you have been provided with an additional Legislation guide. Please take the time to read this document.
When you start a new position you will receive information on your own role within the practice and your responsibilities when it comes to handling patient’s confidential information. employees the desired outcomes of the organisation. They help employees understand their roles and responsibilities within the organization.
A key aspect of following procedures involves working within the scope of your role and responsibilities. It is vital therefore that you know what your job role entails.
If you are unsure of your role and/or your work instructions:
As an employee, it is your responsibility to ensure that you:
► Familiarise yourself with the organisation’s policies and procedures
► Learn about the role and job tasks
► Develop the competencies that are necessary to perform the role efficiently
► Work within the accepted code of conduct and follow applicable legislative requirements
All medical practices are expected to have written policies and procedures. The purpose of healthcare policy and procedures is to communicate to ► Seek regular support and supervision from your supervisor through supervisory sessions and bring any situations to the attention of your team leader
► Seek advice from work colleagues through consultation and staff meetings
► Seek to have your position description clarified and/or have it include reference to professional standards or legislative provisions
► Seek to have your competencies assessed and/or recognised
► Ensure that all major work activities are accurately documented/recorded
An example of a Quality Management Policy & Procedure Manual has been provided in your training materials, please take the time to view this document.
THE TEAM
There may be a team of people you work with on a daily basis depending on the size of the Practice. You may interact with the following people in your role:
► Practice Managers
► Doctors/General Practitioners
► Nurses
► Patients
► Supervisors and work colleagues
You will have a different working relationship with each of these groups.
A Practice Manager’s role can differ widely. Generally, a Practice Manager’s job involves implementing standard policies and procedures that keep the practice running smoothly while also responding to any unexpected issues that regularly crop up and supervising the administration staff.
The Doctor - One of the first and fast rules to learn is that a doctor’s time is valuable, don’t waste it. Finding a good time to ask the Doctor a question can be difficult as they are extremely busy and usually in with patients. Always check with your Practice Manager/supervisor on what the policy is regarding disturbing the Doctor. You will usually find if it is an emergency you can ask at any time even if there is a patient with the Doctor. If it is a question that can wait then find a time when the Doctor is between patients and ask then. Most practices have an internal messaging system which you can use to ask the Doctor questions.
Tip: If the Doctor comes out to speak to you and there are patients in the waiting room please use “Doctor” when you speak to them even if you call them by their first name in private. Calling them doctor shows respect in front of patients.
Not all practices have practice nurses. If your practice does have a nurse they can be a great help when you are not sure what to do. Usually the practice nurse will be in the treatment room but available if you need help with anything to do with patient wellbeing. They are also the person, other than the doctor, who is able to give patients their test results in some circumstances. Because you work in a medical environment, patients on the phone or in the waiting room may ask your opinion on what their symptoms mean, or what you think may be wrong with them. Doctors and nurses spend many years studying medicine so they can diagnose patients. They are also licensed to do so. You are not.
INDUCTION AND TRAINING
Being new to the industry you will no doubt have many questions, and possibly anxieties, about the role.
Information that relates to your job role may come from:
► Induction and training
► Position descriptions which describe in more detail your role, tasks, responsibilities, and your level of authority
► Workplace policies are clear, simple statements of how the practice intends to conduct its services.
► Workplace procedures may specify who in the organisation is responsible for particular tasks and activities, or how they should carry out their duties.
► Other relevant personnel such as co-workers, supervisors or the Practice Manager
► Performance reviews
Most practices have induction programs for new staff. The purpose of induction is to make you familiar with your workplace, the software applications you will be using, the duties you will carry out and the standards of work that are expected of them.
There are a wide range of software applications available to assist with maintaining patient bookings, medical billing and medical records.
Your induction should also cover the relevant legislations and requirements of the workplace and your role.
Training may also be provided throughout your employment, this is commonly referred to as professional development.
MONITOR YOUR ROLE
In any business, roles transform and a medical centre is no exception. As the practice grows your role may change so it is important you monitor your role and be aware of its limitations. You should self-manage and self-evaluate regularly. If need be, make changes to the way you perform your duties, or, in consultation with your supervisor, arrange to undertake some training either internally or externally in the area you feel you are lacking knowledge.
Take on board suggestions made by other team members that may make your role more efficient and effective. Consider making changes, amend your role accordingly, and conduct a self-audit to continually find a more effective way of operating. Try to identify gaps between how you are performing and what is expected of your role. This is known as ‘self-evaluation’. Most importantly, be flexible and be able to meet changes as they occur.
If you have any concerns about your role and how to perform it speak to the Practice Manager or your supervisor.
SKILLS OF A MEDICAL RECEPTIONIST
Medical receptionists need to have solid people and administrative skills to keep things flowing efficiently in the doctor’s office. To be successful in your role as a medical receptionist, you are expected to be compassionate, caring, professional and discrete with a high level of organisation skills. Attention to detail is a must as you will be dealing with sensitive and confidential information on a daily basis.
Regardless of whether you’re working in a general practice, medical or allied health clinic or hospital as a medical receptionist, you need to have excellent organisational skills, be able to effectively multi-task, have amazing time management and provide a high level of customer service.
“Listen to understand rather than listening to respond” EFFECTIVE COMMUNICATION
Communication skills are at the heart of this job role. First and foremost, the medical receptionist should have sharp listening abilities to find out what the patient needs and then help them.
Medical staff speak to people of varying educational, cultural and social backgrounds and must do so in an effective, caring and professional manner – especially when communicating with patients and their family.
Effective communication with patients ensures that:
► Patients can contact the practice when they need to
► Patients can make appointments and receive other information in a timely fashion
► Urgent enquiries are dealt with in a timely and medically appropriate way
► That the patient is happy with the customer service and will keep returning to the practice
Along with providing accurate information about the practice to patients, receptionists manage tricky calls, deal with difficult patients and send clear communication and messages to patients and other health providers either verbally or in writing via email or SMS.
Effective communication is an in depth subject. As part of this course you have been provided with an additional Communication Guide. Please take the time to read this document.
INTERPERSONAL SKILLS
Receptionists interact with a wide range of personality types in both pleasant and sometimes difficult circumstances. They should be friendly and confident but also be tactful and sympathetic.
Medical office front desk receptionists also interact frequently with medical professionals, supervisors and other staff members, so must be able to collaborate easily, give and receive criticism gracefully and rise above petty office politics. Good interpersonal skills go beyond basic communication abilities. Soft skills like friendliness and likability are especially important for the receptionist role.
EXCEPTIONAL TIME MANAGEMENT
Throughout each working day you will juggle a multitude of different tasks; managing the demands of taking calls, booking appointments, taking and relaying messages and still completing clerical tasks on time.
It calls for a high level of multi-tasking ability coupled with skills such as time management and the capability to prioritise duties. It is imperative that you are able to deal with stress while managing fast-paced office duties.
In medical reception jobs, time management is crucial for serving patients promptly and keeping them pacified even when it is busy.
Some simple time management techniques you can use are:
► Start your day with a clear focus
► Have a priority task list
► Focus on high-value activities
► Minimise interruptions
► Stop procrastinating
► Review your day
Time management requires a good sense of how things should flow so that you can correctly allocate the time needed for a task. But it's not just about scheduling. Good time management also requires discipline, quick thinking, knowing how and when to delegate, and knowing when to use strategies for dealing with procrastination, distraction, and even unplanned events.
ATTENTION TO DETAIL
To be a great receptionists, you need to be highly organised and detail oriented to ensure that daily administrative tasks don’t fall through the cracks. After all you need to keep yourself and possibly everyone else on track. You can find files and phone numbers at a moment’s notice, and maintain a tidy work area.
TECHNICAL RECEPTION SKILLS
As a front desk receptionists, you will mainly use telephones and computers to communicate with patients and staff so you must have basic keyboard knowledge.
The telephone system will probably feature multiple internal and external lines that must be kept operating smoothly. You’ll also most likely need to be familiar with word-processing software packages. Any receptionist should be comfortable using phone systems, copiers and printers.
INDUSTRY KNOWLEDGE
There’s no doubt that working in a medical practice, allied health centre or hospital, medical receptionists need a basic understanding of the industry and industry-specific software programs. In general, you should be well versed with medical terminology, privacy legislation and medical billing.
MAKE A DIFFERENCE
Receptionist roles are extremely important to the efficient running of a medical clinic. Whether by telephone or in person you will be the first point of contact a patient usually has with the practice.
Your approach as the receptionist to professionalism and sense of empathy can greatly impact how the patient feels and whether they return to the practice.
You can make a real difference to the patient experience by:
► Using manners
► Being respectful
► Demonstrating Integrity
► Showing empathy
MANNERS
Most people learn the magic words "please" and "thank you" at a very early age and basic manners are essential when communicating with patients. However learning the skill of being polite and diplomatic in your speech enables you to establish habits in good manners.
When speaking to patients at the practice either at the front desk or on the telephone, a different set of phrasing is used instead of our everyday phrases. Using a more professional group of phrasing portrays to the patient a sense of confidence and a sense that you are there to help them. Using phrases such as “Could you”, “May I?”, “Please”, and “Thank you” can help the person standing in front of you or on the other end of the phone line feel more comfortable and feel more at ease with your politeness. Some of the phrasing can seem uncomfortable at first, but with practice, can become as natural as our everyday speech.
Some examples of this are:
Don’t say: “Can I help you” Instead say: “How may I help you?” Don’t say: “Can you repeat that name?” Instead say: “Could you repeat that name again, please?” Don’t say: “Can I take a message?” Instead say: “May I take a message?”
RESPECT
Respect is more than just good manners. In order to receive respect, you first have to display respect. And if you want others to know that you are capable, and passionate about providing quality care, you have to convey that message.
You can demonstrate respect to patients and work colleagues with simple, yet powerful, actions like using a person's name, making eye contact, and actively listening when a person speaks to you.
Treat others the way you would like to be treated and treat all people the same nomatter their race, religion, gender, size or age.
Never insult people, use name calling, or put down people or their ideas.
Don’t be distracted by things going on around you and stay focused on conversations.
You should always treat patients, other employees and doctors with respect regardless of beliefs or backgrounds or what differences of opinion you may have. This will ensure you work in a harmonious environment, which in turn will ensure you are offering quality care and treatment to patients.
INTEGRITY
Integrity is the defined as being honest and having strong moral principles.
When working in the medical environment it is of the utmost importance that you always behave with honesty and integrity and consistently apply the values of the practice and act in accordance with social standards or moral values of society.
Most companies have detailed employee handbooks that outline both acceptable and unacceptable workplace behaviours. This handbook usually includes things such as improper use of the companies’ property, phone and internet. Social media policies to inform employees of unacceptable behaviour when participating in the social media space, bullying and anti-discrimination etc.
In a health setting environment a strong focus is placed on privacy and patient confidentiality. The practice may have a Code of Conduct/Code of Ethics outlining the ethical obligations for administrative staff. For example, the Code may state that the administrative staff shall not reveal confidential communications or health information without permission. It may also state that no patient matter shall be discussed outside of the practice.
Simple ways to demonstrate honesty and integrity in your role:
► Follow workplace policies and procedures
► Be aware of legislation relating to your industry and role
► Take responsibility
► Keep your word
► Keep your commitments
► Respect your employer, patients and other co-workers
What is the difference between Empathy and Sympathy?
Empathy is a learned response. It is different than sympathy, as you are actually placing yourself in the other person's situation versus feeling sorry for them.
Sympathy is a shared feeling, usually of sorrow, pity or compassion for another person. You show concern for another person when you feel sympathy for them.
For example, when someone loses a loved one, you feel sympathy towards that person and their family. You may share a feeling of sadness with them, but you might not have empathy for their situation if you have not experienced, or cannot imagine experiencing, a death in the family.
Empathy is stronger than sympathy. It is the ability to put yourself in the place of another and understand someone else's feelings by identifying with them. With empathy, you put yourself in another's shoes, often feeling things more deeply than if you just felt sympathy.
For example, someone lacking empathy may not be able to understand why another person is upset over a situation if they cannot imagine themselves in that person's place. Someone has empathy if they can put themselves in the same situation and perceive how the other person is feeling, even if they do not share those experiences.
DEALING WITH DIFFICULT PATIENTS
Most patients will be pleasant and easy to deal with however some patients may be responding badly due to the following:
► Because they are feeling really unwell
► Because they are tired
► Because they are anxious
► Because they are under the influence of alcohol or drugs
► Because they are upset
► Because they are depressed
► Because they have been waiting a long time with no explanation
► Or maybe they are just difficult by nature
Give them a chance to tell you what the problem is and listen without interrupting. When they tell you the problem, try and find a solution and communicate with them. If you need to explain something don’t go into long explanations. Be as brief as you can but still address the issue.
If possible, remove the patient from the waiting room and their “audience”. Sometimes this can calm the situation. Ask a colleague for help if you are starting to feel bullied and need some support.
Some patients we just can’t get along with or maybe we are having an off day. Even without difficult patients, dealing with sick people on a daily basis is hard work and not everyone understands this. Try and have a group of people around you who can support you.
The practice should have a policy for dealing with difficult patients which may include the following:
► Be well prepared – be aware of the patient’s history and also practice procedures
► Put things into perspective – don’t make things bigger than they are
► Trust your knowledge, experience and intuition – this will demonstrate confidence and keep you calm ► Plan your responses – based on practice procedures
► Prevent stressful situation – recognise there may be an issue and intervene sooner rather than later when the situation may have escalated
► Have a supportive staff environment
► Manage the stress – debrief in a supportive environment
Keep the Reception and Waiting Ares Clean and Tidy
Having a clean and tidy reception and waiting area will give your patients a great first impression. However more importantly, a clean medical office is essential in keeping employees and patients safe and healthy. Keeping the medical office free from germs is more than what can be found on the surface; it’s about having a space that is free from infectious disease.
How to keep yourself and others healthy in a medical practice:
► Hand washing
► Keeping high touch areas clean
► Use gloves when cleaning and accepting patient specimens
► Disinfecting toys etc. in the waiting room
► Keep tissues and hand sanitizer available for use of both staff and patients
► If you are unwell stay home
How to keep yourself and others safe in a medical practice:
► Check for any hazards in the practice
► Report anything potentially dangerous at work of which you become aware of to your employer DUTIES OF A MEDICAL RECEPTIONIST
The reception desk of a medical office can be a very busy place and is essential for the smooth operations of the medical office. Health administration duties can vary from workplace to workplace but generally speaking, medical receptionists may:
1. Keep the reception and waiting area clean and tidy
2. Greet patients
3. Answer and manage the telephone
4. Schedule appointments
5. Register new patients
6. Facilitate patient flow
7. Issue patient accounts
8. Handle inter-office communication and external correspondence
9. Maintain stocks of stationery and medical supplies
GREETING PATIENTS
The medical receptionist welcomes and greets patients and visitors, in person and over the phone. The first impression that a receptionist gives will be lasting. It is crucial that in all circumstances you provide high-quality customer service, be professional and that you are genuinely warm and welcoming.
Tips for greeting patients
► When a patient walks in the door, if possible stand up to greet them. It’s the courteous thing to do, it demonstrates an interest in them, and makes them feel important.
► Greet him/her by wishing him/her 'Good morning or afternoon' in a cheerful tone. This creates a pleasant feeling. However care should be taken that the greeting does not sound forced, dull or bored, as it then completely loses its impact.
► Always get permission before you call any patient by their first name especially elderly patients. Don’t address patients as love, or dear. Always use their correct title.
► Once you’ve made the patient feel welcome, ask them for anything you may need such as a Medicare or pension card, Let them know where toilet and other facilities are located if required and ask them to take a seat.
► Keep patients calm and informed. If the doctor is running late, let them know and offer alternatives such as another appointment time or ask them if they would like to go and get a coffee and you will message them when doctor is almost ready.
► Be aware your conversations can quite often be heard by those sitting in the waiting room so always be careful with your conversation and also your facial expression. Waiting patients hear and see everything.
Greeting a patient professionally can get a little tricky when the practice is busy. Let’s look at a couple of scenario’s and how to handle them:
► You are on the phone and a patient is waiting at the front desk - what do you do? – Make eye contact with the patient, smile and indicate for them to take a seat then when you are finished go and greet them and ask them to come to the desk so you can check their details and indicate they have arrived.
► A patient does not approach the desk they walk in and sit straight down – Go and ask the patient if they are seeing a doctor and could they please come with you to the reception desk so you can check their details. This sometimes happens with patients who are regular visitors to the practice. However, it is always wise to check they actually do have an appointment and then ask them gently if they could come to the desk so you can check them in.
► You have another patient’s file in view, what do you do? – If it is a paper file, quickly close it and position it so no information including the patient name can be seen. If it is on the computer screen, make sure you can switch to the screen saver quickly to protect the patient’s privacy. Never leave a patient’s notes open on the computer if you are leaving your desk.
ANSWERING THE TELEPHONE
As a medical receptionist, having excellent etiquette is a must!
Having a good telephone manner is sometimes seen to be a simple task however there is a lot that goes into having a professional telephone manner. One recurring theme within the medical reception field is ‘treat others how you would like to be treated’. It is important that medical administration staff are consistently polite and professional. When a patient calls the medical practice, the way in which the front desk personnel handles the telephone call will determine how the practice is perceived.
As the primary means of communication, telephone communication should not be taken lightly. Here are some tips to assist you in improving your telephone etiquette:
LEARN TO LISTEN PROPERLY
You may have heard of a technique called “Active listening”. This means listening with the intent to understand completely and allowing the patient to finish speaking without interruptions. Focusing on what the patients’ needs are by paying close attention to what they are saying, asking clarifying questions and repeating what the person has said. In this technique, the listener will rephrase the information they heard in their own words. If this information is correct, the exchange is complete, if not the sender of the information can correct any misunderstandings at this time. Our tips:
► Focus on the person speaking
► Be curious
► Don’t interrupt
► Consider your non-verbal communication
► Avoid talking to anyone else
► Keep your mind focused on the issue being discussed
BE PROFESSIONAL AND COURTEOUS
Having a good phone manner can come down to two things, being professional and being treated the way you would want to be treated if you were the patient. If the call is answered in a pleasant manner, with an introduction, this sets the tone for the conversation. Here are some tips on how to be professional and courteous while on the telephone:
► Answer quickly, at least by the third ring
► Answer with your name and the name of the medical practice
► Smile, the caller can hear your smile through the phone
► Speak slowly and clearly
► Never chew food, gum or drink anything while on the phone
► Ask permission before placing a caller on hold
► Emphasise what you can do rather than what you can’t do
MAINTAIN CONFIDENTIALITY
Maintaining patient confidentiality not only makes patients feel secure about being treated at your medical facility, it is also the law. You are required to comply with the relevant State / Territory and Federal laws relating to the collection, storage, use, disclosure and disposal of patient records. It is imperative that medical records remain confidential and cannot be accessed by people that do not have proper authorisation. Here are some tips on how to maintain patient privacy:
► Confirm the identity of the patient prior to any information being given over the phone or in person
► Keep in mind other patients may be able to hear your conversation
► If the caller is not the patient, never discuss personal information without permission
THINGS TO CONSIDER
Speaking on the phone isn’t always what you say or what you do, it is also how you sat it and how you do it. Consider these the next time you talk to a patient or other customer on the telephone:
► Always thank them for calling
► Never be the first to hang up
► When receiving a call, take as much detail as possible. If you need to transfer a call it makes it easier and more professional to not have to ask ‘sorry, what was your name again?’
► Stay calm and polite, even when a patient is rude to you
► Important: Before putting a caller on hold, reception staff must first ask if the matter is an emergency
REGISTERING NEW PATIENTS
Creating new patient records and updating existing patient records is one of the most important duties of a medical receptionist. These details provide a benchmark for cross checking a patients identity on return visits, provides information on the patient demographics and insurance information. Invalid information can not only delay payments from Medicare / Health Funds but also has the potential to become very problematic if a patient’s identity can’t be verified on a return visit. A new patient will be required to fill-out and sign a patient registration form. Information required to create a patient record includes but is not limited to:
► Patient’s name, address, phone and email contact details
► Sex, age, birthday and race (ethnicity)
► In case of emergency contact information
► Medicare number
► Private Health insurance information
► Concessions, e.g. healthcare card
► Existing medical conditions/known allergies
If you are working in a computerised practice, you enter all the patient’s details in the ‘create new patient’ section of the program. The computer will then generate every component of the file it needs from this one entry.
You may be required to make a small paper file which will hold all patient’s correspondence e.g. registration form, medical reports, pathology results etc. If you are working with a manual system it will depend on your practice policy and procedures as well as relevant regulations as to how these files will be constructed.
If your system is fully computerised all registration forms, referral letters etc. will be scanned into the patients computerised file. All details of rebates and entitlements patients receive will be built into the software system for ease when processing accounts as well as acting as a database for all patient information. Click to view a short video View a demonstration here: https://mathealthclinic.com/medicalreception-webinars/
SCHEDULING APPOINTMENTS
Nothing is more frustrating for a patient than having to wait for longer periods than expected. Effective scheduling is a necessity for any practice in order to provide an excellent patient experience. Most practices will use some form of scheduling software that makes the scheduling process easier. However, when cancellations and no-shows arise, it becomes imperative that the front desk staff are able to communicate the changes in schedule to both the patients and the physicians.
When making appointments it is important to ensure you get as much detail as possible. There are three pieces of vital information required:
► Name of the patient
► Contact phone number
► Appointment type: is it a normal appointment or are they seeing the doctor for multiple issues which would mean a longer appointment
Practice administration staff must be aware of the procedures that apply to scheduling appointments. For example, they must know what the priorities are in regards to timing and duration of appointments, dealing with requests for emergency appointments and changing appointment times. Different types of medical appointments include initial, standard or long appointments and standard times and costs for each of these will be specified. For example:
Consultation Type Item Number Medicare Schedule Fee
Normal (Level B) lasting less than 20 minutes 23 $37.60
Long (Level C) 20-40 minutes 36 $72.80
Prolonged (Level D) more than 40 minutes 44 $107.15
What is Triage?
Triage is a skill used to prioritise the needs of the patient. Urgent cases should get priority. Triage is a way patients are prioritised when they ring for an appointment or come into the practice wanting to see a doctor.
Why is triage important?
Triage enables the practice to see patients in order of priority and helps with the smooth running of the practice. It is important that everyone in the practice is familiar with the triage policy of the practice.
Triaging isn’t something to be afraid of. You are actually triaging every time you make an appointment for a patient. You will have a series of questions you ask when a patient calls or presents to the practice so you can allocate the appropriate time for that patient. Triage is not only for emergency situations.
Learning how to triage is a skill that you will develop over time and with instruction. The appointment system should always allow for urgent appointments. The practice will have a way these appointments are identified so they can easily be recognised as a priority. There are some simple tools to help all receptionists triage or prioritise patient appointments.
There should be a triage poster at reception for staff to refer to and also a procedure to follow. http://www.ruralhealthwest.com.au/docs/d efaultsource/workforce_support/ecopy_resourc es_front-desk-triage-poster.pdf?sfvrsn=2
When making appointments, it is important to ensure you get as much detail as possible. This will help make sure the practice runs smoothly and on time, providing there are no emergencies. When a person calls to make an appointment always try to find out what sort of appointment it is. Is it a normal appointment, or are they seeing the doctor for multiple issues which would mean a long appointment needs to be booked? The more information you can obtain from the patient the better.
No-shows, changing appointments and cancellations
Occasionally, a patient does not arrive for a scheduled appointment. This is referred to as a no-show. Usually patients are not billed for a ‘no show’ however some practices may have a policy of charging for appointments where patients continue to not attend their scheduled appointment.
Appointments will often be changed either by patient’s or by the medical practitioners, so the appointment system needs to be adaptable and flexible. Changes and cancellations can be frustrating but unavoidable.
Some medical clinics may confirm patient appointments either by having the receptionist call in advance or be using SMS messaging via the practice software.
Even if practices have clear-cut policies on handling no-show patients, dealing with late patients — especially those who are regularly late to appointments — is another issue altogether.
It's important to try and get the patient in to see someone if possible, such as another doctor. If their doctor can accommodate them at a later time let them know they will either have to wait or make another appointment. Some patients have no sense of time or are just inconsiderate and are always late. Explain to the patient it is not acceptable to be constantly late and discuss some strategies to help the patient be on time. View a demonstration here: https://mathealthclinic.com/medicalreception-webinars/
Facilitating patient flow
Notifying the medical practitioners of patient’s arrival, being aware of any delays and communicating with patients and clinic staff all form part of managing the patient flow. If the patients are not happy with the entire process, they may not come back. Providing high-quality care and excellent customer service will all form part of the decision for a patient to remain with the practice or look elsewhere for their medical needs. Patients will very likely continue to come back if they are satisfied with the entire process.
There's no way the practice can run on time, all the time. But there are some ways to ease patient frustrations when you do run behind schedule.
► Anticipate. Take steps to reduce the number of patient complaints that occur by being open and honest with patients regarding long wait times. Explain delays, and ask patients if you can do anything to make them more comfortable while they wait.
► Take the blame. When complaints do crop up, remember the three "A's”: agree, apologise and acknowledge. By acknowledging and apologising, you're reducing the risk of escalation of the complaint.
► Take it elsewhere. If a patient complaint begins to escalate and the patient becomes extremely upset, loud, or unruly, act quickly and privately. If possible and safe for you to do so, move them out of the [reception] room.
Once you find a quiet and safe place to speak with the patient, Say something like, "I see how upset you are and I am very sorry. How can I help?"
If you’re referring a patient to a specialist service, you need to include the following referral information on the account and/or receipt:
► the name of the referring practitioner
► the address or provider number of the referring practitioner
► the date on which the patient was referred
► the period of the validity of the referral - where this is for other than for 12 months, this should be expressed in months, for example 3, 6 or 18 months, or indefinitely
Medical practitioners are free to set their fees for their professional service. However, the amount specified in the patient's account must be the amount charged for the service specified. The fee may not include a cost of goods or services (GST) which are not part of the MBS service specified on the account. There are a variety of ways to bill a patient
► where the practice bulk bills, no account is issued to the patient
► where bulk billing does not occur an itemised account will be given directly to the patient. Many doctors now offer payment and benefit claim via the Medicare Easyclaim system. This allows the patient to claim the Medicare rebate when they pay the account at the doctor's surgery. If the doctor uses the EFTPOS system the rebate is paid into the patients nominated account almost immediately. View demonstration here: https://mathealthclinic.com/medical -reception-webinars/
Electronically generated accounts
A software system is generally used for generating accounts. Medical administrative staff would be trained to use the software package. View a demonstration here: https://mathealthclinic.com/medicalreception-webinars/
Interoffice Communication
The medical office front desk is a hub of communication. To ensure that things run smoothly, it is important that information is clear and concise. Whether in memo, written communication, through inter office email, one on one interaction or in a group setting it is vital that you stay on topic and don’t stray off point. Being organised will go a long way to ensure that inter office communication is effective.
External Correspondence
External communication refers to any communication you have with other practices, insurance companies, Medicare and other businesses. This may require making phone calls, emails, professional letters, faxing etc. so it is essential that you know how to formulate a professional letter and be able to adequately operate office equipment.
Maintaining Stocks of Stationery and Medical Supplies
Adequately stocking by anticipating inventory needs, placing orders and monitoring office equipment and supplies is vital to the smooth running of any office but in particular a medical practice.
The final point to remember is when you work in the medical environment you must abide by strict security procedures/policies in regards to storing drugs and medical equipment.
These must always be stored according to the policy & procedures of the practice. This will take into account any OH&S issues and legislation regarding the storage of drugs, poisons and controlled substances. Secure storage of medication and medical equipment is essential to ensure the safety and welfare of patients and other people who visit the medical practice.
Your organisation will have strict procedures for storing supplies, in particular medicines, narcotics, refrigerated items, sterile stock, syringes and any items that must be stored away from light.
The practice manager or nurse will be responsible for the handling of some of these items. However, all staff should be aware of storage procedures and guidelines can be found in the practice policy and procedure manual.
Some of the guidelines for storing drugs and equipment are:
► Prescription stationery should be stored out of sight and in a lockable cabinet where only authorised personnel have access
► Schedule 8 poisons (labelled controlled drugs) should be stored in a locked facility, fixed to the floor or wall and it must provide no less than a 10mm thick mild steel drug cabinet. No other items must be stored with them
► Schedule 4 poisons (prescription only medicines) must be kept in a lockable storage facility
► Schedule 2 & 3 poisons (pharmacy medicine or pharmacist only medicine) be stored in the same manner to Schedule 4 poisons
► Vaccines that require refrigeration be secured in a lockable container within a refrigerator or a lockable refrigerator.
► Only people authorised should have access to the storage facilities
► Drug registers and transaction records need to be kept
Specialised storage requirements might refer to:
► Controlling storage environments, cleaning, labelling and securing stock
► Waste management of infectious or dangerous materials
► Record keeping procedures.
All drug storage procedures will be documented in the practice policy and procedures manual. These procedures have been documented following legislative guidelines and acts. If you are ever unsure of what to do you should always refer to this manual or to a senior staff member.

United Nations. (n.d.). Universal declaration of human rights. Retrieved June 2, 2023
Preamble
Whereas recognition of the inherent dignity and of the equal and inalienable rights of all members of the human family is the foundation of freedom, justice and peace in the world,
Whereas disregard and contempt for human rights have resulted in barbarous acts which have outraged the conscience of mankind, and the advent of a world in which human beings shall enjoy freedom of speech and belief and freedom from fear and want has been proclaimed as the highest aspiration of the common people,
Whereas it is essential, if man is not to be compelled to have recourse, as a last resort, to rebellion against tyranny and oppression, that human rights should be protected by the rule of law,
Whereas it is essential to promote the development of friendly relations between nations,
Whereas the peoples of the United Nations have in the Charter reaffirmed their faith in fundamental human rights, in the dignity and worth of the human person and in the equal rights of men and women and have determined to promote social progress and better standards of life in larger freedom,
Whereas Member States have pledged themselves to achieve, in cooperation with the United Nations, the promotion of universal respect for and observance of human rights and fundamental freedoms,
Whereas a common understanding of these rights and freedoms is of the greatest importance for the full realization of this pledge,
Now, therefore,
The General Assembly,
Proclaims this Universal Declaration of Human Rights as a common standard of achievement for all peoples and all nations, to the end that every individual and every organ of society, keeping this Declaration constantly in mind, shall strive by teaching and education to promote respect for these rights and freedoms and by progressive measures, national and international, to secure their universal and effective recognition and observance, both among the peoples of Member States themselves and among the peoples of territories under their jurisdiction.
Article 1
All human beings are born free and equal in dignity and rights. They are endowed with reason and conscience and should act towards one another in a spirit of brotherhood.
Article 2
Everyone is entitled to all the rights and freedoms set forth in this Declaration, without distinction of any kind, such as race, colour, sex, language, religion, political or other opinion, national or social origin, property, birth or other status. Furthermore, no distinction shall be made on the basis of the political, jurisdictional or international status of the country or territory to which a person belongs, whether it be independent, trust, non-self-governing or under any other limitation of sovereignty.
Article 3
Everyone has the right to life, liberty and security of person.
Article 4
No one shall be held in slavery or servitude; slavery and the slave trade shall be prohibited in all their forms.
Article 5
No one shall be subjected to torture or to cruel, inhuman or degrading treatment or punishment.
Article 6
Everyone has the right to recognition everywhere as a person before the law.
Article 7
All are equal before the law and are entitled without any discrimination to equal protection of the law. All are entitled to equal protection against any discrimination in violation of this Declaration and against any incitement to such discrimination.
Article 8
Everyone has the right to an effective remedy by the competent national tribunals for acts violating the fundamental rights granted him by the constitution or by law.
Article 9
No one shall be subjected to arbitrary arrest, detention or exile.
Article 10
Everyone is entitled in full equality to a fair and public hearing by an independent and impartial tribunal, in the determination of his rights and obligations and of any criminal charge against him.
Article 11
- Everyone charged with a penal offence has the right to be presumed innocent until proved guilty according to law in a public trial at which he has had all the guarantees necessary for his defence.
- No one shall be held guilty of any penal offence on account of any act or omission which did not constitute a penal offence, under national or international law, at the time when it was committed. Nor shall a heavier penalty be imposed than the one that was applicable at the time the penal offence was committed.
Article 12
No one shall be subjected to arbitrary interference with his privacy, family, home or correspondence, nor to attacks upon his honour and reputation. Everyone has the right to the protection of the law against such interference or attacks.
Article 13
- Everyone has the right to freedom of movement and residence within the borders of each State.
- Everyone has the right to leave any country, including his own, and to return to his country.
Article 14
- Everyone has the right to seek and to enjoy in other countries asylum from persecution.
- This right may not be invoked in the case of prosecutions genuinely arising from non-political crimes or from acts contrary to the purposes and principles of the United Nations.
Article 15
- Everyone has the right to a nationality.
- No one shall be arbitrarily deprived of his nationality nor denied the right to change his nationality.
Article 16
- Men and women of full age, without any limitation due to race, nationality or religion, have the right to marry and to found a family. They are entitled to equal rights as to marriage, during marriage and at its dissolution.
- Marriage shall be entered into only with the free and full consent of the intending spouses.
- The family is the natural and fundamental group unit of society and is entitled to protection by society and the State.
Article 17
- Everyone has the right to own property alone as well as in association with others.
- No one shall be arbitrarily deprived of his property.
Article 18
Everyone has the right to freedom of thought, conscience and religion; this right includes freedom to change his religion or belief, and freedom, either alone or in community with others and in public or private, to manifest his religion or belief in teaching, practice, worship and observance.
Article 19
Everyone has the right to freedom of opinion and expression; this right includes freedom to hold opinions without interference and to seek, receive and impart information and ideas through any media and regardless of frontiers.
Article 20
- Everyone has the right to freedom of peaceful assembly and association.
- No one may be compelled to belong to an association.
Article 21
- Everyone has the right to take part in the government of his country, directly or through freely chosen representatives.
- Everyone has the right to equal access to public service in his country.
- The will of the people shall be the basis of the authority of government; this will shall be expressed in periodic and genuine elections which shall be by universal and equal suffrage and shall be held by secret vote or by equivalent free voting procedures.
Article 22
Everyone, as a member of society, has the right to social security and is entitled to realization, through national effort and international co-operation and in accordance with the organization and resources of each State, of the economic, social and cultural rights indispensable for his dignity and the free development of his personality.
Article 23
- Everyone has the right to work, to free choice of employment, to just and favourable conditions of work and to protection against unemployment.
- Everyone, without any discrimination, has the right to equal pay for equal work.
- Everyone who works has the right to just and favourable remuneration ensuring for himself and his family an existence worthy of human dignity, and supplemented, if necessary, by other means of social protection.
- Everyone has the right to form and to join trade unions for the protection of his interests.
Article 24
Everyone has the right to rest and leisure, including reasonable limitation of working hours and periodic holidays with pay.
Article 25
- Everyone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services, and the right to security in the event of unemployment, sickness, disability, widowhood, old age or other lack of livelihood in circumstances beyond his control.
- Motherhood and childhood are entitled to special care and assistance. All children, whether born in or out of wedlock, shall enjoy the same social protection.
Article 26
- Everyone has the right to education. Education shall be free, at least in the elementary and fundamental stages. Elementary education shall be compulsory. Technical and professional education shall be made generally available and higher education shall be equally accessible to all on the basis of merit.
- Education shall be directed to the full development of the human personality and to the strengthening of respect for human rights and fundamental freedoms. It shall promote understanding, tolerance and friendship among all nations, racial or religious groups, and shall further the activities of the United Nations for the maintenance of peace.
- Parents have a prior right to choose the kind of education that shall be given to their children.
Article 27
- Everyone has the right freely to participate in the cultural life of the community, to enjoy the arts and to share in scientific advancement and its benefits.
- Everyone has the right to the protection of the moral and material interests resulting from any scientific, literary or artistic production of which he is the author.
Article 28
Everyone is entitled to a social and international order in which the rights and freedoms set forth in this Declaration can be fully realized.
Article 29
- Everyone has duties to the community in which alone the free and full development of his personality is possible.
- In the exercise of his rights and freedoms, everyone shall be subject only to such limitations as are determined by law solely for the purpose of securing due recognition and respect for the rights and freedoms of others and of meeting the just requirements of morality, public order and the general welfare in a democratic society.
- These rights and freedoms may in no case be exercised contrary to the purposes and principles of the United Nations.
Article 30
Nothing in this Declaration may be interpreted as implying for any State, group or person any right to engage in any activity or to perform any act aimed at the destruction of any of the rights and freedoms set forth herein.

Australian Human Rights Commission. (2014.). A quick guide to Australian discrimination laws.
Over the past 30 years the Commonwealth Government and the state and territory governments have introduced laws to help protect people from discrimination and harassment. The following laws operate at a federal level and the Australian Human Rights Commission has statutory responsibilities under them:
- Age Discrimination Act 2004
- Australian Human Rights Commission Act 1986
- Disability Discrimination Act 1992
- Racial Discrimination Act 1975
- Sex Discrimination Act 1984.
The following laws operate at a state and territory level, with state and territory equal opportunity and antidiscrimination agencies having statutory responsibilities under them:
- Australian Capital Territory – Discrimination Act 1991
- New South Wales – Anti-Discrimination Act 1977
- Northern Territory – Anti-Discrimination Act 1996
- Queensland – Anti-Discrimination Act 1991
- South Australia – Equal Opportunity Act 1984
- Tasmania – Anti-Discrimination Act 1998
- Victoria – Equal Opportunity Act 2010
- Western Australia – Equal Opportunity Act 1984.
Commonwealth laws and the state/territory laws generally overlap and prohibit the same type of discrimination. As both state/territory laws and Commonwealth laws apply, you must comply with both. Unfortunately, the laws apply in slightly different ways and there are some gaps in the protection that is offered between different states and territories and at a Commonwealth level. To work out your obligations you will need to check the Commonwealth legislation and the state or territory legislation in each state in which you operate.
You will also need to check the exemptions and exceptions in both the Commonwealth and state/territory legislation as an exemption or exception under one Act will not mean you are exempt under the other.
For example, see the attached schedule of coverage.
See the tables below for detailed information on each federal, state and territory Act.
Further information
Australian Human Rights Commission
Level 3, 175 Pitt Street
SYDNEY NSW 2000
GPO Box 5218
SYDNEY NSW 2001
Telephone: (02) 9284 9600
National Information Service: 1300 656 419
TTY: 1800 620 241
Email: infoservice@humanrights.gov.au
Website: www.humanrights.gov.au/employers
These documents provide general information only on the subject matter covered. It is not intended, nor should it be relied on, as a substitute for legal or other professional advice. If required, it is recommended that the reader obtain independent legal advice. The information contained in these documents may be amended from time to time.
Revised November 2014.
Federal Laws
| Legislation and grounds of discrimination | Areas covered |
|---|---|
|
Australian Human Rights Commission Act 1986 Discrimination on the basis of race, colour, sex, religion, political opinion, national extraction, social origin, age, medical record, criminal record, marital or relationship status, impairment, mental, intellectual or psychiatric disability, physical disability, nationality, sexual orientation, and trade union activity. Also covers discrimination on the basis of the imputation of one of the above grounds. |
Discrimination in employment or occupation. |
|
Age Discrimination Act 2004 Discrimination on the basis of age – protects both younger and older Australians. Also includes discrimination on the basis of age-specific characteristics or characteristics that are generally imputed to a person of a particular age. |
Discrimination in employment, education, access to premises, provision of goods, services and facilities, accommodation, disposal of land, administration of Commonwealth laws and programs, and requests for information. |
|
Disability Discrimination Act 1992 Discrimination on the basis of physical, intellectual, psychiatric, sensory, neurological or learning disability, physical disfigurement, disorder, illness or disease that affects thought processes, perception of reality, emotions or judgement, or results in disturbed behaviour, and presence in body of organisms causing or capable of causing disease or illness (eg, HIV virus). Also covers discrimination involving harassment in employment, education or the provision of goods and services. |
Discrimination in employment, education, access to premises, provision of goods, services and facilities, accommodation, disposal of land, activities of clubs, sport, and administration of Commonwealth laws and programs. |
|
Racial Discrimination Act 1975 Discrimination on the basis of race, colour, descent or national or ethnic origin and in some circumstances, immigrant status. Racial hatred, defined as a public act/s likely to offend, insult, humiliate or intimidate on the basis of race, is also prohibited under this Act unless an exemption applies. |
Discrimination in all areas of public life including employment, provision of goods and services, right to join trade unions, access to places and facilities, land, housing and other accommodation, and advertisements. |
|
Sex Discrimination Act 1984 Discrimination on the basis of sex, marital or relationship status, pregnancy or potential pregnancy, breastfeeding, family responsibilities, sexual orientation, gender identity, and intersex status. Sexual harassment is also prohibited under this Act. |
Discrimination in employment, including discrimination against commission agents and contract workers, partnerships, qualifying bodies, registered organisations, employment agencies, education, provision of goods, services and facilities, accommodation, disposal of land, clubs, administration of Commonwealth laws and programs, and superannuation. |
|
Fair Work Act 2009 Discrimination on the basis of race, colour, sex, sexual orientation, age, physical or mental disability, marital status, family or carer responsibilities, pregnancy, religion, political opinion, national extraction, and social origin. |
Discrimination, via adverse action, in employment including dismissing an employee, not giving an employee legal entitlements such as pay or leave, changing an employee’s job to their disadvantage, treating an employee differently than others, not hiring someone, or offering a potential employee different (and unfair) terms and conditions for the job compared to other employees. |
State and Territory Laws
| Legislation and grounds of discrimination | Areas covered |
|---|---|
|
Australian Capital Territory: Discrimination Act 1991 (ACT) Discrimination on the basis of sex, sexuality, gender identity, relationship status, status as a parent or carer, pregnancy, breastfeeding, race, religious or political conviction, disability, including aid of assistance animal, industrial activity, age, profession, trade, occupation or calling, spent conviction, and association (as a relative or otherwise) with a person who has one of the above attributes. Sexual harassment and vilification on the basis of race, sexuality, gender identity or HIV/AIDS status are also prohibited under this Act. |
Discrimination in employment, including discrimination against commission agents and contract workers, partnerships, professional or trade organisations, qualifying bodies, employment agencies, education, access to premises, provision of goods, services or facilities, accommodation, clubs, and requests for information. |
|
New South Wales: Anti-Discrimination Act 1977 (NSW) Discrimination on the basis of race, including colour, nationality, descent and ethnic, ethno-religious or national origin, sex, including pregnancy and breastfeeding, marital or domestic status, disability, homosexuality, age, transgender status, and carer responsibilities. Sexual harassment and vilification on the basis of race, homosexuality, transgender status or HIV/AIDS status are also prohibited under this Act. |
Discrimination in employment, including discrimination against commission agents and contract workers, partnerships, industrial organisations, qualifying bodies, employment agencies, education, provision of goods and services, accommodation, and registered clubs. |
|
Northern Territory: Anti-Discrimination Act 1996 (NT) Discrimination on the basis of race, sex, sexuality, age, marital status, pregnancy, parenthood, breastfeeding, impairment, trade union or employer association activity, religious belief or activity, irrelevant criminal record, political opinion, affiliation or activity, irrelevant medical record, and association with person with an above attribute. Sexual harassment is also prohibited under this Act. |
Discrimination in education, work, accommodation, provision of goods, services and facilities, clubs, insurance, and superannuation. |
|
Queensland: Anti-Discrimination Act 1991 (QLD) Discrimination on the basis of sex, relationship status, pregnancy, parental status, breastfeeding, race, age, impairment, religious belief or religious activity, political belief or activity, trade union activity, lawful sexual activity, gender identity, sexuality, family responsibilities, and association with or in relation to a person who has any of the above attributes. Sexual harassment and vilification on the basis of race, religion, sexuality or gender identity are also prohibited under this Act. |
Discrimination in work and work-related areas (paid and unpaid), education, provision of goods and services, superannuation and insurance, disposal of land, accommodation; club membership and affairs, administration of state laws and programs, local government, qualifications, industrial, trade, professional or business organisation membership, and existing partnership and in pre-partnership. |
|
South Australia: Equal Opportunity Act 1984 (SA) Discrimination on the basis of sex, breastfeeding, including bottle feeding, chosen gender, sexuality, marital or domestic partnership status, pregnancy, race, age, disability, including aid of assistance animal, association with a child, caring responsibilities, religious appearance or dress, and spouse or partner’s identity. Sexual harassment is also prohibited under this Act. |
Discrimination in employment, partnerships, clubs and associations, qualifying bodies, education, provision of goods and services, accommodation, sale of land, advertising (including employment agencies), conferral of qualifications, and superannuation. |
|
Tasmania: Anti-Discrimination Act 1998 (TAS) Discrimination on the basis of age, breastfeeding, disability, family responsibilities, gender, gender identity, intersex status, industrial activity, irrelevant criminal record, irrelevant medical record, lawful sexual activity, marital status, relationship status, parental status, political activity, political belief or affiliation, pregnancy, race, religious activity, religious belief or affiliation, sexual orientation, and association with a person who has, or is believed to have, any of these attributes. Sexual harassment and the incitement of hatred on the basis of race, disability, sexual orientation, lawful sexual activity, or religious belief, affiliation or activity are also prohibited under this Act. |
Discrimination in employment (paid and unpaid), education and training, provision of facilities, goods and services, accommodation, membership and activities of clubs, administration of any law of the State or any State program, and awards, enterprise agreements and industrial agreements. |
|
Victoria: Equal Opportunity Act 2010 (VIC) Discrimination on the basis of age, breastfeeding, disability, employment activity, gender identity, industrial activity, lawful sexual activity, marital status, parental status or status as a carer, physical features, political belief or activity, pregnancy, race (including colour, nationality, ethnicity and ethnic origin), religious belief or activity, sex, sexual orientation, and personal association with someone who has, or is assumed to have, any of these personal characteristics. Sexual harassment is also prohibited under this Act. Victoria: Racial and Religious Tolerance Act 2001 (VIC) Vilification on the basis of race or religion is prohibited under this Act. |
Discrimination in employment, partnerships, firms, qualifying bodies, industrial organisations, education, provision of goods and services, disposal of land, accommodation (including alteration of accommodation), clubs, sport, and local government. |
|
Western Australia: Equal Opportunity Act 1984 (WA) Discrimination on the basis of sex, sexual orientation (including by association), marital status, pregnancy, breastfeeding, race, religious or political conviction, age (including by association), impairment (including by association), family responsibility or family status, gender history, and publication of relevant details on Fines Enforcement Registrar’s website. Sexual harassment and racial harassment are also prohibited under this Act. Western Australia: Spent Convictions Act 1988 (WA) Discrimination on the basis of having a spent conviction is prohibited under this Act. |
Discrimination in employment, including against applicants, commission agents and contract workers, partnerships, professional or trade organisations, qualifying bodies, employment agencies, application forms, advertisements, education, access to places and vehicles, provision of goods, services and facilities, accommodation, clubs, and land. |

Corey, G., Corey, M., & Callanan, P. (2011.). The client’s right to give informed consent. In Issues and ethics in the helping profession (8th ed.), (pp. 160-162). Cengage Learning.
The first step in protecting the rights of clients is the informed consent document. Informed consent involves the right of clients to be informed about their therapy and make autonomous decisions pertaining to it. Informed consent is a shared decision-making process in which a practitioner provides adequate information so that a potential client can make an informed decision about participating in the professional relationship (Barnett, Wise, et al., 2007). One benefit of informed consent is that it increases the chances that clients will become involved, educated, and willing participants in their therapy. Mental health professionals are required by their ethics codes to disclose to clients the risks, benefits and alternatives to proposed treatment. The intent of an informed consent document is to define boundaries and clarify the nature of the basic counseling relationship between the counselor and the client. Although informed consent has both legal and ethical dimensions, it is best viewed “as an integral aspect of the psychotherapy process that is essential for its success” (Snyder & Barnett, 2006, p. 40). Informed consent for treatment is a powerful clinical, legal, and ethical tool (Wheeler & Bertram, 2008).
Informed consent entails a balance between telling clients too much and telling them too little. Most professionals agree that it is crucial to provide clients with information about the therapeutic relationship, but the manner in which this is done in practice varies considerably among therapists. It is a mistake to overwhelm clients with too much detailed information at once, but it is also a mistake to withhold important information that clients need if they are to make wise choices about their therapy. Studies of practitioners’ informed practices have found considerable variability in the breadth and depth of the informed consent given to clients (Barnett, Wise, et al., 2007).
Professionals have a responsibility to their clients to make reasonable disclosure of all significant facts, the nature of the procedure, and some of the more probable consequences and difficulties. Clients have the right to have treatment explained to them. The process of therapy is not so mysterious that it cannot be explained in a way that clients can comprehend how it works. For instance, most residential addictions treatment programs require that patients accept the existence of a power higher than themselves. This “higher power” is defined by the patient, not by the treatment program. Before patients agree to entering treatment, they have a right to know this requirement. It is important that clients give their consent with understanding. It is the responsibility of professionals to assess the client’s level of understanding and to promote the client’s free choice. Professionals need to avoid subtly coercing clients to cooperate with a therapy program to which they are not freely consenting.
Legal Aspects of Informed Consent
Generally, informed consent requires that the client understands the information presented, gives consent voluntarily, and is competent to give consent to treatment (Barnett, Wise, et al., 2007; Wheeler & Bertram, 2008). Therapists must give clients information in a clear way and check to see that they understand it. Disclosures should be given in plain language in a culturally sensitive manner and must be understandable to clients, including minors and people with impaired cognitive functioning (Goodwin, 2009a). To give valid consent, it is necessary for clients to have adequate information about both the therapy procedures and the possible consequences.
Educating Clients About Informed Consent
A good foundation for a therapeutic alliance is for therapists to employ an educative approach, encouraging clients’ questions about assessment or treatment and offering useful feedback as the treatment process progresses. Here are some questions therapists and clients could address at the outset of the therapeutic relationship:
- What are the goals of the therapeutic endeavour?
- What services will the counselor provide?
- What is expected of the client?
- What are the risks and benefits of therapy?
- What are the qualifications of the provider of services?
- What are the financial considerations?
- To what extent can the duration of therapy be predicted?
- What are the limitations of confidentiality?
- What information about the counselor’s values should be provided in the informed consent document so that clients can choose whether they want to enter a professional relationship with this counselor?
- In what situations does the practitioner have mandatory reporting requirements?
- If the person is referred for an assessment or for therapy from the court or from an employer, who is the client?
A basic part of the informed consent process involves giving clients an opportunity to raise questions and to explore their expectations of counseling. We recommend viewing clients as partners with their therapists in the sense that they are involved as fully as possible in each aspect of their therapy. Practitioners cannot assume that clients clearly understand what they are told initially about the therapeutic process. Furthermore, informed consent is not easily completed within the initial session by asking clients to sign forms. The Canadian Code of Ethics for Psychologists (CPA, 2000) states that informed consent involves a process of reaching an agreement to work collaboratively rather than simply having a consent form signed (Section 1.17).
Informed consent is a collaborative process that helps to establish and enhance the therapeutic relationship (Snyder & Barnett, 2006). The more clients know about how therapy works, including the roles of both client and therapist, the more clients will benefit from the therapeutic experience. Educating clients about the therapeutic process is an ongoing endeavour. Informed consent is not a single event; rather, it is best viewed as a process that continues for the duration of the professional relationship as issues and questions arise (Barnett, Wise, et al., 2007; Barnett & Johnson, 2010; Goodwin, 2009a; Snyder and Barnett, 2006; Wheeler and Bertram, 2008).
The informed consent process is a way of engaging the full participation of the client; it is a means of empowering the client, giving it clinical as well as ethical significance. Especially in the case of clients who have been victimized, issues of power and control can be central in the therapy process. The process of informing clients about therapy increases the chances that the client-therapist relationship will become a collaborative partnership.
Practitioners are ethically bound to offer the best quality of service available, and clients have a right to know that managed care programs, with their focus on constant containment, may have adverse effects on the quality of care available. Clinicians are expected to provide prospective clients with clear information about the benefits to which they are entitled and the limits of treatment.

Kampf, A., McSherry, B., Rothschild, A., & Ogloff, J. (2010). Statutory schemes. In Confidentiality for mental health professionals (pp. 75-92). Australian Academic Press.
One of the most complex aspects of the law on confidentiality is trying to understand the variety of legislative provisions dealing with confidential information and its interplay with the common law. It is important to differentiate between the statutory schemes within Commonwealth legislation and the states’ and territories’ legislation that relate to private or confidential information. Confidentiality provisions and provisions for the disclosure of certain information can be found in legislation relating to mental health care; court proceedings; criminal investigations; the use, collection and storage of health information; guardianship; and other areas. The following broad overview of legislative requirements will focus on provisions that specifically address health information or provisions that are particularly relevant to mental health care settings. The overview will include a list of some of the relevant provisions on matters of confidentiality within federal, state and territory legislation. Although this list is not exhaustive, it provides a reference point for understanding the scope of current provisions. If there is some doubt as to which statutory provisions apply to a practical dilemma, it is important and helpful to seek professional advice from indemnity insurers and legal counsel to assist in decision-making.
Privacy and Health Records Legislation
The Privacy Act 1988 (Cth) evolved in response to international law developments concerning the protection of privacy. In particular, privacy issues are addressed in:
- the United Nations International Covenant on Civil and Political Rights (ICCPR) (http://www2.ohchr.org/english/law/ccpr.htm);
- the Organisation for Economic Cooperation and Development (OECD) Privacy Guidelines (available at http://www.oecd.org/); and
- the Council of Europe’s Convention for the Protection of Individuals with Regard to Automatic Processing of Personal Data (http://epic.org/privacy/intl/coeconvention/).
An investigation into Australia’s privacy protection scheme suggested that improvements were necessary in order to comply with international standards (Law Reform Commission, 1983). In response to that finding, privacy legislation was enacted.
The Privacy Act 1988 (Cth) establishes a legal obligation for employees to keep health records confidential. It also distinguishes between two sets of principles: the Information Privacy Principles (IPP) and the National Privacy Principles (NPP). The IPP apply to federal and Australian Capital Territory government agencies, while the NPP apply to parts of the private sector and individuals. The fact that the Privacy Act establishes these two distinctive schemes to handle health information in the private and public sectors can be confusing and has attracted criticism (Office of the Privacy Commissioner, 2005, 64ff).
As the NPP provide specific rules to protect sensitive health information, this type of information is subject to stronger protection than other private information. Principle 2 of the NPP generally prohibits disclosure of personal health information beyond its primary purpose. The primary purpose is typically the diagnosis and treatment of the client or patient. But disclosure is permissible in the following circumstances:
- if it is directly related to the primary purpose and within the client’s or patient’s reasonable expectations;
- if the client or patient consents to it; or
- if disclosure is required or authorised by law.
Sensitive health information may also be disclosed in order to lessen or prevent either a serious and imminent threat to an individual’s life, health or safety, or a serious threat to public health or safety. It should be noted, however, that the NPP do not impose a duty to disclose information. Note 2 in the NPP Schedule 3.2.1 explicitly states that ‘an organisation is always entitled not to disclose personal information in the absence of a legal obligation to disclose it’.
All states and territories have also enacted specific health records and information privacy legislation. Table 6.1 sets out the main provisions in this area. The provisions in these statutes are generally more detailed than those included in mental health legislation. They are mostly based on the IPP or NPP, found in the Privacy Act 1988 (Cth). In turn, they also distinguish between the public and private service sectors and, depending on whether a mental health service is part of the public or private sector, different statutes apply in some states and territories. As the health record provisions are similar to the IPP and NPP of the Privacy Act 1988 (Cth), further elaboration will be omitted.
However, it is worth noting that all relevant provisions permit disclosure in an emergency situation when that disclosure is necessary to lessen or prevent a serious and imminent threat to the life, health or safety of a person. Confidential information may also be disclosed to lessen or prevent a serious threat to public health or public safety.
Key Points
- The Privacy Act 1988 (Cth) and health records statutes protect health records and information from disclosure.
- Exceptions to the general rule of confidentiality permit disclosure in the following circumstances:
- if disclosing confidential information is directly related to the treatment of the client or patient or within that client’s or patient’s reasonable expectations
- if the client or patient consents to disclosing confidential information;
- if disclosure serves to lessen or prevent either a serious and imminent threat to an individual’s life, health or safety, or a serious threat to public health or safety;
- if disclosure is otherwise authorised by law.
Table 6.1 Most relevant legislation on disclosure of health information
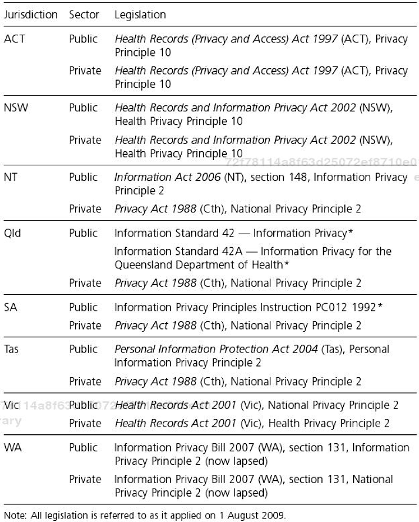
Mental Health Legislation
General Provisions Dealing with Confidentiality
All Australian states and territories have specific mental health legislation in place. With the exception of the Australian Capital Territory, each piece of mental health legislation incorporates specific provisions that generally protect confidentiality in mental health settings. The Mental Health (Treatment and Care) Act 1994 in the Australian Capital Territory is currently under review and it may be that a revised Act will contain confidentiality provisions.
The relevant mental health Acts in Australia use different formulations and define the scope and context of services differently. However, with the exception of the Australian Capital Territory, they essentially protect the information that a mental health professional obtains when he or she exercises functions or powers under the mental health legislation. If mental health professionals who fall under the application of the mental health legislation do not comply with these provisions, various penalties apply.
However, the relevant mental health Acts contain many exceptions and limitations to the duty to maintain confidentiality. As a general observation, it is worth noting that confidential information may be disclosed in the following situations or to the following individuals:
- with the client’s consent;
- when the disclosure is required or authorised by the mental health legislation or other legal provisions;
- to nominated carers or guardians in certain circumstances;
- for the purpose of criminal investigations or criminal proceedings; and
- for statistical analysis and research purposes, provided that there is compliance with further requirements.
Table 6.2 sets out the main provisions in this area. The actual language of the relevant provisions has been used wherever possible, with some paraphrasing.
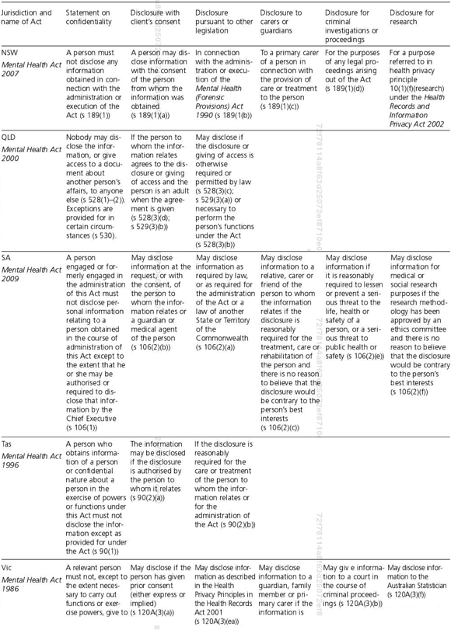
Table 6.2 Provisions dealing with confidentiality in mental health legislation
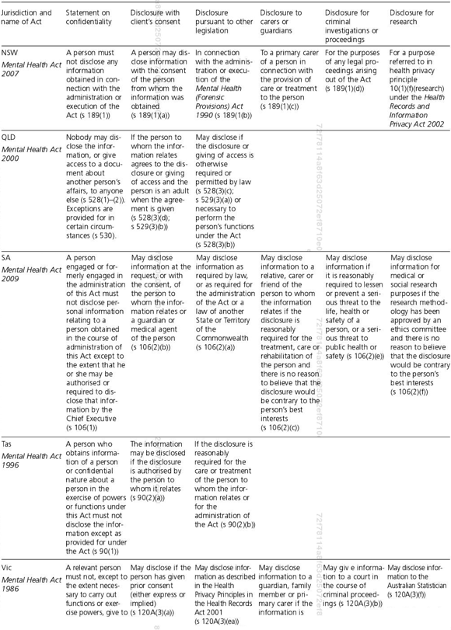
Table 6.2 Provisions dealing with confidentiality in mental health legislation (cont’d)
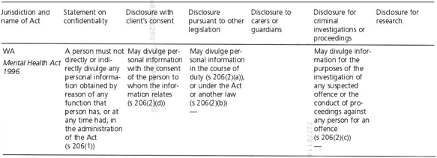
Disclosure for the Protection of Others
Sub-sections 91(2)(f)-(h) of the Mental Health and Related Services Act 2005 (NT) and subsection 106(2)(e) of the Mental Health Act 2009 (SA) are the only legislative provisions that deal specifically with the disclosure of confidential information for the purpose of warning authorities about a client or patient considered to be at risk of harming others.
Sub-section 106(2)(e) of the Mental Health Act 2009 (SA) states that persons engaged in administering the Act ‘may disclose information if it is reasonably required to lessen or prevent a serious threat to the life, health or safety of a person, or a serious threat to public health or safety’. It is important to note that this gives discretion to the relevant person; it is not a mandatory requirement.
The exceptions to confidentiality in the Northern Territory are more complex. Subsections 91(2)(f)-(h) permit (that is, it is not mandatory) disclosure of confidential information to police officers and the Commissioner of Police or persons specifically nominated by the Commissioner of Police.
Confidential information may be disclosed to the Commissioner of Police if the mental health professional ‘reasonably believes’ that the client or patient ‘may harm himself or herself or represents a danger to the general community’ (ss 91(2)(g)).
Sub-section 91(2)(f) also permits a mental health professional to disclose confidential information to a police officer if:
- the person to whom the information relates is in a situation requiring immediate intervention; and
- the person: (A) is likely to cause serious harm to himself or herself or to someone else; or (B) represents a substantial danger to the general community; and
- the information is relevant to the safe resolution of the situation.
In addition, sub-section 91(2)(h) permits a mental health professional to disclose confidential information to a police officer when ‘it is required to prevent or lessen a serious or imminent threat to the life or health of the person, another person or the general community’.
Although legislative provisions enabling disclosure in the public interest exist only in South Australia and the Northern Territory at present, the latter scheme presents a staged approach, which is useful to consider in decision-making. Under the Northern Territory scheme, the more serious the risk, the more flexibility is given to a mental health professional in deciding to whom he or she may disclose confidential information. The legislation differentiates between harm, serious harm, and a serious and imminent threat to a life or to the health of a person.
The other Australian jurisdictions, however, do not specify how to deal with the disclosure of confidential information in emergency situations.
Key Points
- Mental health Acts contain provisions protecting the confidentiality of information about individuals with mental illnesses.
- Mental health Acts contain provisions providing for exceptions to the general duty to maintain confidentiality.
- The Mental Health and Related Services Act 2005 (NT) and the Mental Health Act 2009 (SA) are the only statutes that deal specifically with the disclosure of confidential information for the purpose of warning authorities about a client or patient considered to be at risk of harming others.
Mandatory Reporting of Child Abuse
In addition to the mental health care and confidential information legislation, various other statutory provisions such as those in public health legislation may require the disclosure of confidential information. The most discussed issue in this regard is the mandatory reporting of child abuse.
In most Australian jurisdictions, certain professionals are under a duty to report cases of child abuse. Table 6.3 sets out the main provisions dealing with mandatory reporting. There are penalties for nondisclosure where the person concerned is mandated to disclose the information and fails to do so. As in Table 6.2, the actual language of the Act has been included wherever possible with some paraphrasing.
It should be noted that these statutes also contain provisions permitting disclosure by any person primarily on the basis of a reasonable belief that the child is being sexually or physically abused and some statutes include provisions protecting those who have disclosed information from legal liability. For example, while the Child Protection Act 1999 (Qld) does not have mandatory reporting provisions, section 22 of that Act protects individuals from liability for the notification of, or information given to, the Chief Executive of the Department of Communities about alleged harm or risk of harm.
Many of the state and territory departments responsible for the care and protection of children have the requisite forms for reporting child abuse available on their websites.
Table 6.3 Disclosure mandated in cases of child abuse
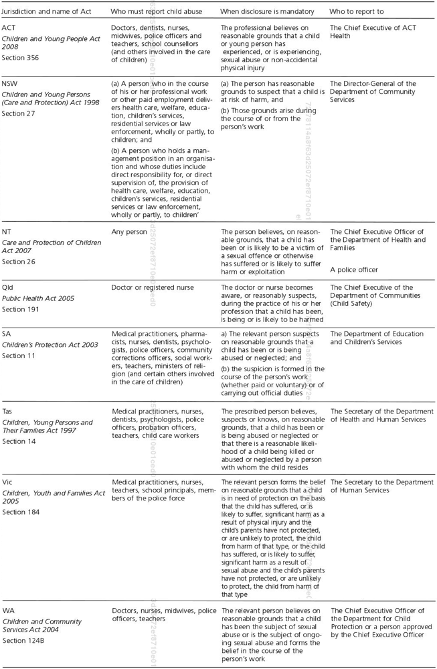
Key Points
- All Australian jurisdictions now have statutory provisions relating to the mandatory reporting of child abuse by certain professionals.
- Disclosure of child abuse is also permitted by any person in certain circumstances.
Other Legislation
There are other statutes requiring the disclosure of confidential information particularly in relation to court proceedings. Each Australian jurisdiction has an Evidence Act that contains provisions enabling courts to request or compel a person to give evidence or produce documents and other statutes enable the issuing of subpoenas or summons to give evidence. Again, it is important to obtain legal advice if a court has issued documents requiring evidence in court or the disclosure of certain documents because there may be circumstances when such legal requests can be challenged.
When dealing with confidential information, the growing importance of human rights should also be considered. On a federal level, Australia does not have a bill or charter of rights, although discussion is now taking place about whether it is necessary to have one. The Australian Capital Territory and Victoria have legislative schemes in place, which provide limited protection of certain human rights (Human Rights Act 2004 (ACT); Charter of Human Rights and Responsibilities Act 2006 (Vic)).
The impact of these schemes is limited in that the human rights they enshrine are not legally enforceable and any laws that conflict with human rights standards cannot be struck down by the courts. Nevertheless, they serve as a reference point for judges in interpreting the law and as an indicator of the human rights commitment of the state or territory government that enacted the legislation. Beyond this, the human rights legislation has an important symbolic value and potential for the interpretation and application of human rights within the Australian legal framework. Thus, the Human Rights Act 2004 (ACT) and the Victorian Charter of Human Rights and Responsibilities are relevant for guiding law and policy-making as well as individual decision-making when applying the law.
An individual’s right to privacy is discussed in section 12 of the Human Rights Act 2004 (ACT) and Part 2 of the Victorian Charter of Human Rights and Responsibilities. The concept of privacy derives from the protection of autonomy and the individual freedom to choose with whom to share private information. It is a concept that is protected in international human rights documents and it is expected that it will increasingly influence law reform and the development of the common law in Australia. With Australia also having ratified the United Nations Convention on the Rights of Persons with Disabilities in July 2008, Australia has strengthened its human rights commitment in particular in the mental health area.
Key Points
- Confidentiality provisions and provisions for the disclosure of certain information can be found in many different statutes.
- Some of the most important provisions can be found in privacy and health records legislation, mental health Acts and legislation dealing with the mandatory disclosure of information regarding child abuse.
- The concept of privacy is protected in international human rights documents, and statutory exceptions are generally carefully circumscribed.
- Australian legislation mandates breaching confidentiality only in limited, clearly identified situations, such as mandatory reporting of child abuse.

Australian Institute of Family Studies. (2020). Mandatory reporting of child abuse and neglect.
If you require assistance or would like to talk to a trained professional about the issues described in this resource sheet, please call Kids Helpline on 1800 55 1800 or Lifeline on 13 11 14.
If you believe a child is in immediate danger call Police on 000.
This resource sheet is provided as a guide only, and is current at the date of publication.
Changes to mandatory reporting laws are currently being considered in various jurisdictions. Individuals are encouraged to contact the relevant department or organisation to clarify requirements in their jurisdiction, or in relation to legislation. For more information and contact details, see the CFCA Resource Sheet Reporting child abuse and neglect: Information for service providers.
Overview
This resource sheet provides members of the community with information on mandatory reporting laws, which require specified people to report suspected abuse and neglect to government child protection services in Australia1. It provides answers to common questions asked about mandatory reporting, outlines the challenges and benefits of mandatory reporting and covers the various mandatory reporting legislation across all Australian jurisdictions.
Introduction
Mandatory reporting laws aim to identify cases of child abuse and neglect, and to assist the individual children in these cases (Royal Commission into Institutional Responses to Child Sexual Abuse, [Royal Commission], 2017). They were first developed in response to the largely hidden nature of child physical abuse and neglect, with the purpose of bringing cases to the attention of child welfare agencies (Mathews, 2014a). They require selected groups of people to report suspected cases of child abuse and neglect to government authorities.
In Australia, the first laws were introduced in South Australia in 1969, and these laws have since been introduced in all Australian jurisdictions (Mathews, 2014b). However, the laws are not the same across all jurisdictions. Differences exist in who has to report, what types of abuse and neglect have to be reported, the ‘state of mind’ that activates the reporting duty (i.e. having a concern, suspicion or belief on reasonable grounds) and who the report is made to. These differences are described and discussed in this resource sheet.
Common Questions
(1) There are legal requirements for various professionals to report other child-related conditions to various authorities (i.e. certain diseases, the occurrence of injuries in children attending schools or child care, and incidents of domestic violence related to adult victims). This resource sheet does not relate to those circumstances but is specific to the reporting of child abuse and neglect to government authorities.
Who Has to Report?
Mandatory reporting legislation generally contains lists of particular occupations that are mandated to report cases of suspected child abuse and neglect. The groups of people mandated to report range from persons in a limited number of occupations (Qld) to a more extensive list (Vic. and WA), to a very extensive list (ACT, NSW, SA and Tas.), through to every adult (NT). The occupations most commonly named as mandated reporters are those who deal frequently with children in the course of their work: teachers, early childhood education and care practitioners, doctors, nurses and police.
What Types of Abuse and Neglect Have to be Reported?
Differences exist in the types of abuse and neglect that must be reported. In some jurisdictions (e.g. NSW and NT) it is mandatory to report suspicions of all five recognised types of abuse and neglect (i.e. physical abuse, sexual abuse, emotional abuse, neglect, and exposure to family violence). In other jurisdictions it is mandatory to report only some of the abuse types (e.g. WA, Qld, Vic. and ACT).
In most jurisdictions the legislation generally specifies that, except for sexual abuse, it is only cases of significant abuse and neglect that must be reported. As sexual abuse should always create a suspicion of significant harm, in practical terms all suspicions of sexual abuse must be reported. While not required by the legislation, suspicions of less severe child abuse and neglect may still be referred to child and family welfare agencies.
It is important to note that the duty to report applies to suspicions that significant abuse or neglect is likely in the future, not just suspected cases of significant abuse or neglect that have already happened.
What Protections Are Given to Mandatory Reporters?
In all jurisdictions, the legislation protects the mandatory reporter’s identity from disclosure. In addition, the legislation provides that as long as the report is made in good faith, the reporter cannot be liable in any civil, criminal or administrative proceedings.
How Does Mandatory Reporting Legislation Define a Child?
Legislation in all jurisdictions except New South Wales and Victoria requires mandatory reporting in relation to all young people up to the age of 18 years. In New South Wales, the duty only applies to situations involving children aged under 16 years. In Victoria, the duty only applies to situations involving children under 17 years of age.
How Does This Type of Mandatory Reporting Co-Exist With Other Types Of Reporting Laws?
This form of mandatory reporting is one of several different legal domains that require designated people to report specified types of child abuse. The reporting duties discussed here are located in child protection legislation in each jurisdiction. They are the major form of reporting duty - being primarily directed towards situations of multiple types of abuse and neglect by parents and caregivers (although, operationally, situations of non-familial sexual abuse will be subsumed under the reporting duty).
Accordingly, other types of reporting laws co-exist with the child protection reporting laws. These other laws appear most prominently in criminal laws and most often require reports of child sexual abuse, although they sometimes extend to serious physical abuse. These criminal law reporting duties do not exist in every jurisdiction, and where they do exist (e.g. in NSW, Vic., the ACT and NT) they have slightly different scope and details, although all require reports to be made to police.
The criminal law reporting duties require all adults in the jurisdiction to report the specified type of abuse. Other types of reporting duty are aimed at identifying institutional sexual abuse. All these different duties are discussed in recent research (Mathews, 2019).
Which Mandated Reports Can Child Protection Services Act On?
A common assumption is that mandatory reporting requirements, the legislative grounds for child protection services intervention, and research classifications of abusive and neglectful behaviour are the same. In fact, mandatory reporting laws define the types of situations that must be reported to statutory child protection services. Legislative grounds for government intervention define the circumstances and, importantly, the threshold at which the statutory child protection service is legally able to intervene to protect a child. Researchers typically focus on defining behaviours and circumstances that can be categorised as abuse and neglect. These differences arise because each description serves a different purpose; the lack of commonality does not mean that the system is failing to work as policy makers had intended.
As such, not all reports of child abuse and neglect lead to immediate action from child protection services. A single report may not meet the threshold for intervention; however, this report grouped with other information on file (or that is yet to be collected) may meet the threshold and result in action being taken. Reports are not looked at in isolation, instead they work to form a body of information that determine if and how child protection services are legally able to intervene.
Can Voluntary Reports Be Made About Abuse and Neglect, Even If Not Required by The Legislation?
Any person is lawfully entitled to make a report if they are concerned for a child’s welfare, even if they are not required to do so as a mandatory reporter. Anyone making a voluntary (non-mandated) report is also protected with regard to confidentiality and immunity from legal liability as outlined above.
In addition to the mandatory reporting legislation, certain professional groups (such as psychologists) and government agencies (such as education departments) may have their own occupational reporting protocols outlining the moral, ethical, professional or organisational responsibility to report. These policy-based reporting duties may be narrower, broader or the same as those officially mandated under legislation. For example, in Queensland, teachers are required to report all forms of suspected significant abuse and neglect under school policy but are only mandated to report sexual abuse and physical abuse under the legislation.
Challenges with the Introduction of Mandatory Reporting
The introduction of mandatory reporting increases awareness of child abuse and neglect, which can result in a substantial increase in the number of reports being made to child protection services, especially in the short term (Mathews, Lee & Norman, 2016). There need to be adequate resources available to respond to any increased demand for staffing and services. Reporting trends generally stabilise several years after the introduction of a mandatory reporting duty (Mathews, Bromfield, Walsh, & Vimpani, 2015).
It is important that mandated reporters receive multidisciplinary training and accurate information to ensure that they know what cases they have to report, how to make a report containing the details needed by the child welfare agency intake team, and what cases they should not report. This training should occur pre-service and in-service. Since non-mandated reporters make a large proportion of all reports, it is also important for the public to be made aware of the appropriate extent of their responsibility. It is also essential that child and family support services be adequately resourced to respond to children and families in need of protection and assistance.
Benefits of Mandatory Reporting Requirements
As a public policy, mandatory reporting aims to protect children from child abuse and neglect. Mathews and Bross (2008) argue that a society without a mandatory reporting system will be far less able to protect children and assist families, as many cases of child abuse and neglect will remain hidden. Comparative studies between countries with and without a mandatory reporting system have found that substantially more cases of child sexual abuse are identified in countries with a mandatory reporting system (Royal Commission, 2017). Studies in Australia support this finding (Lamond, 1989; Mathews, 2014a; Mathews, Bromfield, Walsh, Cheng, & Norman, 2017; Mathews et al., 2016). Reports by mandated reporters identify large proportions of maltreated children and result in the provision of services to many more children and families (Drake & Jonson-Reid, 2007).
Mandatory reporting also aims to increase the awareness of child abuse and neglect in professionals who work with children and overcome any reluctance to report this abuse (Cashmore, 2002). Mandatory reporting laws set acceptable standards of behaviour for the community (Australian Law Reform Commission [ALRC], 2010), affect the policies and practices of child protection services (Tomison & Tucci, 1997), and make the protection of children from abuse and neglect a professional responsibility.
Mandatory Reporting Legislation
Commonwealth legislation
The Family Law Act 1975 (Cth) creates a mandatory reporting duty for personnel from the Family Court of Australia, the Federal Circuit Court of Australia, the Family Court of Western Australia and other designated practitioners. This includes registrars, deputy registrars, family consultants, family counsellors, family dispute resolution practitioners, arbitrators, and lawyers independently representing children’s interests. Section 67ZA(1) and (2) require that when these persons have reasonable grounds for suspecting that a child has been abused, or is at risk of being abused, and this suspicion is developed in the course of performing their duties or functions, or exercising powers, they must, as soon as practicable, notify a prescribed child welfare authority of their suspicion and its basis.
Australian Capital Territory
The Australian Capital Territory’s mandatory reporting laws cover an extensive list of professions, and the details of the reporting requirements are provided in the table below.
| Legal provisions | Section 356 of the Children and Young People Act 2008 (ACT) |
|---|---|
| Who is mandated to report? | A person who is: a doctor; a dentist; a nurse; an enrolled nurse; a midwife; a psychologist; a teacher at a school; a person authorised to inspect education programs, materials or other records used for home education of a child or young person under the Education Act 2004; a police officer; a person employed to counsel children or young people at a school; a person caring for a child at a child care centre; a person coordinating or monitoring home-based care for a family day care scheme proprietor; a public servant who, in the course of employment as a public servant, works with, or provides services personally to children and young people or families; the public advocate; an official visitor; a minister of religion, religious leader or member of the clergy of a church or religious denomination; a person who, in the course of the person’s employment, has contact with or provides services to children, young people and their families and is prescribed by regulation. |
| What must be reported? | A belief, on reasonable grounds, that a child or young person has experienced or is experiencing sexual abuse or non-accidental physical injury; and the reasons for the belief arise from information obtained by the person during the course of, or because of, the person’s work (whether paid or unpaid) |
| Abuse and neglect types that must be reported |
Physical abuse Sexual abuse |
New South Wales
New South Wales’ mandatory reporting laws cover an extensive list of professions, and the details of the reporting requirements are provided in the table below.
| Legal provisions | Sections 23 and 27 of the Children and Young Persons (Care and Protection) Act 1998 (NSW) | |
|---|---|---|
| Who is mandated to report? |
A person who, in the course of his or her professional work, or other paid employment, delivers health care, welfare, education, children’s services, residential services or law enforcement, wholly or partly, to children. A person who holds a management position in an organisation, the duties of which include direct responsibility for, or direct supervision of, the provision of health care, welfare, education, children’s services, residential services or law enforcement, wholly or partly, to children. |
|
| What must be reported? | Suspicion on reasonable grounds, obtained during the course of or from the person’s work, that a child is at risk of significant harm because of the presence to a significant extent of circumstances of: neglect, physical abuse, sexual abuse, psychological abuse, risk of harm through exposure to domestic violence, and failure to engage with services after a pre-natal report. | |
| Abuse and neglect types that must be reported |
|
|
Northern Territory
The Northern Territory’s mandatory reporting laws apply to any person, with additional provisions covering health practitioners. The details of these reporting requirements are provided in the table below.
| Legal provisions | Sections 15, 16 and 26 of the Care and Protection of Children Act 2007 (NT) | Section 26(2) of the Care and Protection of Children Act 2007 (NT) |
|---|---|---|
| Who is mandated to report? | Any person | A health practitioner or someone who performs work of a kind that is prescribed by regulation |
| What must be reported? | A belief on reasonable grounds that a child has suffered or is likely to suffer harm or exploitation | Reasonable grounds to believe a child aged 14 or 15 years has been or is likely to be a victim of a sexual offence and the age difference between the child and offender is greater than 2 years |
| Abuse and neglect types that must be reported |
|
|
Queensland
Queensland has three separate pieces of mandatory reporting legislation, each covering different occupational groups and having their own reporting requirements. The details of these pieces of legislation are provided in the table below.
| Legal provisions | Part 1AA, section 13F of the Child Protection Act 1999 (Qld) | Part 1AA, section 13E of the Child Protection Act 1999 (Qld) | Sections 364, 365, 365A, 366, 366A of the Education (General Provisions) Act 2006 (Qld) |
|---|---|---|---|
| Who is mandated to report? | An authorised officer, a public service employee employed in the department, a person employed in a departmental care service or licensed care service | Doctors; registered nurses; teachers; a police officer who, under a direction given by the commissioner of the police service under the Police Service Administration Act 1990, is responsible for reporting under this section; a person engaged to perform a child advocate function under the Public Guardian Act 2014; early childhood education and care professionals. | School staff |
| What must be reported? | A reasonable suspicion that a child in care (a child placed in the care of an entity conducting a departmental care service or a licensee) has suffered, is suffering, or is at unacceptable risk of suffering, significant harm caused by physical or sexual abuse | A reasonable suspicion that a child has suffered, is suffering or is at an unacceptable risk of suffering, significant harm caused by physical or sexual abuse; and may not have a parent able and willing to protect the child from the harm | Awareness or reasonable suspicion that a child has been or is likely to be sexually abused; and the suspicion is formed in the course of the person’s employment |
| Abuse and neglect types that must be reported |
|
|
|
South Australia
South Australia’s mandatory reporting laws cover an extensive list of professions, and the details of the reporting requirements are provided in the table below.
| Legal provisions | Sections 17, 18, 30 and 31 of the Children and Young People (Safety) Act 2017 (SA) | |
|---|---|---|
| Who is mandated to report? | Medical practitioners; pharmacists; registered or enrolled nurses; dentists; psychologists; police officers; community corrections officers under the Correctional Services Act 1982; social workers; ministers of religion; employees of, or volunteers in, an organisation formed for religious or spiritual purposes; teachers employed as such in a school (within the meaning of the Education and Early Childhood Services (Registration and Standards) Act 2011) or a preschool or kindergarten; employees of, or volunteers in, an organisation that provides health, welfare, education, sporting or recreational, child care or residential services wholly or partly for children and young people, being a person who - (i) provides such services directly to children and young people; or (ii) holds a management position in the organisation, the duties of which include direct responsibility for, or direct supervision of, the provision of those services to children and young people | |
| What must be reported? | Reasonable grounds to suspect a child or young person is, or may be, at risk; and the suspicion was formed in the course of the person’s employment | |
| Abuse and neglect types that must be reported |
|
|
Tasmania
Tasmania’s mandatory reporting laws cover an extensive list of professions, and the details of the reporting requirements are provided in the table below.
| Legal provisions | Sections 3, 4 and 14 of the Children, Young Persons and Their Families Act 1997 (Tas.) | |
|---|---|---|
| Who is mandated to report? | Medical practitioners; registered or enrolled nurses; persons registered under the Health Practitioner Regulation National Law (Tasmania) in the midwifery, dental (dentists, dental therapist, dental hygienist or oral health therapist) or psychology professions; police officers; probation officers; principals and teachers in any educational institution including kindergartens; persons who provide child care or a child care service for fee or reward; persons concerned in the management of an approved education and care service, within the meaning of the Education and Care Services National Law (Tasmania) or a child care service licensed under the Child Care Act 2001; a member of the clergy of any church or religious denomination; a member of the Parliament of this State; any other person who is employed or engaged as an employee for, of, or in, or who is a volunteer in, a government agency that provides health, welfare, education, child care or residential services wholly or partly for children, and an organisation that receives any funding from the Crown for the provision of such services; and any other person of a class determined by the Minister by notice in the Gazette to be prescribed persons. | |
| What must be reported? |
Knowledge, or a belief or suspicion on reasonable grounds that: a child has been or is being ‘abused’ or ‘neglected’ or is an affected child within the meaning of the Family Violence Act 2004 (a child whose safety, psychological wellbeing or interests are affected or likely to be affected by family violence); or there is a reasonable likelihood of a child being killed or abused or neglected by a person with whom the child resides; or while a woman is pregnant, that there is reasonable likelihood that after the birth of the child: the child will suffer abuse or neglect, or may be killed by a person with whom the child is likely to reside; or that the child will require medical treatment or other intervention as a result of the behaviour of the woman or another person with whom the woman resides or is likely to reside, before the birth of the child. Note on extent of harm required to activate the duty (section 3(1) definition of ‘abuse and neglect’: for all forms except sexual abuse, reports must be made where: (i) the injured, abused or neglected person has suffered, or is likely to suffer, physical or psychological harm detrimental to the person’s wellbeing; or (ii) the injured, abused or neglected person’s physical or psychological development is in jeopardy. All instances of suspected sexual abuse must be reported. |
|
| Abuse and neglect types that must be reported |
|
|
Victoria
Victoria’s mandatory reporting laws cover an extensive list of professions, and the details of the reporting requirements are provided in the table below.
| Legal provisions | Sections 182(1), 184 and 162(1)(c)-(d) of the Children, Youth and Families Act 2005 (Vic.) |
|---|---|
| Who is mandated to report? | Registered medical practitioners, nurses, midwives, a person registered as a teacher or an early childhood teacher under the Education and Training Reform Act 2006 or teachers granted permission to teach under that Act; principals of government or non-government schools within the meaning of the Education and Training Reform Act 2006; police officers, a person in religious ministry, out-of-home care workers (excluding voluntary foster and kinship carers), early childhood workers, youth justice workers and registered psychologists. |
| What must be reported? | Belief on reasonable grounds that a child is in need of protection on a ground referred to in section 162(1)(c) or 162(1)(d), formed in the course of practising his or her profession or carrying out the duties of his or her office, position or employment as soon as practicable after forming the belief and after each occasion on which he or she becomes aware of any further reasonable grounds for the belief |
| Abuse and neglect types that must be reported |
Note that technically, under s. 162, the duty is limited to instances of physical injury and sexual abuse where ‘the child’s parents have not protected, or are unlikely to protect, the child from harm of that type’. |
Western Australia
Western Australia has two separate pieces of mandatory reporting legislation, each covering different occupation groups and having their own reporting requirements. The details of these pieces of legislation are provided in the table below.
| Legal provisions | Sections 124A and 124B of the Children and Community Services Act 2004 (WA)2 | Sections 5 and 160 of the Family Court Act 1997 (WA) |
|---|---|---|
| Who is mandated to report? | Doctors; nurses and midwives; teachers and boarding supervisors; and police officers | The Principal Registrar, a registrar or a deputy registrar; family counsellors; family consultants; family dispute resolution practitioners, arbitrators or legal practitioners independently representing the child’s interests |
| What must be reported? | Belief on reasonable grounds that child sexual abuse has occurred or is occurring, where this belief is formed in the course of the person’s work, whether paid or unpaid | Reasonable grounds for suspecting that a child has been: abused, or is at risk of being abused; ill-treated, or is at risk of being ill-treated; or exposed or subjected to behaviour that psychologically harms the child |
| Abuse and neglect types that must be reported |
|
|
(2) Note: The Western Australian Government has announced its intent for this Act to be amended to introduce mandatory reporting of child sexual abuse for ministers of religion, including where this knowledge is gained through religious confession. These amendments are yet to be enacted (Government of Western Australia, 2019).
Further Reading
- Kohl, P., Jonson-Reid. M., & Drake, B. (2009). Time to leave substantiation behind: Findings from a national probability study. Child Maltreatment, 14(1), 17.
- Mathews, B. (2012). Exploring the contested role of mandatory reporting laws in the identification of severe child abuse and neglect. In M. Freeman (Ed.), Current legal issues (Vol. 14: Law and Childhood Studies) (pp. 302-338). Oxford: Oxford University Press.
- Mathews, B., & Kenny, M. (2008). Mandatory reporting legislation in the USA, Canada and Australia: A cross-jurisdictional review of key features, differences and issues. Child Maltreatment, 13, 50-63.
- Mathews, B., & Walsh, K. (2014). Mandatory reporting laws. In A. Hayes & D. Higgins (Eds.), Families, policy and the law: Selected essays on contemporary issues for Australia (pp. 131-142). Melbourne: AIFS. Retrieved from www.aifs.gov.au/publications/families-policy-and-law/14-mandatory-reporting-laws
- Melton, G. (2005). Mandated reporting: A policy without reason. Child Abuse & Neglect, 29, 9-18.
- Tomison, A. (2002). Mandatory reporting: A question of theory versus practice. Developing Practice: The Child, Youth and Family Work Journal, 4, 13-17.
For more resources, visit the CFCA mandatory reporting bibliography.

Workplace Health and Safety Queensland. (2021). How to manage work health and safety risks – Code of practice (pp. 5-25).
1. Introduction
1.1 Who has duties for managing work health and safety risks?
Duty holders who have a role in managing work health and safety risks include:
- persons conducting a business or undertaking (PCBUs)
- officers
- designers, manufacturers, importers, suppliers and installers of plant, substances or
- structures.
Workers and other persons at the workplace also have duties under the WHS Act, such as the duty to take reasonable care for their own health and safety at the workplace.
A person can have m Person conducting a business or undertaking
WHS Act section 19
Primary duty of care
A PCBU must eliminate risks in the workplace, or if that is not reasonably practicable, minimise the risks so far as is reasonably practicable.
The WHS Regulations include more specific requirements for PCBUs to manage the risks of hazardous chemicals, airborne contaminants and plant, as well as other hazards associated with the workplace.
PCBUs have a duty to consult workers about work health and safety and may also have duties to consult, cooperate and coordinate with other duty holders.
Examples of where a PCBU will have a health and safety duty include when:
- the PCBU engages workers to carry out work
- the PCBU directs or influences workers in carrying out work
- other people may be put at risk from work carried in their business or undertaking, and
- the PCBU manages or controls a workplace or fixtures, fittings or plant at the workplace.
Officers
WHS Act section 27
Duty of officers
Officers, such as company directors, have a duty to exercise due diligence to ensure the PC-BU complies with the WHS Act and WHS Regulations. This includes taking reasonable steps to gain an understanding of the hazards and risks associated with the operations of the business or undertaking, and ensure the business or undertaking has and uses appropriate resources and processes to eliminate or minimise risks to health and safety.
Designers, manufacturers, importers and suppliers of plant, substances or structures
WHS Act Part 2 Division 3
Further duties of persons conducting businesses or undertakings
Designers, manufacturers, importers and suppliers of plant, substances or structures must ensure, so far as is reasonably practicable, the plant, substance or structure they design, manufacture, import or supply is without risks to health and safety. This duty includes carrying out testing and analysis as well as providing specific information about the plant, substance or structure.
The WHS Regulations include a number of specific requirements for consultation and information sharing to assist in meeting these duties, for example:
- manufacturers to consult with designers of plant
- importers to consult with designers and manufacturers of plant, and
- the person who commissions construction work to consult with the designer of the structure.
Workers
WHS Act section 28
Duties of workers
Workers have a duty to take reasonable care for their own health and safety and to not adversely affect the health and safety of other persons. Workers must comply with reasonable instructions, so far as they are reasonably able, and cooperate with reasonable health and safety policies or procedures that have been notified to workers.
If personal protective equipment (PPE) is provided by the business or undertaking, the worker must so far as they are reasonably able, use or wear it in accordance with the information and instruction and training provided.
Other persons at the workplace
WHS Act section 29
Duties of other persons at the workplace
Other persons at the workplace, like visitors, must take reasonable care for their own health and safety and must take reasonable care not to adversely affect other people’s health and safety. They must comply, so far as they are reasonably able, with reasonable instructions given by the PCBU to allow that person to comply with the WHS Act.
1.2 What is involved in managing risks?
Management Commitment
Effective risk management starts with a commitment to health and safety from those who operate and manage the business or undertaking. You also need the involvement and cooperation of your workers, supply chain partners, and other businesses you work with. Management commitment is about demonstrating you are serious about health and safety and influencing other duty holders in the workplace.
To demonstrate your commitment, you should:
- get involved in health and safety issues so that you understand the hazards and risk associated with your operations
- consult workers and other duty holders on the hazards and risk, and how to control them
- invest time and money in health and safety
- ensure you and your workers clearly understand health and safety responsibilities and have the knowledge and skill to do tasks safely, and
- apply health and safety values and behaviours to your own work practices.
A step-by-step process
A safe and healthy workplace does not happen by chance or guesswork. You have to think about what could go wrong at your workplace and what the consequences could be. Then you must do whatever you can (in other words, whatever is ‘reasonably practicable’) to eliminate or minimise health and safety risks arising from your business or undertaking.
This process is known as risk management and involves the four steps set out in this Code (see Figure 1 below):
- Identify hazards – find out what could cause harm.
- Assess risks, if necessary – understand the nature of the harm that could be caused by the hazard, how serious the harm could be and the likelihood of it happening. This step may not be necessary if you are dealing with a known risk with known controls.
- Control risks – implement the most effective control measure that is reasonably practicable in the circumstances and ensure it remains effective over time.
- Review hazards and control measures to ensure they are working as planned.
This process will be implemented in different ways depending on the size and nature of your business or undertaking. Larger businesses and those in sectors where workers are exposed to more or higher risks are likely to need more complex, sophisticated risk management processes.
Examples demonstrating how to manage work health and safety risks in consultation with workers are at Appendix B.
Determining what is ‘reasonably practicable’
Deciding what is ‘reasonably practicable’ to protect people from harm requires taking into account and weighing up all relevant matters, including:
- the likelihood of the hazard or risk concerned occurring
- the degree of harm that might result from the hazard or risk
- knowledge about the hazard or risk, and ways of eliminating or minimising the risk
- the availability and suitability of ways to eliminate or minimise the risk, and
- after assessing the extent of the risk and the available ways of eliminating or minimising the risk, the cost associated with available ways of eliminating or minimising the risk, including whether the cost is grossly disproportionate to the risk.
Further information is available in the Interpretive Guideline: The meaning of ‘reasonably practicable’. The process of managing risk described in this Code will help you decide what is reasonably practicable in particular situations so that you can meet your duty of care under the WHS laws.
Many hazards and their associated risks are well known and have well established and accepted control measures. In these situations, the second step to formally assess the risk is unnecessary. If, after identifying a hazard, you already know the risk and how to control it effectively, you can implement the controls without undertaking a risk assessment.
Risk management is a proactive process that helps you respond to change and facilitate continuous improvement in your business. It should be planned, systematic and cover all reasonably foreseeable hazards and associated risks.
Consulting workers
WHS Act section 47
Duty to consult workers
WHS Act section 48
Nature of Consultation
A PCBU must consult, so far as is reasonably practicable, with workers who carry out work for the business or undertaking and who are (or are likely to be) directly affected by a health and safety matter.
This duty to consult is based on the recognition that worker input and participation improves decision-making about health and safety matters and assists in reducing work-related injuries and disease.
The broad definition of a ‘worker’ under the WHS Act means a PCBU must consult, so far as is reasonably practicable, with contractors and sub-contractors and their employees, on-hire workers, outworkers, apprentices, trainees, work experience students, volunteers and other people who are working for the PCBU and who are, or are likely to be, directly affected by a health and safety matter.
Workers are entitled to take part in consultations and to be represented in consultations by a health and safety representative who has been elected to represent their work group.
Consultation with workers and their health and safety representatives is required at each step of the risk management process. By drawing on the experience, knowledge and ideas of your workers you are more likely to identify all hazards and choose effective control measures.
You should encourage your workers to report any hazards and health and safety problems immediately so that risks can be managed before an incident occurs.
If you have a health and safety committee, you should engage the committee in the risk management process as well.
Consulting, cooperating and coordinating activities with other duty holders
WHS Act section 46
Duty to consult with other duty holders
The WHS Act requires that a PCBU to consult, cooperate and coordinate activities with all other persons who have a work health or safety duty in relation to the same matter, so far as is reasonably practicable.
There is often more than one business or undertaking involved in the same activities or who share the same workplace who may each have responsibility for the same health and safety matters, either because they are involved in the same activities or share the same workplace.
In these situations, each duty holder should exchange information to find out who is doing what and work together in a cooperative and coordinated way so risks are eliminated or minimised so far as is reasonably practicable.
For example, if you engage labour hire workers as part of your workforce you share a duty of care to these workers with the business that provides them. In these situations, you must discuss the hazards and risks associated with the work and what precautions will be taken with the labour hire firm.
Never assume that someone else is taking care of a health and safety matter. Find out who is doing what and work together with other duty holders in a cooperative and coordinated way so risks are eliminated or minimised as far as reasonably practicable.
When entering into contracts you should communicate your safety requirements and policies, review the job to be undertaken, discuss any safety issues that may arise and how they will be dealt with. Remember that you cannot transfer your responsibilities to another person.
Further guidance on WHS consultation is available in the Code of Practice: Work health and safety consultation, cooperation and coordination.
1.3 When should a risk management approach be used?
Managing work health and safety risks is an ongoing process that needs attention over time, but particularly when any changes affect your work activities. Examples of when you should work through the steps in this Code include:
- starting a new business
- expanding or purchasing an existing business
- changing work practices, procedures or the work environment
- changing organisational structure or job roles
- introducing new workers or returning workers to the workplace
- purchasing new or used equipment or using new substances
- working with a new supplier or new commissioner of your services
- planning to improve productivity or reduce costs
- new information about workplace risks becomes available
- responding to workplace incidents (even if they have caused no injury)
- responding to concerns raised by workers, health and safety representatives or others at the workplace, or
- required by the WHS regulations for specific hazards.
It is also important to use the risk management approach when designing and planning products, processes or places used for work, because it is often easier and more effective to eliminate hazards before they are introduced into a workplace by incorporating safety features at the design stage.
The risk management process outlined in this Code should be applied to both physical and psychological risks. Further guidance specific to psychological risks is available in the Guide: Integrated approach to work-related psychosocial health and safety and the Guide for preventing and responding to workplace bullying.
2. Step 1—How to identify hazards
Identifying hazards in the workplace involves finding things and situations that could potentially cause harm to people. Hazards generally arise from the following aspects of work and their interaction:
- physical work environment
- equipment, materials and substances used
- work tasks and how they are performed, and
- work design and management.
Table 1 below lists some common types of workplace hazards. Some hazards are part of the work process, such as mechanical hazards, noise or toxic properties of substances. Other hazards result from equipment or machine failures and misuse, chemical spills and structural failures, or where work demands exceed a worker’s ability to cope.
A piece of plant, substance or a work process may have many different hazards. Each of these hazards needs to be identified. For example, a production line may have dangerous moving parts, noise, hazards associated with manual tasks and psychosocial hazards due to the pace of work.
| Table 1 Examples of common hazards | ||
|---|---|---|
| Hazard | Example | Potential harm |
| Manual tasks | Tasks involving sustained or awkward postures, high or sudden force, repetitive movements or vibration | Musculoskeletal disorders such as damage to joints, ligaments and muscles |
| Gravity | Falling objects, falls, slips and trips of people | Fractures, bruises, lacerations, dislocations, concussion, permanent injuries or death |
| Psychosocial | Excessive time pressure, bullying, violence and work-related fatigue | Psychological or physical injury or illness |
| Electricity | Exposure to live electrical wires | Shock, burns, damage to organs and nerves leading to permanent injuries or death |
| Machinery and equipment | Being hit by moving vehicles, or being caught in moving parts of machinery | Fractures, bruises, lacerations, dislocations, permanent injuries or death |
| Hazardous chemicals | Acids, hydrocarbons, heavy metals, asbestos and silica | Respiratory illnesses, cancers or dermatitis |
| Extreme temperatures | Heat and cold |
Heat can cause burns and heat stroke or injuries due to fatigue Cold can cause hypothermia or frost bite |
| Noise | Exposure to loud noise | Permanent hearing damage |
| Radiation | Ultra violet, welding arc flashes, micro waves and lasers | Burns, cancer or blindness |
| Biological | Micro-organisms | Hepatitis, legionnaires’ disease, Q fever, HIV/AIDS or allergies |
2.1 How to find hazards
Inspect the workplace
As a person conducting a business or undertaking (PCBU), regularly walking around the workplace and observing how things are done can help you predict what could or might go wrong. Look at how people actually work, how plant and equipment are used, what chemicals are around and what they are used for, what safe or unsafe work practices exist as well as the general state of housekeeping.
Things to look out for include the following:
- Does the work environment enable workers to carry out work without risks to health and safety (for example, space for unobstructed movement, adequate ventilation, lighting)?
- How is work performed, including the physical, mental and emotional demands of the tasks and activities?
- How suitable are the tools and equipment for the task and how well are they maintained?
- How do workers, managers, supervisors and others interact and how are inappropriate behaviours or conflicts dealt with?
- Have any changes occurred in the workplace which may affect health and safety?
Hazards are not always obvious. Some hazards can affect health over a long period of time or may result in stress (such as bullying) or fatigue (such as shiftwork). Also think about hazards that you may bring into your workplace with new, used or hired goods (for example, worn insulation on a hired welding set).
As you walk around, you may spot straightforward problems and action should be taken on these immediately, for example cleaning up a spill. If you find a situation where there is immediate or significant danger to people, move those persons to a safer location first and attend to the hazard urgently. Follow up on why the situation occurred to identify additional hazards and risks.
Make a list of the hazards you find, including the ones you know are already being dealt with, to ensure that nothing is missed. This list can be kept and updated next time you do an inspection. You may use a checklist designed to suit your workplace to help you find and make a note of hazards.
Good work design and safe design
The best chance to find ways to eliminate hazards and minimise risks is during the design phase.
Effective design of ‘good work’ considers the work tasks, work systems, the physical working environment, and the workers and others in the workplace. For more information on good work design principles, see Principles of good work design: A work health and safety handbook.
Safe design of buildings, structures, equipment and vehicles accounts for the hazards and risks present at all stages of the product’s lifecycle. For more information on safe design principles and how to achieve safe design, see Guidance on the principles of safe design for work and the Code of Practice: Safe design of structures.
Consult your workers
Ask your workers about any health and safety problems they have encountered in doing their work and any near misses or incidents that have not been reported.
Worker surveys may also be undertaken to obtain information about matters such as workplace bullying, as well as muscular aches and pains that can signal potential hazards.
Consult your supply chains and networks
Talk with your suppliers or those commissioning your services to understand each other’s needs and identify any hazards and risks. For example, hazards may relate to frequent pressure to deliver services in very tight timeframes or to delay service delivery for long periods which reduce workers’ opportunities to rest. Other hazards may relate to packaging products in ways that increase workers’ risks of musculoskeletal injury or exposure to hazardous chemicals.
When people within a supply chain act cooperatively they can exert greater influence on health and safety than when acting alone.
Review available information
Information and advice about hazards and risks relevant to particular industries and types of work is available from regulators, industry associations, unions, technical specialists and safety consultants.
Manufacturers and suppliers can also provide information about hazards and safety precautions for specific substances (safety data sheets), plant or processes (instruction manuals).
Analyse your records of health monitoring, workplace incidents, near misses, worker complaints, sick leave and the results of any inspections and investigations to identify hazards. If someone has been harmed doing a particular task, then a hazard exists that could hurt someone else. These incidents need to be investigated to find the hazard that caused the injury or illness.
3. Step 2—How to assess risks
A risk assessment involves considering what could happen if someone is exposed to a hazard and the likelihood of it happening. A risk assessment can help you, as a person conducting a business or undertaking (PCBU), to determine:
- how severe a risk is
- whether any existing control measures are effective
- what action you should take to control the risk, and
- how urgently the action needs to be taken.
Many hazards and their associated risks are well known and have well established and accepted control measures. In these situations, the second step to formally assess the risk is not required. If after identifying a hazard you already know the risk and how to control it effectively, you may simply implement the controls.
A risk assessment can be undertaken with varying degrees of detail depending on the type of hazard and the information, data and resources that you have available. It can be as simple as a discussion with your workers or involve specific risk analysis tools and techniques developed for specific risks or recommended by safety professionals. For some complex situations, expert or specialist advice may be useful when conducting a risk assessment.
When should a risk assessment be carried out?
A risk assessment should be done when:
- there is uncertainty about how a hazard may result in injury or illness
- the work activity involves a number of different hazards and there is a lack of understanding about how the hazards may interact with each other to produce new or greater risks, or
- changes at the workplace occur that may impact on the effectiveness of control measures.
In some circumstances, a risk assessment will assist to:
- identify which workers are at risk of exposure
- determine what sources and processes are causing the risk
- identify if and what kind of control measures should be implemented, and
- check the effectiveness of existing control measures.
A risk assessment is mandatory under the WHS Regulations for certain activities that are high risk such as, but not limited to, entry into con-fined spaces, diving work and live electrical work.
Some hazards that have exposure standards, such as noise and airborne contaminants, may require scientific testing or measurement by a competent person to accurately assess the risk and to check that the relevant exposure standard is not being exceeded (for example, by using noise meters to measure noise levels and using gas detectors to analyse oxygen levels in confined spaces).
A risk assessment is not required when legislation requires a hazard or risk to be controlled in a specific way – these requirements must be complied with.
A detailed risk assessment may not be required in the following situations:
- A code of practice or other guidance sets out a way of controlling a hazard or risk that is applicable to your situation.
- There are well-known and effective controls that are in use in the particular industry that are suited to the circumstances in your workplace.
In these situations, you may be able to simply implement these control measures.
A risk assessment may be appropriate to reuse in situations where all the hazards, tasks, things, workers or circumstances are the same and no worker or other person will be exposed to greater, additional or different risks. However, as stated above, if there are any changes at the workplace, a new risk assessment should be performed.
How to do a risk assessment
Hazards have the potential to cause different types and severities of harm, ranging from minor discomfort to a serious injury or death.
For example, heavy liquefied petroleum gas (LPG) cylinders can cause muscular strain when they are handled manually. However, if the cylinder is damaged causing gas to leak, which is then ignited, a fire could result in serious burns. If that leak occurs in a storeroom or similar enclosed space, it could result in an explosion that could destroy the building and kill or injure any-one nearby. Each of the outcomes involves a different type of harm with a range of severities, and each has a different likelihood of occurrence.
The risk will increase as the severity and likelihood of harm increases.
Work out how hazards may cause harm
In most cases, incidents occur as a result of a chain of events and a failure of one or more links in that chain. If one or more of the events can be stopped or changed, the risk may be eliminated or reduced.
One way of working out the chain of events is to determine the starting point where things begin to go wrong and then consider: ‘If this happens, what may happen next?’ This will provide a list of events that sooner or later cause harm. See the example in Appendix C.
In thinking about how each hazard may cause harm, you should consider:
- the effectiveness of existing control measures and whether they control all types of harm
- how work is actually done, rather than relying on written manuals and procedures, and
- infrequent or abnormal situations, as well as how things are normally meant to occur.
Consider how harm could be caused during maintenance and cleaning, as well as breakdowns of equipment and failures of health and safety controls.
Work out how severe the harm could be
To estimate the severity of harm that could result from each hazard you should consider the following questions:
- What type of harm could occur (for example muscular strain, injuries due to fatigue, psychological injury, burns, laceration)? How severe is the harm? Could the hazard cause death, serious injuries, illness or only minor injuries requiring first aid?
- What factors could influence the severity of harm that occurs? For example, the distance someone might fall or the concentration of a particular substance will determine the level of harm that is possible. The harm may occur immediately if something goes wrong (for example injury from a fall) or it may take time for it to become apparent (for example illness from longterm exposure to a substance or to excessive work demands).
- Do you need to use specific tools or processes to assess how severe the harm could be? This could include sending samples to a lab for testing or arranging noise exposure level testing.
- How many people are exposed to the hazard and how many could be harmed in and outside your workplace? For example, a mobile crane collapse on a busy construction site has the potential to kill or injure a large number of people.
- Could one failure lead to other failures? For example, could the failure of your electrical supply make any control measures that rely on electricity ineffective?
- Could a small event escalate to a much larger event with more serious consequences? For example, a minor fire can get out of control quickly in the presence of large amounts of combustible materials.
Work out the likelihood of harm occurring
The likelihood that someone will be harmed can be estimated by considering the following:
- How often is the task done? Does this make the harm more or less likely?
- How often are people near the hazard? How close do people get to it?
- Has it ever happened before, either in your workplace or somewhere else? How often?
Table 2 contains further questions that can help you estimate likelihood.
| Table 2 Questions to help estimate the likelihood of harm occurring | |
|---|---|
| Questions | Explanation and examples |
| How often are people exposed to the hazard? |
A hazard may exist all of the time or it may only exist occasionally. The more often a hazard is present, the greater the likelihood it will result in harm.
|
| How long might people be exposed to the hazard? |
The longer that someone is exposed to a hazard, the greater the likelihood that harm may result. For example:
|
| How effective are current controls in reducing risk? |
In most cases the risks being assessed will already be subject to some control measures. The likelihood of harm resulting from the risk will depend upon how adequate and effective the current measures are. For example:
|
| Could any changes in your organisation increase the likelihood? |
The demand for goods or services in many organisations varies throughout the year. Changes in demand may be seasonal, depend on environmental conditions or be affected by market fluctuations that are driven by a range of events. Meeting increased demand may cause unusual loads on people, plant and equipment and systems of work. Failures may be more likely. For example:
|
| Are hazards more likely to cause harm because of the working environment? |
Examples of situations where the risk of injury or illness may become more likely:
|
| Could the way people act and behave affect the likelihood of a hazard causing harm? | The possibility that people may make mistakes, misuse items, become distracted or panic in particular situations needs to be taken into account. The effects of fatigue or stress may make it more likely that harm will occur. |
| Do the differences between individuals in the workplace make it more likely for harm to occur? |
Workers are not all the same and individual variability should be considered, for example:
|
You can rate the likelihood as one of the following:
- Certain to occur – expected to occur in most circumstances
- Very likely – will probably occur in most circumstances
- Possible – might occur occasionally
- Unlikely – could happen at some time
- Rare – may happen only in exceptional circumstances.
4. Step 3—How to control risks
The most important step in managing risks in-volves eliminating them so far as is reasonably practicable, or if that is not reasonably practicable, minimising the risks so far as is reasonably practicable.
In deciding how to control risks, as a person conducting a business or undertaking (PCBU), you must consult your workers and their representatives who will be directly affected by this decision. Their experience will help you choose appropriate control measures and their involvement will increase the level of acceptance of any changes that may be needed to the way they do their job.
There are many ways to control risks. Some control measures are more effective than others.
You must consider various control options and choose the control that most effectively eliminates the hazard or minimises the risk in the circumstances. This may involve a single control measure or a combination of different controls that together provide the highest level of protection that is reasonably practicable.
Some problems can be fixed easily and should be done straight away, while others will need more effort and planning to resolve. Of those requiring more effort, you should prioritise areas for action, focusing first on those hazards with the highest level of risk.
4.1 The hierarchy of control measures
The ways of controlling risks are ranked from the highest level of protection and reliability to the lowest as shown in Figure 2. This ranking is known as the hierarchy of control measures.
The hierarchy of control measures can be applied in relation to any risk. The WHS Regulations make it mandatory for duty holders to work through this hierarchy when managing certain risks.
You must always aim to eliminate the risk, which is the most effective control. If this is not reasonably practicable, you must minimise the risk by working through the other alternatives in the hierarchy.
The lower levels in the hierarchy are less effective because controls that change the hazard or minimise exposure to the hazard can only minimise the risk. You cannot eliminate the risk without eliminating the hazard.
Administrative controls and personal protective equipment (PPE) are the least effective at minimising risk because they do not control the hazard at the source and rely on human behaviour and supervision. These control measures should only be used:
- to supplement higher level control measures (as a back-up)
- as a short-term interim measure until a more effective way of controlling the risk can be used, or
- when there are no other practical control measures available (as a last resort).
Elimination
The most effective control measure involves eliminating the hazard and associated risk. The best way to do this is by, firstly, not introducing the hazard into the workplace. For example, you can eliminate the risk of a fall from height by doing the work at ground level.
Eliminating hazards is often cheaper and more practical to achieve at the design or planning stage of a product, process or place used for work. In these early phases, there is greater scope to design out hazards or incorporate risk control measures that are compatible with the original design and functional requirements. For example, not using a noisy machine will be more effective than providing workers with personal hearing protectors.
You can also eliminate risks by removing an existing hazard, for example, by removing trip hazards on the floor, disposing of unwanted chemicals, or not working in an isolated or remote area.
It may not be reasonably practicable to eliminate a hazard if doing so means that you cannot make the end product or deliver the service. If you cannot eliminate the hazard, then you must minimise as many of the risks associated with the hazard as reasonably practicable.
Substitution, isolation and engineering controls
If it is not reasonably practicable to eliminate the hazards and associated risks, you must minimise the risks using one or more of the following approaches, so far as is reasonably practicable
Substitute the hazard with something safer
For instance, replace solvent-based paints with water-based ones or allow workers to have more control of line speed instead of pacing line work by computer.
Isolate the hazard from people
This involves physically separating the source of harm from people by distance or using barriers. For instance, install guardrails around exposed edges and holes in floors; use remote control systems to operate machinery; store chemicals in a fume cabinet; place barriers between workers and customers where there is a risk of assault.
Use engineering controls
An engineering control is a control measure that is physical in nature, including a mechanical device or process. For instance, use mechanical devices such as trolleys or hoists to move heavy loads; place guards around moving parts of machinery; install residual current devices (electrical safety switches); set work rates on a production line to reduce fatigue; install sound dampening measures to reduce exposure to unpleasant or hazardous noise.
Administrative controls
If risks remain, they must be minimised by implementing administrative controls, so far as is reasonably practicable. Administrative controls include work methods or procedures that are designed to minimise exposure to a hazard as well as the information, training and instruction needed to ensure workers can work safely. For instance, develop procedures on how to operate machinery safely, provide training and support to managers and workers to identify and manage health and safety risks, implement anti-bullying policies, limit exposure time to a hazardous task, and/or use signs to warn people of a hazard.
Some administrative measures will be necessary to ensure substitution, isolation and engineering controls are implemented effectively, for example, following safe work procedures when using equipment. See section 4.2 below for information on implementing control measures.
Personal protective equipment
Any remaining risks must be minimised with suitable PPE. Examples of PPE include ear muffs, respirators, face masks, hard hats, gloves, aprons and protective eyewear. PPE limits exposure to the harmful effects of a hazard but only if workers wear and use the PPE correctly.
WHS regulation 44
Provision to workers and use of personal protective equipment
If PPE is to be used at the workplace, you must ensure the equipment is:
- selected to minimise risk to health and safety, including by ensuring that the equipment is suitable for the nature of the work and any hazard associated with the work and is of suitable size and fit and reasonably comfortable for the worker who is to use or wear it
- maintained, repaired and replaced so that is continues to minimise risk to the worker who uses it, including by ensuring that the equipment is clean and hygienic, and in good working order.
If you direct the carrying out of work, you must provide the worker with information, training and instruction in the proper use and wearing of PPE, and the storage and maintenance of PPE.
A worker must, so far as reasonably able, use or wear the PPE in accordance with any information, training or reasonable instruction and must not intentionally misuse or damage the equipment.
4.2 How to develop and implement control options
Information about suitable controls for many common hazards and risks can be obtained from:
- codes of practice and guidance material
- manufacturers and suppliers of plant, substances and equipment used in your workplace, or
- industry associations and unions.
In some cases, published information will provide guidance on the whole work process. In other cases, the guidance may relate to individual items of plant or how to safely use specific substances. You may use the recommended control options if they suit your situation and eliminate or minimise the risk.
Developing specific control measures
You may need to develop specific control measures if the available information is not relevant to the hazards and risks or circumstances at your workplace. This can be done by referring to the chain of events that were recorded during the risk assessment.
For each of the events in the sequence, ask: ‘What can be done to stop or change the event occurring?’ An example of this approach is shown in Appendix C.
Working through the events in the sequence will give you ideas about possible ways to eliminate or minimise the risk. There may be more than one solution for each of the events. The control option you choose should be:
- one or more controls that provide the highest level of protection for people and is the most reliable – that is, controls located towards the top of the hierarchy in Figure 2
- available – that is, it can be purchased, made to suit or be put in place, and
- suitable for the circumstance in your workplace – that is, it will work properly given the workplace conditions, work process and your workers.
Where the hazard or risk has the potential to cause death, serious injury or illness, more emphasis should be given to those controls that eliminate or reduce the level of harm, than those that reduce the likelihood of harm occurring.
Make sure that your chosen solution does not introduce new hazards. If this is not possible, any new hazards or risks introduced will also need to be managed.
You may prepare a risk register that identifies the hazards, what action needs to be taken, who will be responsible for taking the action and by when. An example is provided at Appendix D.
Cost of control measures
All risks can be controlled and it is always possible to do something, such as stopping the activity or providing instructions to those exposed to the risk. There will normally be a number of different options between these two extremes. Cost (in terms of time and effort as well as money) is just one factor to consider when determining the best control option.
The cost of controlling risk may be taken into account in determining what is reasonably practicable, but cannot be used as a reason for doing nothing.
The greater the likelihood of harm occurring or the greater the extent of that harm, the less weight should be given to the cost of controlling the hazard or risk.
If two control measures provide the same level of protection and are equally reliable, you can adopt the less expensive option.
Cost cannot be used as a reason for adopting controls that rely exclusively on changing people’s behaviour or actions when there are more effective controls available that can change the risk through substitution, engineering or isolation.
For further information, see the Interpretive Guideline: The meaning of ‘reasonably practicable’.
Implementing controls
The control measures you put into operation will usually require changes to the way work is carried out, for example, working with new or modified equipment or processes, new or different chemicals or new personal protective equipment. In these situations, it is necessary to support the control measures with the following.
Work procedures
Develop a safe work procedure that describes the task, identifies the hazards and documents how the task is to be performed to minimise the risks.
Training, instruction and information
Train your workers in the work procedure to en-sure that they are able to perform the task safely. Training must cover the nature of the work, the associated risks and the control measures to be implemented.
Training should require workers to demonstrate that they are competent in performing the task according to the procedure. It is insufficient to simply give a worker the procedure and ask them to acknowledge that they understand and are able to perform it. Training, instruction and information must be provided in a form that can be understood by all workers.
Information and instruction may also need to be provided to others who enter the workplace, such as customers or visitors.
Supervision
The level of supervision required will depend on the level of risk and the experience of the workers involved. High levels of supervision are necessary where inexperienced workers are expected to follow new procedures or carry out difficult and critical tasks.
Maintenance
Control measures need regular monitoring and maintenance to ensure they remain effective. You should decide what is required when you implement the control and establish a schedule for routine checks and maintenance appropriate to the controls.
You may prepare a risk register identifying the hazards, what action needs to be taken, who will be responsible for taking the action and by when. An example is provided at Appendix D.
4.3 How to ensure controls
remain effective
An important part of controlling risk is ensuring that your chosen control measures are maintained after their initial implementation. The following actions may help you monitor the control measures you have implemented and ensure that they remain effective.
Accountability for health and safety
Managers and supervisors should be provided with the authority and resources to implement and maintain control measures effectively. Ac-countability should be clearly allocated to ensure procedures are followed and maintained.
Maintenance of plant and equipment
This will involve scheduling and performing regular inspection and testing, repair or replacement of damaged or worn plant and equipment. It includes checking that any control measures are suitable for the nature and duration of work, are set up and used correctly.
Further information on maintaining plant and equipment is available in the Code of Practice: Managing the risks of plant in the workplace.
Up-to-date training and competency
Most control measures depend on workers and supervisors having the appropriate competencies to do the job safely. Training must be provided to maintain competencies and to ensure new workers are capable of working safely.
Up-to-date hazard information
Information about hazards, such as plant and substances, may be updated by manufacturers and suppliers and should be checked to make sure controls are still relevant. New technology may provide more effective solutions than were previously available. Changes to operating conditions or the way activities are carried out may also mean that control measures need to be updated.
Regular review and consultation
Control measures are more effective where there is regular review of work procedures and consultation with your workers and their representatives.
If maintenance processes reveal new hazards, or existing hazards that are not being addressed, you will need to perform a review of your control measures.
5. Step 4—How to review controls
The control measures you, as a person conducting a business or undertaking (PCBU), put in place should be reviewed regularly to make sure they work as planned. Don’t wait until something goes wrong.
The WHS Regulations require a risk management process for specific risks. That process includes circumstances where you must review your control measures for those risks and, if necessary, change them. A review is required:
- when the control measure is not effective in controlling the risk
- before a change at the workplace that is likely to give rise to a new or different health and safety risk that the control measure may not effectively control
- if a new hazard or risk is identified
- if the results of consultation indicate that a review is necessary, or
- if a health and safety representative requests a review.
In any case, as part of your ongoing duties as a PCBU, you should regularly review your control measures, including in the above circumstances. Managing work health and safety risks is an ongoing process that needs attention over time, but particularly when any changes affect your work activities.
You may use the same methods as in the initial hazard identification step (Chapter 2 – How to identify hazards) to check controls. Consult your workers and their health and safety representatives and consider the following questions:
- Are the control measures working effectively in both their design and operation?
- Have the control measures introduced new problems?
- Have all hazards been identified?
- Have new work methods, new equipment or chemicals made the job safer?
- Are safety procedures being followed?
- Have the instruction and training provided to workers on how to work safely been successful?
- Are workers actively involved in identifying hazards and possible control measures? Are they openly raising health and safety concerns and reporting problems promptly?
- Are the frequency and severity of health and safety incidents reducing over time?
- If new legislation or new information becomes available, does it indicate current controls may no longer be the most effective?
If problems are found, go back through the risk management steps (Chapter 4 How to control risks), review your information and make further decisions about risk control. Priority for review should be based on the level of risk. Control measures for high risks should be reviewed more frequently.
If you design, manufacture or supply products used for work, quality assurance processes may be used to check the product effectively minimises health and safety risks. Obtain feedback from users of the product to determine whether any improvements can be made to make it safer.
6. Keeping records
Keeping records of the risk management process demonstrates what you have done to comply with the WHS Act and WHS Regulations. It also helps when undertaking subsequent risk management activities, including reviewing your control measures.
Keeping records of the risk management process has the following benefits. It:
- allows you to demonstrate how decisions about controlling risks were made
- assists in targeting training at key hazards
- provides a basis for preparing safe work procedures
- allows you to more easily review risks following any changes to legislation or business activities, and
- demonstrates to others (regulators, investors, shareholders, customers) that work health and safety risks are being managed.
The detail and extent of recording will depend on the size of your workplace and the potential for major work health and safety issues. It is useful to keep information on:
- the identified hazards, assessed risks and chosen control measures (including any hazard checklists, worksheets and assessment tools used in working through the risk management process)
- how and when the control measures were implemented, monitored and reviewed
- who you consulted with
- relevant training records, and
- any plans for changes.
There are specific record-keeping requirements in the WHS Regulations for some hazards, such as hazardous chemicals, plant and equipment. If such hazards have been identified at your workplace, you must keep the relevant records for the time specified.
You should ensure that everyone in your workplace is aware of record-keeping requirements, including which records are accessible and where they are kept.

Kampf, A., McSherry, B., Rothschild, A., & Ogloff, J. (2010). Ethical decision-making in confidentiality dilemmas. In Confidentiality for mental health professionals (pp. 93-116). Australian Academic Press.
Lack of awareness or misunderstanding of an ethical standard is not itself a defence to an allegation of unethical conduct. (Australian Psychological Society, Code of Ethics, p. 10)
As any mental health professional knows, it is one thing to review ethical and legal principles in the abstract and quite another to rely on them to make decisions when actual situations arise. The appropriate course of conduct and decision-making is governed by a variety of influences, including legal principles and ethics codes. Samuel Knapp and Leon VandeCreek (2003), in introducing their book on the 2002 revision of the American Psychological Association’s Ethics Code, state: ‘Ethics Codes of professions are, by their very nature, incomplete moral codes’ (p. 7). Drawing on the information covered so far in this book, the aim of this chapter is to move from the abstract to the concrete, and in so doing model decision-making processes for mental health professionals to assist them in dealing with issues pertaining to confidentiality. To achieve this aim, two situations are identified in which mental health professionals face ethical dilemmas in relation to client or patient confidentiality.
The first situation pertains to a request for a psychiatrist to release information about a patient to the patient’s employer. In the second case, the clinician wrestles with issues pertaining to the patient’s risk of harm to third parties. Once the cases have been presented, information is provided to work through the dilemmas using a model for ethical decision-making presented in Figure 7.1. It is hoped that these exercises will assist mental health professionals to incorporate a systematic decision-making framework in their consideration of confidentiality-related ethical dilemmas. The exercises will also provide a good opportunity to learn how the principles that have been discussed throughout this book apply to actual dilemmas.
It is necessary to note a few general matters before proceeding. First, by their very nature, ethical dilemmas may not always have a single ‘correct’ outcome. Rather, some number of alternatives will inevitably arise to address such matters. Each alternative will have strengths and weaknesses. It is incumbent upon mental health professionals, therefore, to explore the options available and to evaluate the consequences and implications of each one before deciding how to proceed.
While it is possible that the decision reached by the mental health professional ends up being the ‘wrong’ decision, it is far worse, legally and professionally, to be negligent by not having gone through a careful decision-making process before arriving at a decision.
Second, as has been the case throughout this book, the challenge exists to state both principles that cover the law and ethical principles relevant to the different mental health professionals across different circumstances. As always, it is incumbent upon mental health professionals to be familiar with the code of ethics and their underlying values and principles governing their professions when considering ethical matters. Moreover, it is helpful for mental health professionals to have a working understanding of the relevant legal principles pertaining to confidentiality to guide their practices. The previous chapters have set out the relevant ethical and legal principles. As always, though, the information provided in considering the ethical dilemmas in this chapter is general in nature.
Third, it is important and helpful to seek professional advice from colleagues, superiors, professional bodies, indemnity insurers and legal counsel to assist in decision-making. Of course, time permitting, the more serious the situation, the longer the consultation should be. It is also prudent to document the information and advice received.
A Model for Ethical Decision-Making
Mental health professionals, who may be highly skilled and knowledgeable in their fields, often approach matters that require ethical decision-making in an unsystematic and unsophisticated manner. Very often, by using a systematic model of decision-making, the most appropriate resolution of ethical dilemmas becomes apparent.
In reviewing a number of different ethical decision making models for mental health professionals, Samuel Knapp and Leon VandeCreek (2003) identify five steps shared by the various approaches:
- identification of the problem;
- development of alternatives;
- evaluation of alternatives;
- implementation of the best option; and
- evaluation of the results.
In addition to these steps, Knapp and Vande-Creek propose that additional steps or factors are required to deal with emotional and situational factors, and point to the need for an immediate response in emergency situations. With respect to decision-making in emergency situations, the authors wisely suggest that mental health professionals should anticipate the sorts of ethical situations that may arise and develop ethical action plans to implement should the need arise. Without such already-established plans it may be too late or difficult to reasonably consider alternatives prior to needing to act in an emergency situation.
A useful model for decision-making that will be employed in this chapter is based on the model developed by Shane Bush, Mary Connell and Robert Denny (2006) as well as the work of the Canadian Psychological Association (2001). Drawing on the work of Knapp and Vande-Creek (2003), Bush, Connell and Denny incorporate the five general steps noted above into their model. In addition, they outline the following three steps:
- consider the significance of the context and setting;
- identify and use ethical and legal resources; and
- consider personal beliefs and values.
The Canadian Psychological Association (2001) adds that the individuals and groups potentially affected by the decision should be identified and that the problem should be construed in accordance with the relevant ethical issues and practices being considered. Incorporating all of these steps, the model to be used in this chapter is presented in Figure 7.1. The steps will be defined as the example cases are resolved.
![[ADD IMAGE'S ALT TEXT]](/sites/default/files/Figure%207.1_2.png)
Sample Case Scenarios
In this section, two sample cases are presented. More detail will be provided as we work through the first case since this provides the first opportunity for practical application of the information pertaining to confidentiality reviewed throughout this book. Less detail will be required in the second case since the overarching principles will have been addressed in greater detail in the initial case.
For both case scenarios, Figure 7.1 should be referred to in order to see how the decision-making model and the questions posed throughout it are employed to guide the decision-making process. The aim of these exercises is to help you apply the information from this book in order to resolve actual dilemmas that may arise in your own practice.
Case 1: Requests for Obtaining Confidential Client Information
When Belinda was 17 years old she was admitted to the local Child and Adolescent Mental Health Service. Her parents reported that she was acting strangely, believing things that were not true. She was paranoid, became estranged from her friends and was reclusive. Upon examination, she was diagnosed with a psychotic illness not otherwise specified. Over time, the psychiatrist who treated her, Dr Waters, believed she had experienced the first episode of a schizophrenic illness. Belinda was in hospital for three weeks. Her symptoms stabilised and she was able to return home. She continued to see the mental health service on an outpatient basis. In the intervening two years, Belinda was hospitalised on three occasions. From the time she was 19 years old until she was 23, she had no further periods of hospitalisation, but was treated by Dr Waters on an outpatient basis.
Belinda was well enough to work and she obtained employment as a clerk in a department store. Things went well for her for several months and she was promoted to a supervisory position. Soon after, she began to deteriorate. She was once again paranoid and was unable to go to work. When she missed work, she obtained a medical certificate from Dr Waters, in-dicating she was unwell. As is the usual case, Dr Waters did not write the nature of Belinda’s illness on the note; however, the letterhead on which the note was written indicated that Dr Waters was a psychiatrist.
When Belinda returned to work, the human resources manager asked to see her. Given that Belinda had acted strangely at work before she took time off, the human resources manager wanted to ensure she was fit to work. Belinda assured her that she was but declined to discuss the nature of her illness. She returned to work.
From the medical certificate Belinda provided, the human resources manager knew that she had been in the care of a psychiatrist. To allay her concerns, the manager telephoned Dr Waters, having obtained the telephone number from the certificate. The human resources manager told Dr Waters that Belinda worked for the store and that she was concerned about her capacity for work. The manager stated further that if she could not confirm that Belinda was fit to work, the store would be forced to let her go. Dr Waters wanted to be supportive of Belinda to help her keep her job.
How should the psychiatrist proceed?
Drawing on the decision-making model outlined in Figure 7.1, Case 1 will be analysed and resolved below.
Defining the Problem
The first four steps of the decision-making model provide an opportunity for the clinician to carefully define the nature and scope of the problem, as well as identify the resources necessary and available to assist them in resolving the dilemma. Each of these steps will be reviewed in turn.
Step 1: Identify the Individuals and Groups Potentially Affected by the Decision
In this dilemma, first and foremost Belinda, as the traditional patient or client, will be affected by Dr Waters’ decision. Second, Belinda’s employer may be affected by the decision. Third, Dr Waters will of course be affected by the decision and what she decides could affect the therapist-patient relationship she has with Bel-inda. Finally, although it is not specified in the scenario description, other individuals such as Belinda’s family members or dependents may be affected by Dr Waters’ decision.
Step 2: Identify the Problem, Including the Relevant Ethical and Legal Issues and Clinical Practices
Given that this book focuses on confidentiality, it almost goes without saying that confidentiality is the central ethical and legal issue in this and all of the other scenarios. Specifically, though, the ethical issue is whether Dr Waters should share information regarding her opinion of Belinda’s capacity to work with the human resources manager. The legal issue is whether the information Dr Waters has regarding Belinda’s health is protected under the state privacy legislation and, if so, whether and under what circumstances the information may be shared with the manager.
Step 3: Consider the Significance of the Context and the Settings
The situation is one in which the human resources manager is requesting information that is not consistent with the purpose for which it was initially collected – that is, for the health care of Belinda. The context in which the manager is seeking the information is highly unusual. To the extent that the employment is important to Belinda, however, the situation is significant. It is also worth noting that this situation is not an emergency.
Step 4: Identify and Use Relevant Legal, Ethical and Professional Resources
Dr Waters has a number of resources at her disposal:
- the relevant ethics code provisions:
- ‘Psychiatrists shall hold clinical information in confidence’ (The RANZCP Code of Ethics, Principle 4);
- ‘Confidentiality cannot always be absolute. A careful balance must be maintained between preserving confidentiality and the need to breach it rarely in order to promote the patient’s best interests and/or safety and welfare of other persons’ (The RANZCP Code of Ethics, Principle 4.5).
- the relevant Privacy Act and any other related Acts (e.g., Health Records Act) in her state;
- she can raise the matter with colleagues for advice;
- she can contact her medical indemnity insurer for legal advice; and
- she can consult a lawyer.
For the purposes of these exercises, it is assumed that in the information gathering phase, mental health professionals will have had an opportunity to explore their options for action with the various people noted above, and that they will have relied on the other resources as well.
Considering Options
Step 5: Develop and Consider Alternative Solutions to the Problem
Step 5 requires the clinician to begin to consider the alternative solutions to the dilemma. In demonstrating this process, we will review the relevant principles as we discuss the possible courses of action that Dr Waters may choose to follow.
Alternative 1: Do Not Disclose the Information
The general rule in considering matters pertaining to confidentiality is that the information obtained in the course of a clinical service is confidential. As such, the clinician must not share information about the patient or client, or even acknowledge that the individual is or has been their patient or client. As the ethical principles quoted above make clear, however, ‘confidentiality cannot always be absolute’. Thus Dr Waters will need to determine whether Belinda’s situation is such that an exception to the general rule might apply.
The usual circumstances in which confidential health care information may be shared occur when the purpose for sharing the information is consistent with the reason the information was initially obtained. In Belinda’s situation, she has obtained psychiatric care from Dr Waters to treat her psychiatric illness. Given that the request by the human resources manager to obtain information about Belinda’s care is to satisfy employment demands, the request is not consistent with the original purpose for which the information was obtained. Using this rationale, the first alternative is for Dr Waters to refuse to share the information with the human resources manager. Moreover, since the clinical relationship between Dr Waters and Belinda is confidential, Dr Waters may decide not to even acknowledge that Belinda is her patient.
Based on this alternative, Dr Waters may respond to the human resources manager: ‘I am not in a position to even confirm that the person you are asking about is a patient of mine and certainly I would be unable to disclose any information to you about her, even if she was a patient of mine.’
Analyse risks and benefits of this course of action. The risk of this course of action is that Belinda may end up losing her employment because the human resources manager has not been assured that Belinda is fit to work. The benefit, however, is that Dr Waters will have protected Belinda’s privacy by not revealing any information about the therapeutic relationship or any health information about Belinda. Moreover, by Dr Waters holding Belinda’s information in confidence, she will ensure that Belinda trusts her, which will in turn protect the therapeutic relationship.
Consider how your personal beliefs, values and biases may affect your decision-making. In this scenario, Dr Waters has been providing psychiatric care to Belinda for several years; therefore, she will doubtless want to help Belinda. As such, it may be tempting to engage in a dialogue with the human resources manager to help protect Belinda by saving her job. Thus it will be tempting to share relevant information in a way that would serve to help Belinda maintain employment.
Alternative 2: Share the Information
While the first alternative may initially seem to be the only ‘correct’ course of action, the matter is perhaps more complicated than it first appears. Indeed, the language from the ethical principles for psychiatrists is somewhat broad, providing that ‘A careful balance must be maintained between preserving confidentiality and the need to breach it rarely in order to promote the patient’s best interests and/or safety and welfare of other persons’ (The RANZCP Code of Ethics, Principle 4.5). Dr Waters may need to ask whether it is in the ‘best interests’ of Belinda or other persons that she lose her job.
Further, it may be argued that Belinda waived her right to complete confidentiality when she requested that Dr Walters prepare the medical certificate that she submitted to her employer (that is, she implicitly consented to share information indicating that she was unwell and being treated by a psychiatrist). This is particularly the case since the letterhead indicated that Dr Waters is a psychiatrist. However, the information in the letter was limited in scope so that the extent to which the confidential information was shared was also limited.
Dr Waters is concerned that Belinda may lose her job, which has been an important part of her recovery. She realises that the human resources manager was calling to follow-up the medical certificate she completed. In this alternative, if she believes that it is in Belinda’s best interests not to lose her job, Dr Waters may elect to provide information to the human resources manager to assure her that Belinda is fit for work. A complication would occur, of course, if Dr Waters does not believe that Belinda is fit for work and that the work would detrimentally affect her psychiatric wellbeing.
Analyse risks and benefits of this course of action. The risk with this course of action is that by electing to communicate with the human resources manager about Belinda, Dr Waters has violated Belinda’s confidentiality. The benefit with this alternative is that Dr Waters believes she is protecting Belinda’s employment.
Consider how your personal beliefs, values and biases may affect your decision-making. Dr Waters’ beliefs and values will influence her decision-making. It is apparent that she is balancing her obligation to protect Belinda’s privacy and the confidentiality of her treatment against the need to assure the human resources manager that Belinda is able to work, despite her illness.
Alternative 3: Compromise by Deferring the Decision to Belinda
Drawing on the need to balance two or more competing interests, which is typical in resolving ethical dilemmas, Dr Waters may contemplate a third alternative, one that offers a compromise to the first two courses of actions discussed. For this alternative, Dr Waters realises that she owes a duty of confidentiality to Belinda and that to share any information with the human resources manager may be seen as a violation of that duty. Although she did prepare the medical certificate, at Belinda’s request, Dr Waters took care not to state the nature of the illness. From the letterhead the human resources manager discovered that Belinda was being treated by a psychiatrist, but that was the limit of the confidential information that was shared to that point.
The human resources manager clearly has concerns about Belinda’s fitness to return to work. Therefore, Dr Waters may decide that since Belinda essentially holds the right of confidentiality, it must be her decision whether to allow Dr Waters to share any information with the manager. The extent to which patients value confidentiality varies, and it likely varies across situations as well. For example, while people may share confidential information with their friends, they may choose not to do so with their coworkers or employers. Therefore, it is always prudent, if possible, to check with patients to obtain an explicit indication of the value they place on confidentiality in particular situations.
For this third alternative, Dr Waters may decide to let the human resources manager know that she is unable to discuss any information pertaining to Belinda without first contacting her to seek her consent. Dr Waters could then contact Belinda to let her know that the human resources manager has been in touch. Dr Waters could engage Belinda in a dialogue about what, if any, information should be shared with the manager. They could agree on the limitations of confidential information that would be shared. For example, they could agree that Dr Waters would not reveal that Belinda has been diagnosed with schizophrenia or how she is being treated. Assuming Dr Waters believes that Belinda is now fit for work, they could agree that Dr Waters simply inform the human resources manager that Belinda has been in her care but has now recovered and is able to work. They could also agree that Dr Waters could further inform the manager that she will continue to see Belinda to assist her in maintaining her wellbeing. Dr Waters could also suggest that the manager contact Belinda to discuss the matter directly with her.
It is the case with this alternative that should Belinda decide she does not consent to Dr Waters sharing any information about her, Dr Waters will have to respect her wishes and not provide any information to the human resources manager.
Analyse risks and benefits of this course of action. This course of action minimises the risk of Belinda losing her job since the human resources manager could be assured that she is fit for work. Similarly, this alternative reduces or eliminates the risk of Dr Waters violating Belinda’s right to confidentiality by revealing confidential information to the human resources manager without her consent. The benefit of this course of action is, therefore, that Belinda is likely to maintain her employment, assuming the human resources manager is content with the information shared by Dr Waters, with the minimum disclosure of Belinda’s confidential health care information. Moreover, given protections afforded under legislation to people with disabilities, including mental illnesses, it would be difficult for the employer to dismiss Belinda due to a mental illness, as long as she was able to satisfactorily carry out her employment duties.
Consider how your personal beliefs, values and biases may affect your decision-making. For this course of action, Dr Waters’ feelings of obligation to her patient can be respected while still helping to achieve the goal of assisting Belinda to maintain her employment.
Step 6: Choose the Most Appropriate Outcome
Alternative 3 appears to be the most appropriate course of action, particularly where the psychiatrist believes that Belinda is fit for work. This alternative allows the psychiatrist to share a limited amount of information, as agreed to by Belinda, to help preserve Belinda’s employment. As such, the confidential information Belinda does not want shared – including, perhaps, the nature of the illness and other personal details – is held in confidence. Yet, enough information is shared with the human resources manager to hopefully preserve Belinda’s employment.
Monitoring
Step 7: Monitor and Assess the Outcome Chosen
Having decided to proceed with the third alternative described above, Dr Waters would need to begin to implement the plan. She would need to contact Belinda and explain the options available to her. Assuming Belinda would consent to Dr Waters sharing the limited information with the human resources manager, Dr Waters could then contact the manager. Dr Waters would need to monitor whether the limited information Belinda has agreed to share – that she has a mental illness for which she has been successfully treated, that Dr Waters believes she is fit for work and that Dr Waters will continue to treat and monitor her – would satisfy the human resources manager at this point. If not, Dr Waters will need to reconsider her decision.
Resolving the Problem
Assuming Belinda and the human resources manager are satisfied with the planned course of action, the ethical dilemma should be resolved satisfactorily.
Step 8a: Consider the Need for an Ethical Action Plan or Practice Modification
Dr Waters would need to consider that when patients request medical certificates or letters for employers, they should be informed of the possibility that the employer may then learn that they have been in the care of a psychiatrist. This would hold true for other mental health professionals as well. In many circumstances, the patient could then opt to ask a general practitioner to prepare the certificate, given that most often the general practitioner and specialist mental health professional will be in communication about the patient’s situation. If the pa-tient does not mind the employer learning that they have been cared for by a mental health professional, then the mental health professional should discuss with the patient the nature of information to be shared in the medical certificate or note.
Step 8b: Repeat Steps 5-7
Steps 5 to 7 would need to be revisited if in the course of implementing or monitoring the situation Dr Waters realised that the plan was unsuccessful or inappropriate.
Case 2: Divulging Confidential Information to Protect Third Parties
Sebastian was a voluntary patient at the local Community Mental Health Service where he was seen regularly by Dr Suresh, a clinical psychologist. Sebastian was 31 years old and had a history of psychiatric illness. He received a disability support pension and lived in supported accommodation. While Sebastian had a history of making threats and becoming enraged, the psychologist did not believe that he had ever assaulted anyone. Similarly, although he was uncertain, the psychologist did not believe that Sebastian had a criminal history. Sebastian had a history of self-harm, including an occasion 18 months ago when he was rescued by staff after cutting his wrists and overdosing on benzodiazepines.
Dr Suresh found that, over the past three months, Sebastian was finding it increasingly difficult to control his anger. In particular, he was making threats to harm others. While the threats were diffused, he had targeted a young man, Adam, who had been living in the same accommodation until two weeks ago.
On the most recent occasion that Dr Suresh saw Sebastian, he was guarded on interview and initially downplayed the level of anger and distress he was experiencing. He exhibited delusional thinking, believing that others had targeted him and were conspiring against him. This was consistent with his past history of symptoms while he was unwell, although Sebastian had not verbalised such thoughts for more than two years.
Consistent with previous paranoid thinking, Sebastian expressed the belief that some co-residents were ‘spies’, placed there to monitor him. Over time, he admitted that he felt as though he was ‘at the end of his rope’ and ready to give up. He felt he was destined to end his own life. Again, this was consistent with previous suicidal thinking evidenced by Sebastian. However, unlike previous occasions, Sebastian discussed a desire to ‘take someone with him’ this time. When Dr Suresh queried this thinking, Sebastian replied that ‘they’ had caused him so much pain, he wanted them to know how he felt when he was targeted. Initially Sebastian denied having any particular person in mind. When pressed, though, Sebastian named the young male co-resident Adam, whom he had previously targeted.
Dr Suresh employed the HCR-20 violence risk assessment measure (Webster, Douglas, Eaves, & Hart, 1997) to assist with determining Sebastian’s level of risk for engaging in violence. Based on the information available, Dr Suresh formed the belief that at the present time he posed a high risk of harm to others and, in particular, to the co-resident Sebastian named Adam.
How should the psychologist proceed?
Defining the Problem
As discussed with Case 1, the decision-making model requires the clinician to carefully define the nature of the dilemma, including the significance and context of the situation. These initial steps also make mental health professionals evaluate the legal, ethical and professional resources available and required to resolve the dilemma.
Step 1: Identify the Individuals and Groups Potentially Affected by the Decision
Dr Suresh has an ongoing, voluntary, therapeutic relationship with Sebastian. As such, Sebastian will be clearly affected by Dr Suresh’s decision. The former co-resident whom Sebastian has targeted may also be affected by Dr Suresh’s decision. As always, the clinician, Dr Suresh, will be affected by the decision, particularly in light of his relationship with Sebastian.
Step 2: Identify the Problem, Including the Relevant Ethical and Legal Issues and Clinical Practices
Although the case pertains – broadly speaking – to confidentiality, the narrow ethical issue to be addressed in this scenario is whether Dr Suresh should use information held in confidence to try to ‘protect’ the third party, Adam. There is a related legal issue: could Dr Suresh and/or the mental health service for which he works be civilly liable should he decide to protect Sebastian’s confidentiality and Sebastian attacks and injures Adam? Conversely, there is a risk that Sebastian might take legal action against Dr Suresh and the mental health service if Dr Suresh decides to violate his confidentiality, and Sebastian believes it was wrongfully done. However, if Dr Suresh warns Adam or takes any measures to control Sebastian, Sebastian might lose his trust in Dr Suresh and no longer talk with him about why he is experiencing anger and distress.
Step 3: Consider the Significance of the Context and the Settings
Given Dr Suresh’s conclusion that ‘at the present time he posed a high threat of harm to others and, in particular, to the co-resident Sebastian named – Adam’, the situation is serious. Indeed, Sebastian may cause harm to Adam or to someone else. Of concern as well is that should Dr Suresh violate Sebastian’s confidentiality, their therapeutic relationship may be irrevocably harmed. The context is that Sebastian has been deteriorating and has expressed suicidal and homicidal ideation. This is in light of Sebastian’s ongoing psychiatric illness.
Step 4: Identify and Use Relevant Legal, Ethical and Professional Resources
In this situation, Dr Suresh may consider the following:
- the relevant Australian Psychological Society ethics code provisions, which are as follows:
- ‘Psychologists safeguard the confidentiality of information obtained during their provision of psychological services’ (The APS Code of Ethics , Standard A.5.1)
- ‘Psychologists disclose confidential information obtained in the course of their provision of psychological services only under any one or more of the following circumstances … (c) if there is an immediate and specified risk of harm to an identifiable person or persons that can be averted only by disclosing information’ (The APS Code of Ethics, Standard A.5.2)
- ‘Psychologists inform clients at the outset of the professional relationship, and as regularly thereafter as is reasonably necessary, of the: (a) limits to confidentiality; and (b) foreseeable uses of the information generated in the course of the relationship’ (The APS Code of Ethics, Standard A.5.3)
- ‘When a standard of this Code allows psychologists to disclose information obtained in the course of the provision of psychological services, they disclose only that information which is necessary to achieve the purpose of the disclosure, and then only to people required to have that information’ (The APS Code of Ethics , Standard A.5.4)
- ‘Psychologists ensure consent is informed by: … (h) explaining confidentiality and limits to confidentiality’ (The APS Code of Ethics, Standard A.3.3)
- the Privacy Act in his State
- raising the matter with colleagues for advice
- contacting his professional indemnity insurer
- consulting a lawyer, including the legal department representing the mental health service.
Once again, for the purposes of these exercises, it is assumed that Dr Suresh will have had an opportunity to explore his options for action with the various people noted above, and that he will have relied on the other resources as well.
Considering Options
Step 5: Develop and Consider Alternative Solutions to the Problem
Alternative 1: Do Not Disclose the Information
For the first alternative course of action, it is al-ways useful to consider the effect of maintaining confidentiality. As indicated above, the general principle regarding confidentiality, as reflected in The APS Code of Ethics, is that ‘(p)sychologists safeguard the confidentiality of information obtained during their provision of psychological services ‘(Standard A.5.1). Adhering to this general rule, Dr Suresh might choose to continue treating Sebastian with the aim of helping him to manage his risk through treatment. Based on this alternative, Dr Suresh may wish to increase the frequency of his contact with Sebastian to help manage the risk.
Analyse risks and benefits of this course of action. The risk of this course of action, obviously, is that Sebastian may end up causing harm to someone, particularly Adam. Because Dr Suresh has recognised that Sebastian poses a ‘high risk’ of causing harm to others, he may feel professionally responsible for not doing more to protect others, and for ensuring that Sebastian does not detrimentally affect his own life by harming others. In addition, as pointed out in chapter 5, although there is no common law ‘duty to protect’ third parties in Australia, it is conceivable that given the right set of facts, a court could find that a therapist is liable for the harm that ensues as a result of the foreseeable actions of a psychiatric patient.
While it is possible that some risks might arise from Dr Suresh’s decision to maintain confidentiality and to continue to treat Sebastian, some possible benefits might also unfold. In particular, Dr Suresh will be able to maintain a therapeutic relationship with Sebastian. This relationship, and the treatment that Dr Suresh could provide, might serve to reduce Sebastian’s level of risk while helping to ensure a stable, long-term therapeutic relationship. Finally, Dr Suresh’s decision to maintain confidentiality is consistent with The APS Code of Ethics, which does not require a psychologist to share confidential information to protect third parties, but allows them to do so.
Consider how your personal beliefs, values and biases may affect your decision-making. Dr Suresh will doubtless have a desire to preserve the therapeutic relationship with Sebastian. How-ever, in trying to preserve the relationship, he may be overly confident in his ability to monitor Sebastian and prevent him from causing harm to a third party. Thus, Dr Suresh will need to keep an open mind about the likelihood that he will be able to provide adequate treatment and monitoring to manage Sebastian’s risk. Dr Suresh will also need to consider his own attitudes towards the police and other relevant authorities in deciding how to proceed.
Alternative 2: Share the Information to Protect Third Parties
Dr Suresh could consider taking steps beyond ongoing treatment to reduce Sebastian’s risk of harming Adam, or other people. To accomplish this, he may consider breaching information held in confidence to try to contain the level of risk that he believes Sebastian presents, thereby protecting Adam. To this end, Dr Suresh may elect to contact the police or other authorities to share his concern that Sebastian may harm others. In addition, he may decide to try to contact Adam to let him know that he may be targeted by Sebastian for harm.
When deciding to undertake this course of action, Dr Suresh would need to consider whether he is in fact violating Sebastian’s confidentiality. For example, The APS Code of Ethics, Standard A.3.3, requires that ‘(p)sychologists ensure consent is informed by: … (h) explaining confidentiality and limits to confidentiality’. Moreover, The APS Code of Ethics, Standard A.5.3, provides that ‘ (p)sycholgists inform clients at the outset of the professional relationship, and as regularly thereafter as is reasonably necessary, of the: (a) limits to confidentiality; and (b) foreseeable uses of the information generated in the course of the relationship’.
In accordance with these standards, if Dr Suresh informed Sebastian as part of the initial informed consent process that he may need to share confidential information should Sebastian present a risk of harm to identified third parties, then electing to share the information to protect the third party will not be seen as an improper breach of confidentiality. This is particularly true if Dr Suresh reiterated the fact that the information discussed may not be held in confidence once Dr Suresh commenced evaluating Sebastian for the purpose of the risk assessment.
Specifically, The APS Code of Ethics, Standard A.5.2, considers the grounds upon which information may be disclosed by psychologists as follows:
(p)sychologists disclose confidential information obtained in the course of their provision of psychological services only under any one or more of the following circumstances… (c) if there is an immediate and specified risk of harm to an identifiable person or persons that can be averted only by disclosing information.
Thus, to disclose the confidential information to the police and/or to Adam (if Dr Suresh can contact him) requires Dr Suresh to be satisfied that not only is there a high risk of harm, but that the harm is ‘imminent’, the third party to be protected is identified and the risk of harm can only be averted by the psychologist disclosing the information.
Finally, once the psychologist makes a decision to share the confidential information, the psychologist must ‘disclose only that information which is necessary to achieve the purpose of the disclosure, and then only to people required to have that information’ (The APS Code of Ethics, Standard A.5.4). As such, Dr Suresh might inform the police of something similar to the following:
I am a psychologist employed by X service. I have a patient, Sebastian [surname], whose behaviours have been escalating and I believe he presents a high risk of harming an identifiable person (Adam [surname]). He has a mental illness that is contributing to this condition. As a result, it is my opinion that he may harm someone, most likely Adam, whom he has targeted.
In addition to the above, the psychologist could share details about the patient’s address, but must not share information about the particular nature of Sebastian’s mental illness or any other information obtained in confidence that is not relevant for the police to assist with Dr Suresh’s request to help protect Adam.
Analyse risks and benefits of this course of action. There are a number of risks associated with this course of action. First, it is questiona-ble what the police would be able to achieve. While they do have powers under all of the state and territory mental health Acts to apprehend people who they believe are mentally ill and require treatment to protect them from harming themselves or others, police have few other options for how to proceed in cases where people are making vague threats to harm others. Second, Sebastian may become angry with Dr Suresh and refuse to continue to see him therapeutically. Similarly, Sebastian’s trust in mental health professionals, generally, may be affected. Third, although Dr Suresh has judged Sebastian as being a high risk of harming others, that does not mean Sebastian will actually end up harming anyone. Thus, the therapeutic relationship – and Sebastian’s confidence in mental health professionals – may be jeopardised unnecessarily. Finally, should Dr Suresh decide to share some of the confidential information pertaining to Sebastian, Sebastian may make a complaint, or take legal action, against Dr Suresh for breach of confidentiality.
The benefit of this action is that Dr Suresh may be able to help Sebastian contain his level of risk by having the police become involved. This, in turn, may help to protect Adam, assuming Sebastian would have engaged in violent or threatening behaviour against him. Moreover, this course of action would be in accordance with Dr Suresh’s ethical obligations.
Consider how your personal beliefs, values and biases may affect your decision-making. Dr Suresh will need to monitor his own beliefs, values and biases to help ensure that his decision to disclose confidential information is made independent of his own biases. For example, he will need to consider whether his decision to share the confidential information is based on any of his own biases. For example, is he afraid of Sebastian, or does he mistakenly believe that mentally ill people are always violent?
Alternative 3: Compromise to Help Manage Sebastian’s Level of Risk
For this alternative, Dr Suresh may consider a situation where he chooses to arrange for an involuntary hospital admission for Sebastian. In this scenario, Dr Suresh may elect to share confidential information about Sebastian in order to help arrange a period of involuntary hospitalisation. To this end, Sebastian may draw upon a psychiatrist member of his team to arrange for an involuntary hospitalisation. Dr Suresh will need to share enough information with the treating psychiatrist to assist him or her with making a determination about whether Sebastian might meet the criteria for involuntarily hospitalisation.
The mental health Acts across the states require that a medical practitioner (and sometimes other health practitioners) needs to examine the individual to determine whether, in their professional opinion, the patient suffers from a mental illness, presents a risk of harm to himself or herself or others, or is unable to care for himself or herself or will deteriorate significantly without the involuntary treatment.
As with the second alternative, Dr Suresh’s actions as described here would not contradict his ethical obligations if he ensures that the risk is imminent, the victim is identifiable and the risk cannot be averted by some other means that would not necessitate breaking confidentiality. He would also need to ensure that the only information revealed is that which is necessary to assist the psychiatrist with obtaining the information necessary to conduct an assessment of the patient’s suitability for involuntary hospitalisation.
Analyse risks and benefits of this course of action. There are two general risks associated with this proposed course of action. First, it may not ultimately serve to protect third parties from Sebastian since he may not be found eligible for involuntary hospitalisation (although this is unlikely given the facts, Sebastian’s history of psychiatric illness and Sebastian’s current symptoms). Second, Sebastian may take offence with Dr Suresh’s decision to share confidential information with others in order to protect possible third parties. The benefits of this action are that Sebastian may in fact be hospitalised or treated on a community-based order that assists him to restore his mental well-being over time, thereby also reducing the level of risk he poses to third parties including Adam. The related benefit is that while Dr Suresh is sharing some information obtained in confidence, the information is being shared to assist Sebastian in his care – not to warn the police in order to somehow protect third parties including Adam. Also, the information Dr Suresh is sharing is shared with a psychiatrist who is also obliged to maintain confidentiality.
Consider how your personal beliefs, values and biases may affect your decision-making. Considerations in this section are similar to those discussed for the previous two alternatives. For this alternative, Dr Suresh will have to consider his own views regarding involuntary treatment. Some people have misgivings about compelling treatment, which is typically forced medication. Dr Suresh would have to consider the extent to which any such views are balanced against the need to reduce the likelihood that Sebastian may harm Adam, or some other person.
Step 6: Choose the Most Appropriate Outcome
On balance, the first alternative, to maintain confidentiality and to try to reduce Sebastian’s risk by continued treatment, is unlikely to be suitable given Dr Suresh’s own conclusion that Sebastian poses a high risk of harm to others, particularly Adam. Dr Suresh’s ability to treat Adam satisfactorily given the description of his presentation and mental state is tenuous at best.
While the first alternative course of action discussed may not be sufficient to avert harm, the second course of action may be too extreme under the circumstances. Given Sebastian’s history and mental state, particularly in light of his current behaviour and di, ordered thinking, he would likely meet the criteria for involuntarily hospitalisation. As such, contacting the police or informing the intended victim, Adam, of the pending risk would not be seen to be the only means by which the ‘immediate and specified risk of harm’ to Adam could be ‘averted’. Indeed, Sebastian is a known patient to the mental health service where Dr Suresh works. Dr Suresh would have ready access to psychiatrists or other suitable medical practitioners such as registrars or advanced trainees who can assist with a determination of whether involuntary hospitalisation or at least a community-based order is appropriate. Of course, if involuntary hospitalisation is not possible, or Sebastian’s risk of harm to Adam could not be contained and eventually reduced through involuntary treatment and/or hospitalisation, Alternative 2 may become necessary.
Based on the considerations above, the third course of action would appear to satisfy Dr Suresh’s need to reduce Sebastian’s level of risk to protect Adam, while still preserving must of the confidential information revealed in the therapeutic relationship. Moreover, the purpose for which the confidential information was obtained through the therapeutic relationship – that is, to assist Sebastian with his mental and psychological wellbeing – is quite consistent with the ongoing provision of mental health treatment to Sebastian, albeit involuntary.
Monitoring
Step 7: Monitor and Assess the Outcome Chosen
Monitoring would be necessary and helpful in this situation to ensure that Sebastian’s level of risk is being managed and that, whichever alternative course of action is in place, Adam is not likely to be harmed.
Resolving the Problem
If Sebastian’s level of risk is managed and reduced without him causing harm to Adam, or other third parties, then the immediate problem will be resolved. If not, the information below will need to be considered to modify the plan of action.
Step 8a: Consider the Need for an Ethical Action Plan or Practice Modification
First, there is a need to ensure that Sebastian’s level of risk is being managed and hopefully reducing. Second, should it be found that Sebastian does not satisfy the requirements for involuntary hospitalisation or treatment, Alternative 2 would need to be reconsidered and likely adopted. Third, even with treatment, Sebastian’s level of risk to Adam may not reduce sufficiently prior to discharge, thereby necessitating the consideration of following the second alternative.
Step 8b: Repeat Steps 5-7
Steps 5 to 7 would need to be reconsidered if in the course of monitoring the situation it was found that the plan was not successful or appropriate.
Conclusions
As suggested by the information presented in this chapter, employing a comprehensive decision-making model to assist with considering ethical dilemmas provides a useful mechanism for mental health professionals to decide how to act on a case-by-case basis. Furthermore, as the two exercises revealed, the process of considering and resolving ethical dilemmas regarding confidentiality is fluid and complex. The mental health professional needs to consider the various ethical and legal principles in order to arrive at an appropriate and effective resolution.
While it may not always be clear exactly which alternative course of action will be ‘correct’ under the circumstances, the structured decision-making process ensures adequate consideration of the factors that mental health professionals most consider prior to making a decision on how to proceed in the most appropriate manner. Ongoing monitoring is then required, along with modification of the plan or implementation of alternative courses of action as necessary.

Fair Work Ombudsman. (2023). Protections at work.
Overview
All people working in Australia under relevant Commonwealth workplace laws are entitled to general workplace protections. The Fair Work Act 2009 (FW Act) provides protections of certain rights, including:
- workplace rights
- the right to engage in industrial activities
- the right to be free from unlawful discrimination
- the right to be free from undue influence or pressure in negotiating individual arrangements.
These rights are protected from certain unlawful actions, including (but not limited to):
- adverse action
- coercion
- misrepresentations
- undue influence or pressure in relation to:
- individual flexibility arrangements under modern awards and enterprise agreements
- guarantees of annual earnings
- deductions from wages.
What Rights Are Protected Under General Protections?
Workplace Rights
The term ‘workplace right’ is broadly defined under the FW Act, and exists where a person:
- is entitled to a benefit or has a role or responsibility under a workplace law, workplace instrument (such as an award or agreement) or an order made by an industrial body
- is able to initiate or participate in a process or proceedings under a workplace law or workplace instrument
- has the capacity under a workplace law to make a complaint or inquiry:
- to a person or body to seek compliance with that workplace law or workplace instrument
- if the person is an employee, in relation to their employment.
Industrial Activities
All employers, employees and independent contractors are free to become, or not to become, members of an industrial association, such as a trade union or employer association. In addition, all employers, employees and independent contractors are entitled to engage or not engage in what are called ‘industrial activities’.
These activities are defined in the FW Act. They include various forms of lawful participation in an industrial association (such as a trade union) and its activities, including organising or promoting lawful activities for or on its behalf, representing its views, and seeking to be represented. Further, it covers a person being victimised for refusing to be involved in unlawful activity organised or promoted by an industrial association or industrial action.
For more information on industrial action, including what is protected industrial action, please see our Industrial action fact sheet.
Discrimination
Under the FW Act, it is unlawful for an employer to take adverse action against a person who is an employee, former employee or prospective employee because of the person’s race, colour, sex, sexual orientation, age, physical or mental disability, marital status, family or carer’s responsibilities, pregnancy, religion, political opinion, national extraction or social origin.
For more information on unlawful workplace discrimination, please see our Unlawful workplace discrimination fact sheet.
What am I protected from?
Adverse Action
Adverse action is action that is unlawful if it is taken for particular reasons. The FW Act defines a number of actions as adverse actions. Adverse action taken by a person includes doing, threatening, or organising any of the following:
- an employer dismissing an employee, injuring them in their
- employment, altering their position to their detriment, or discriminating between them and other employees
- an employer refusing to employ a prospective employee or discriminating against them in the terms and conditions the employer offers
- a principal terminating a contract with an independent contractor, injuring them or altering their position to their detriment, refusing to use their services or to supply goods and services to them, or discriminating against them in the terms and conditions the principal offers to engage them on
- an employee or independent contractor taking industrial action against their employer or principal
- an industrial association, or an officer or member of an industrial association, organising or taking industrial action against a peson, or taking action that is detrimental to an employee or independent contractor
- an industrial association imposing a penalty of any kind on a member.
The FW Act prohibits a person from taking adverse action against another person because that person:
- has a workplace right
- has or has not used a workplace right
- proposes to, or proposes not to, use a workplace right
- does or does not belong to a trade union
- engages or does not engage in industrial activity (as set out previously).
Adverse action does not include:
- action that is authorised by or under the FW Act or any other Commonwealth law
- an employer standing down an employee who is engaged in protected industrial action
- an employer standing down an employee who is employed under a contract of employment that provides for the employer to stand down the employee in the circumstances.
Coercion
It is unlawful for a person to organise or take action (or threaten to) with the intent to coerce another person or third party to:
- use or not use a workplace right, or use it in a particular way
- take part in industrial activity
- employ or not employ a particular person
- engage or not engage a particular independent contractor
- allocate or not allocate certain duties or responsibilities to a particular employee or independent contractor
- give a particular employee or independent contractor certain duties and responsibilities.
Misrepresentations
A person must not knowingly or recklessly make a false or misleading representation about:
- the workplace rights of another person
- the use, or the effect of the use, of a workplace right by another person
- another person’s obligation to take part in industrial activity
- another person’s obligation to tell anyone whether they, or a third person: is or is not an officer or member of an industrial association
- is or is not taking part in industrial activity.
Undue Influence or Pressure
Undue influence or pressure is when an employer exerts significant or inappropriate pressure on an employee to modify or alter their conditions of employment. It is unlawful for an employer to force or try to force an employee to:
- make or not make an agreement or arrangement under the National Employment Standards (which commenced operation from 1 January 2010)
- make or not make an agreement or arrangement under a term of a modern award or enterprise agreement that is permitted to be included in the award or agreement
- agree to or terminate an individual flexibility arrangement under an enterprise agreement or modern award
- accept a guarantee of annual earnings
- agree or not agree to a deduction from amounts payable to the employee in relation to the performance of work.
- The undue influence or pressure or coercive behaviour can be unlawful even if it does not succeed in making the person take or not take the action.
How Can I Seek Help for A General Protections Contravention?
There are a number of avenues a person can pursue if they believe they have been subject to a general protections contravention.
A person who believes they have been subject to a general protections contravention can request assistance from the Fair Work Ombudsman (FWO) by:
- submitting an online enquiry
- calling us on 13 13 94.
The FWO can investigate allegations of contraventions of the general protections provisions. Where identified, the FWO can initiate legal action for penalties of up to $12,600 for an individual, or $63,000 for a corporation.
The Fair Work Commission (FWC) can also deal with alleged contraventions of the general protections provisions.
There are two main types of applications:
- disputes – if a person has not been dismissed, but alleges that there has been some other contravention of the general protections provisions, they may make an application to the FWC to deal with the dispute
- dismissals – if a person believes they have been dismissed and alleges that their dismissal was in contravention of the general protections provisions, they should make an application to the FWC to deal with the dismissal in the first instance. A general protections dismissal application must be lodged within 21 days of the dismissal taking effect.
Contact us
Fair Work Online: www.fairwork.gov.au
Fair Work Infoline: 13 13 94
Need language help?
Contact the Translating and Interpreting Service (TIS) on 13 14 50
Hearing & speech assistance
Call through the National Relay Service (NRS):
For TTY: 13 36 77. Ask for the Fair Work Infoline 13 13 94
Speak & Listen: 1300 555 727. Ask for the Fair Work Infoline 13 13 94
The Fair Work Ombudsman is committed to providing you with advice that you can rely on. The information contained in this fact sheet is general in nature. If you are unsure about how it applies to your situation you can call our Infoline on 13 13 94 or speak with a union, industry association or a workplace relations professional. Last updated: July 2019 © Copyright Fair Work Ombudsman

