Obesity is defined as a person having a body mass index (BMI) of over 30, or the equivalent for those younger than 18 (Ministry of Health NZ). From a global perspective, the World Health Organisation (WHO) describes the prevalence of obesity as an “epidemic of massive proportions”.
In this topic we will cover:
- an overview of New Zealand statistics
- factors that contribute to obesity
- current approaches for weight loss
- some great tips for motivating your clients to stick with their weight loss journey
- referrals.
New Zealand has the third-highest adult obesity rate in the Organisation for Economic Co-operation and Development (OECD), with rates increasing steadily over the last decade (MoH, 2020). All evidence points to the fact that unless a dramatic change in our eating and exercise habits occurs the levels of obesity in NZ will continue to rise. This is likely to have a crippling effect on the NZ health care system and overall economy.
Barton and Love (2021) produced a report that outlined the economic impact of excess weight in NZ. Here are the key finding of the report:
- Direct costs: The direct cost of health care related to obesity in NZ is approximately $2 billion per year (about 8% of total health care spending).
- Indirect and intangible costs: Include the costs of lost productivity and reduced labour output as a result of obesity and obesity related conditions. These costs are estimated at between $7 billion and $9 billion a year.
Overall, over $9 billion a year can be confidently attributed to excess weight. These costs equate to 2.8% of total GDP or around $1800 per NZ resident per year.
Obesity is also clearly linked to a number of additional health conditions that can impact a person’s quality and longevity of life. The most common conditions associated with obesity are included in the following table. Barton and Love (2021) were able to calculate the attributable cost of obesity to each of these conditions:
| Condition | Prevalence/Impact in NZ | Direct Costs (attributed to obesity) |
|---|---|---|
| Diabetes | 5% of NZ population (245,000) in 2021 | $870 million |
| Cardiovascular Disease | Nearly one in three deaths; 1 in 23 adults affected | $2.1 billion |
| Coronary Artery Disease | Around 177,000 affected in 2019/20 | $125 million |
| Hypertension | One in three adults affected | $274 million |
| Cancers | 3.6% of new cancer cases attributable to obesity | $93 million |
| Arthritis | Increased risk with higher BMI; $500 million attributed yearly | $500 million |
Please note: These figures may be subject to change over time.
Unless a systemic change in approach by New Zealanders is adopted soon, the cost of obesity will soar and place considerable stress on the NZ health system and economy.
The last NZ Health Survey conducted on behalf of the Ministry of Health was completed in 2020/21.
The key findings of this survey in relation to obesity rates of NZ were as follows:
- Around 1 in 3 adults (aged 15 years and over) were classified as obese (34.3%), up from 31.2% in 2019/20. Around 1 in 8 children (aged 2–14 years) were classified as obese (12.7%), up from 9.5% in 2019/20. Prior to this, the rate of obesity among children had been relatively stable
- There was a significant increase from 2019/20 to 2020/21 for women (31.9% to 35.9%), but not for men
- the prevalence of obesity among adults differed by ethnicity, with 71.3% of Pacific, 50.8% of Māori, 31.9% of European/Other and 18.5% of Asian adults obese. The prevalence of obesity among children also differed by ethnicity, with 35.3% of Pacific and 17.8% of Māori obese, followed by 6.6% of Asian and 10.3% of European/Other children
- Adults living in the most socioeconomically deprived areas were 1.6 times as likely to be obese as adults living in the least deprived areas. Children living in the most socioeconomically deprived areas were 2.5 times as likely to be obese as children living in the least deprived areas
(Ministry of Health NZ – Obesity Statistics, 2020/21)
Interestingly, while obesity rates have slowly but steadily increased over recent years, a 2021/2022 update of NZ Health Survey (2020/21) data indicates that obesity rates in NZ remained unchanged between 2021 and 2022. However, due to COVID, a widespread collection of BMI was not possible during this time period, so BMI data for this update were restricted to measures taken by GPs around the country and may not accurately reflect the true state of obesity in the wider population. Regardless, obesity remains an issue for a significant proportion of adults and children in our country.
This means that the future will also see an increased likelihood that you will have clients who exhibit higher BMIs. This topic is designed to help you be better prepared for this eventuality by covering the following areas of interest.
- Factors contributing to the obesity epidemic.
- Factors influencing metabolism.
- The science of fat loss.
- Diet and weight loss – What the research says.
- Exercise and weight loss – What the research says.
- Enhancing motivation and adherence to healthy eating practices.
- Fat loss supplements.
- Referral pathways for tricky clients.
Unpacking the complexity of weight gain
Weight gain arises from an imbalance between calories expended and consumed, a well-established principle in weight loss research. Maintaining a healthy body weight hinges on achieving energy balance, where energy intake matches requirements. While this is known, many struggle to implement it effectively. To combat obesity, it's crucial to not just recognise the calorie imbalance, but to understand why it's occurring. Addressing the underlying causes of excessive calorie consumption is key to making a meaningful impact on obesity outcomes.
Recent research suggests that while energy balance is pivotal, other factors influence it. This insight paints a more nuanced picture, emphasising that while the energy in versus energy out remains central to weight gain, various factors may predispose individuals to an energy imbalance.
Upadhyay et al (2017) performed a review of the literature focusing on the casual factors associated with obesity and concluded that obesity is a complex issue with an abundance of evidence-based literature that presents obesity as a complicated medical condition caused by an inter-play of multiple genetic, environmental, metabolic and behavioural factors. These authors categorise the plethora of casual factors related to obesity as follows.
- Individual behaviours – Relating to food choices, total food intake and activity levels.
- Genetic factors – The presence of genes that predispose people to weight gain.
- Environmental factors – Sedentary jobs, family and cultural practices, income, availability of food etc.
- Metabolic factors – hormones and their effect on weight gain.
- Medications and conditions – That directly or indirectly lead to weight gain.
Please note: These fall outside of the scope of this module.
Let’s look at what the research has to say about each of these potential causes.
Individual behaviours
There is no question that in order to become overweight a person has consumed more calories than their body requires, but is this simply the result of poor nutritional choices on the part of the individual? The term “personal choice” implies human behaviour derives from conscious, volitional decisions and suggests that humans have “free will” to decide between alternative courses of action – independent of biological and environmental forces (Appelhans et al, 2011). However, people cannot be removed from their biological constraints, nor often their environment, so many argue that personal choice is undeniably linked to additional factors beyond an individual’s control.
The way that food is produced can also impact on an individual’s self-control. The human body is designed to provide self-regulation of hunger and satiety (fullness). This mechanism appears to be altered in obese populations. The palatability of our food supply has been greatly enhanced by the food industry through the inclusion of more sugar, fat, salt and flavourings. This means the “reward” stimulus for eating these types of foods (i.e. the experience of “pleasure”) has been significantly heightened which brings about a motivational drive to consume more of the same type of food.
There are also suggestions that the feelings of reward and motivation to eat these foods are grounded in the genetics and neurobiology of individuals, meaning that different people experience the reward of highly palatable foods in different ways (Appelhans et al, 2011).
The neuroprocessing of food reward has been traced to the mesolimbic system, the brains “reward” centre which also mediates the motivation to engage in sex, gambling and substance use (Berridge et al, 2010). Essentially, eating highly palatable food triggers a “reward circuit” that is primarily mediated by dopamine.
Watch the following video that explains this process.
Dopamine is not simply a “pleasure” producing hormone. Yes, it is released in response to tasty food being eaten, but it is also released in expectation of a pleasurable experience and as such can drive the motivation to consume highly palatable foods.
Rather than having a heightened experience of pleasure from eating highly palatable food, there is a hypothesis that obese populations have reduced pleasure signalling which leads to them over-consuming palatable foods in an attempt to create a heightened pleasure effect (Appelhans et al, 2011). The theory is that when the “reward” experience is dampened, individuals have stronger food cravings for sugar, salt and fatty foods as the brain attempts to seek “reward” (this has been shown by higher dopamine release in obese populations at the expectation of food intake). When this stronger drive to consume highly palatable foods is combined with easy access to such foods, individuals become highly vulnerable to becoming overweight and obese.
There is evidence that this “pull” towards highly palatable food that drives over-eating is independent of hunger or fullness signalling. In short, overweight individuals still choose to consume excessive amounts of food, it may just be that the motivation and drive to do so is stronger than in those of healthy body weight ranges.
Control of over-eating is thought to be the job of the pre-frontal cortex of the brain. The prefrontal lobe is located at the front of the brain, specifically in the frontal cortex. It is situated behind the forehead, and it is the largest of the four lobes in the human brain This area of the brain is thought to be critical for self-control, planning and goal-directed behaviours.
Multiple studies have noted that when self-control measures are required, this area of the brain is very active. Essentially, when subjects were placed in positions where self-control was necessary and a decision was required to inhibit impulses for the purpose of self-regulation, those who were able to exhibit self-control had more pre-frontal cortex activation than those who did not exhibit self-control. When the brains of obese populations were studied in this context, they exhibited the same lack of pre-frontal cortex activation as those suffering from ADHD and drug addiction (Appelhans et al, 2011).
In a study by Hare et al (2009), subjects were asked to choose between healthy and unhealthy foods. Those who consistently chose the healthier foods exhibited more pre-frontal cortex activation than those who chose the unhealthy foods. There is also evidence that activation of the pre-frontal cortex is more common in those of healthy body weights after they consume a meal, suggesting that their brains are recognising signals of satiety and exhibiting self-regulation. This post-meal pre-frontal cortex activation is associated with reduced body fat, decreased food cravings and greater success in weight loss. Obese populations did not exhibit the same level of pre-frontal cortex activation following a meal and reported continued food cravings despite having just eaten a meal that should satisfy (Gautier et al, 2012).
So, it would appear that there are a number of neurobiological differences between obese and non-obese populations that make self-control (when it comes to food intake) more difficult for some than others. The question that remains is, are some people pre-disposed to these neurobiological differences, or are they something that occurs when a person becomes obese? This is an area of constant debate. How can some people resist the temptation to consume highly palatable food while others can’t? We could also throw in another question here; why are some people driven to exercise, while others aren’t? Is this also the result of neurobiological differences?
The following short video introduces the potential role of genetics in obesity.
Please note: Take note of the reference to a hormone named Leptin.
Genetic factors associated with obesity
The genetic factors that may pre-dispose people to obesity have been a keen area of interest for obesity researchers for some time now. The notion that genetics may play a role in obesity comes from the simple fact that many of us are living in the same “obesogenic” environments with easy access to and exposure to constant marketing of unhealthy foods, yet some people become obese, and others don’t. This fact raises the question, are some people more susceptible to weight gain than others, when exposed to the same environment?
This question has prompted many studies over the last two decades, many of which have utilised twins and adopted children to see if removing an individual from a particular environment influences their chance of obesity. Since 2007, progress in molecular technologies has allowed for genome scanning and has been successful in identifying more than 100 loci associated with common forms of obesity (Albuquerque et al, 2014). These authors conducted a review of studies related to genetic influences on obesity. Here are the key findings of their report:
- Parental obesity – when both parents are overweight a child has double the risk of developing obesity in childhood. However, to date, scientists have been unable to adequately separate the genetic aspects associated with this increase in obesity from environmental factors within the household.
- Long-term studies of twins and identical twins have shown that these individuals exhibit very high correlations in fat mass and distribution of fat mass over their lifespan (despite often living different lifestyles) suggesting that BMI is highly correlated with heredity.
- Studies using adopted children have found that the BMI of adopted children corresponds more closely with their biological parents than the families they were placed with suggesting a strong genetic influence on fat mass.
- The search for the suspected genotypes that influence obesity has been challenging as studies have not been consistent enough in their findings to make definitive links. It is also very difficult to completely remove environmental factors during studies, so elements of doubt always remain as to the level of effect that is due to genetics alone.
- While a number of genome differences are noted in obese populations, these are likely to be the result of becoming obese, rather than a cause of obesity.
- There is clear evidence of gene mutation that causes extreme obesity, but these are specific medical conditions affecting a very small percentage of obese populations who would exhibit extreme obesity from a young age and do not help explain the general obesity issue.
The authors of this review concluded that although most scientists and clinicians acknowledge that while genes contribute to obesity, there is still relatively little known about the direct effect of genetics on weight gain.
One genome that has received considerable attention in recent years is the Fat Mass and Obesity-Associated Gene (FTO gene). This gene was the first obesity risk gene identified. While its mechanism is not well understood, it appears to exert influence on the hypothalamus which houses the regulation of appetite and satiety. Several variants of the FTO gene are associated with increased BMI and obesity. These variants do not appear in everyone, for example, the A-allele variant (associated with obesity) only affects 42% of Caucasians, 54% of those of African descent and 16% of Asians.
People who carry the risk variants of FTO are more likely to overeat due to a lack of satiety, eat larger portions, prefer calorie-dense foods, eat again sooner after a meal and snack more frequently (Obesity and the FTO Gene, n.d.).
To summarise, while there is a strong belief that genes can play a role in susceptibility to obesity and a number of potential genomes have been identified, at this point less than 3% of inherited susceptibility to obesity is thought to be genetic (Albuquerque et al, 2014). This means that it is still difficult to explain the rapid spread of obesity worldwide based on genetics. Genes rarely have the ability to determine an individual’s anatomy, physiology and behaviour (Albuquerque et al, 2014). However, genes may influence mechanisms of energy homeostasis, causing a variation in body weight within any given environment.
It appears that genes may simply exert some influence on how much the environment impacts an individual, rather than be a direct cause of obesity. This essentially means we are all exposed to the same environmental factors, however, genetic factors may influence our ability to process, self-regulate and when necessary, avoid the temptations of our environment.
Environmental factors associated with obesity
Many authors suggest that the global rise in obesity is driven largely by environmental factors such as high food consumption, high intake and availability of sugary beverages, lower levels of activity (both at work and in our own time) and increased screen time rather than biological factors. There is an abundance of evidence to support this theory. Here are a few key areas of concern that the research has identified:
Family dynamic
Family dynamics are thought to play a large role in the weight status of individuals as family members are likely to have similar diets, screen time, sleep practices and physical activity behaviours. They also commonly exhibit the same perceptions and attitudes to diet and physical activity, resulting in similar outcomes in terms of BMI (Albuquerque et al, 2014). Sedentary lifestyles, reduced physical activity, reduced sleep and increased screen time have all been independently associated with increased weight gain (Yadav and Jawahar (2023). A study by Heinonen et al (2013) examined the effects of sedentary behaviours on obesity and found that for every additional hour of screen time viewed, subjects increased their waistlines by 1.8cm for women and 2cm for men.
Cooking skills and knowledge of nutritional principles are also reflective of the family environment. If a family has limited time, knowledge or willingness to cook their own meals, there becomes a reliance on processed food options. This may also offer one logical solution to the obesity crisis. A study by Arslan et al (2023) found that obese people showed more cognitive restraint, less emotional eating behaviours and improved their BMI as their food preparation and cooking skills improved.
Sleep has also been consistently found to impact on obesity levels. Attitudes to sleep are heavily influenced by the family dynamic. Less than 6 hours or greater than 8 hours of sleep a night is associated with weight gain. Sleep has also been extensively studied in children with findings that even 1 hour of reduced sleep over time correlates with higher levels of obesity (Yadav and Jawahar, 2023). Children from lower socioeconomic households report less sleep than those from higher-income households (most likely due to later bedtimes).
Socioeconomic status and food availability
Obesity prevalence is higher amongst lower socioeconomic groups in developed countries and is also highly correlated with the level of education of parents. Lower socioeconomic groups exhibit both lower levels of physical activity and higher obesity rates. Studies have shown a socioeconomic gradient in relation to childhood obesity with parental education levels one of the strongest predictors of childhood obesity, followed by parental occupation and income. (Albuquerque et al, 2014).
Parental education levels appear to influence the family’s knowledge and beliefs around nutrition, with higher education levels facilitate better understanding and utilisation of available nutrition information (Alder et al, 1994). Children from more educated parents are more likely to eat breakfast and fruit and vegetables; consume fewer snacks and are less likely to eat foods with high-energy content, such as sweetened beverages (Albuquerque et al, 2014).
Children living in more deprived areas tend to eat less fruit and vegetables, but more low-cost energy-dense foods like sugar and sweets, fats, processed meats, salty snacks and soft drinks compared with higher-income households. Lower-income household members also participate in less physical activity (Albuquerque et al, 2014). A meta-analysis by Wu et al (2015) showed that low socioeconomic position is associated with a 41% higher risk of childhood obesity in North America, Europe and Oceania. This is thought to be because families living in poverty have different priorities than those who are better off, with less importance placed on healthy eating and physical activity levels. Surveying has revealed that lower socioeconomic households value energy-dense food (over healthy food) and perceive many healthy food options as beyond their resources or too expensive to buy (Albuquerque et al, 2014).
Over the last decade there has been a growing prevalence of fast-food options in lower socioeconomic areas. Yadav and Jawahar (2023) report that there are up to 30% less supermarkets in low-income neighbourhoods, but statistically more fast-food options in these areas than higher income areas. This, combined with a higher tendency in lower socioeconomic populations to perceive fast food options as more affordable than healthy options means that the average BMI of those in lower socioeconomic areas has increased steadily.
A reliance on processed food
Food intakes that include large amounts of highly processed foods are associated with higher obesity levels. Consumption of highly processed foods has increased markedly over recent years. In the USA and UK, it is reported to make up nearly 60% of these nation’s diets. In Australia, it is more like 42% (Castles, n.d.). While we have limited recent data for NZ, a 2021 University of Otago study looked at the consumption of highly processed foods in NZ children at ages 12, 24 and 60 months and found that highly processed foods made up 45%, 42% and 51% of energy in diets of children at these ages (Castles, n.d.). This shows that our children are not off to a very good start with nutrition. But how does consuming highly processed food lead to obesity?
A study by Hall et al (2019) compared diets high in processed food to those low in processed food and found that even when keeping macronutrient content the same, meals that were ultra-processed resulted in greater food intake and weight gain over a two-week follow-up compared to consumption of non-processed foods. In the study, subjects of healthy body weights were split into two groups. One group were only allowed to consume foods of a processed nature and the other group largely ate unprocessed foods. The food options were calorie and macronutrient-matched, but subjects were instructed to consume as much or as little as they liked of the foods based on hunger and satiety. The processed food group consumed more daily calories over 2 weeks and as such gained an average of almost a kilogram of body weight. Conversely, those in the non-processed group, ate less calories daily and actually lost an average of almost a kilogram of body weight over the 2 weeks.
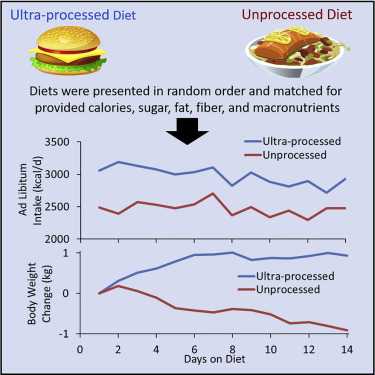
This strongly indicates that by simply eating a diet higher in processed foods, a person will likely eat more total calories and put themselves at a higher risk of weight gain.
Advertising
The marketing techniques employed by the food industries across multiple mediums are also thought to have contributed to the increase in fast food and highly processed foods. Adults appear to be less affected by marketing strategies, but experimental studies with children and adolescents have shown a greater increase in certain fast foods following advertising exposure. Food advertising is often aimed at children with the express intent of making them lifelong consumers (Boyland et al 2016).
A study by Watkins et al (2022) looked at how often NZ children were exposed to unhealthy food advertising every day. The study collected data by small cameras attached to 90 children that recorded what they saw. The cameras collected data every day for 4 consecutive days. The overall findings of the study were that children were exposed to an average of 554 brands in a 10-hour day. Food and beverage products made up 20% of these brands which equated to 68 junk food ads per day. 43% of the brand exposures happened at school, 30% at home and 12% in stores.
Work environment
In recent decades, the nature of work has changed due to globalisation and technological advances making sedentary work and non-standard patterns of work (i.e. shift work) increasingly common. Eng et al (2022) studied the effects of long working hours and sedentary work on NZ employees. The data was collected from over 1.5 million working NZ men and women between 30 and 64 years of age. The authors of this report suggested sedentary occupations (i.e. those that spent over 50% of the working day seated) were more common for females (41%) than males (33%). Approximately, 20% of both men and women also worked in a job that required some form of night shift. Both shift work and long periods spent seated (as in sedentary jobs) have been strongly associated with increased BMI. A clear association exists between work-related energy expenditure and weight gain. There is also a small correlation between long work hours (above 40 hours) and weight gain, with a higher risk associated with 55 hours a week or above (Virtanen et al, 2020).
Food delivery
Access to highly palatable food has never been easier in Western society. Nowadays, people need only reach for their smartphone and food can arrive at their door. Since COVID hit in 2019, NZ has seen a massive increase in the use of food delivery apps. Uber Eats alone has added more the $162 million to the NZ economy each year (Wynn, 2022). Kiwis appear to be willing to pay up to 25% more than if they had gone out to get the food themselves and around 25% of young people report being regular users of these food delivery apps. School drop-offs in Auckland at lunchtime became so frequent that school principals were forced to ban students from ordering food to school (Wynn, 2022).
The use of food delivery apps in the USA is an even bigger business showing growth of 23% in the last 4 years and returning $26.8 billion to the USA economy. While a wide range of foods including healthy options are freely available for consumers, the most frequently used platforms report that the most commonly ordered foods through the apps are cheeseburgers and fries, pizza, nachos, cheesecake, pork ribs and other calorie-dense options (Stephens et al, 2020),
Research into the negative health impacts that the use of these apps is having on people is limited at this point in time, however, the latest World Health Organisation European Obesity report has flagged food delivery apps as a likely contributor to the rising obesity problem as they encourage even more sedentary behaviours and play a significant role in increasing consumption of high fat and high sugar foods and drinks (Roxby, 2022).
Metabolic factors contributing to obesity
It’s not my fault, I have a slow metabolism
First, let’s clear up a common misconception regarding metabolism and becoming overweight. Overweight populations do not have a slow metabolism. In fact, the basal metabolic rate of overweight or obese people is usually higher (to accommodate for the extra fat tissue they must maintain, and the increased difficulty associated with performing normal bodily functions (Marcus, 2013). While there is a genetic variance in metabolic rate between individuals, the reality is, that weight gain is the result of consuming calorie amounts that are over and above the requirements of the body. Like the genetic influences discussed earlier, individual variances in metabolic rate may influence the likelihood of gaining weight, however, only if excessive calories are consumed on a chronic basis.
Hormones linked to obesity
Let’s turn our focus on the metabolic effects that obesity causes in the body (i.e., those that occur once a person becomes obese). The metabolic effects of obesity are often referred to collectively as “metabolic syndrome”. Metabolic syndrome refers mainly to alterations in the way that hormones are produced and recognised by the body. One of the main effects of metabolic syndrome is insulin resistance, which can culminate in impaired glucose tolerance, high cholesterol, hypertension, diabetes and premature heart disease (Singla et al, 2010). Insulin resistance is a term used to describe impaired glucose sensitivity. This occurs when the cells in your muscles, fat and liver don’t respond to insulin as they should. This means that insulin’s role in regulating blood sugar by facilitating the entry of glucose into cells is impaired, leading to high circulating blood glucose levels and a high risk of developing diabetes.
Obesity is characterised by an excess of adipose tissue or body fat. Adipose tissue is a major endocrine organ in the body that produces various hormones that regulate metabolism. An increase in fat cells leads to imbalances in the production of these hormones, which can have various metabolic effects (Singla et al, 2010). Of these hormones produced by adipose tissue, those that play an important role in body weight regulation are listed in the following table:
| Hormone | Function | Obesity Association |
|---|---|---|
| Leptin | Thought to play a major role in regulating appetite and desire to move. | Levels of leptin are elevated in obese populations. |
| Visfatin | Thought to act like insulin as a means of keeping blood glucose levels stable (may increase fat storage). | Levels of visfatin are increased in obese populations. |
| Apelin | A substance that is elevated in obese populations and appears to alter glucose and lipid use for energy. May be an insulin inhibitor that plays a role in insulin resistance. | Levels of apelin are elevated in obese populations. |
| Resistin | Provides resistance to insulin. It is a hormone released due to inflammation (in this case of fat cells). | Levels of resistin are increased in obese populations. |
| Adiponectin | This hormone aids insulin in glucose uptake and increases the use of fat as a fuel. | Levels of adiponectin are decreased in obese |
While the exact roles and effects of many of these hormones are still being investigated, the role of leptin in obesity has been extensively researched. Let’s move on to learning about the role of leptin in obesity and discuss the effects of obesity on the production and effectiveness of insulin.
Leptin
Leptin is a protein-derived hormone secreted from fat cells. Leptin is thought to have several roles including growth control, metabolic control, immune regulation, insulin sensitivity regulation, and reproduction, however, its most important influence is in body weight regulation.
Leptin is the chief regulator of the “brain-gut axis”, which provides a satiety (fullness) signal to the hypothalamus. When leptin is recognised by the hypothalamic leptin receptors, they suppress food intake and promote energy expenditure. Put simply, leptin is produced by the stored fat cells. The more fat cells you store, the more leptin your fat cells produce. This leptin travels in your bloodstream to the brain, where leptin receptors respond by reducing appetite and increasing the desire to engage in movement. In a well-functioning system, this should lead to the maintenance of a stable body weight. The image below helps explain how leptin works.
When food intake increases (or energy expenditure decreases) and a positive energy balance is present, we tend to store increased amounts of body fat. This fat tissue produces the hormone leptin. Leptin receptors in the hypothalamus recognise leptin and the brain establishes that we have enough fat stores, so reduces appetite and stimulates a desire to move more.
![[ADD IMAGE'S ALT TEXT]](/sites/default/files/Leptin.png)
Conversely, a body with very little body fat will produce very little leptin. The brain will recognise this lack of leptin and as a means of survival will increase appetite and decrease calorie expenditure in order to ensure the body has sufficient stores of fat for survival. Click through the following images to show how this mechanism is supposed to work.
The first column shows a body with low body fat stores (empty adipose cells). This reduced leptin signalling leads to an increase in appetite leading us to eat.
The second column shows a body with full adipose cells, leading to increased leptin secretion and signalling. This results in a reduction in appetite leading to reduced calorie consumption.
It appears that this regulatory signalling system becomes faulty in obese populations. This has become known a “leptin resistance”. Leptin resistance is thought to be caused by either a defect in intra-cellular signalling associated with the leptin receptors or decreases in leptin transport from the blood to the brain (Gruzdeva et al, 2019).
It was initially thought that this faulty effect could be the result of a gene mutation, but this has been found to be extremely rare in humans and typically results in the development of morbid obesity directly after birth. Instead, the primary cause of leptin resistance is thought to be that excessive levels of leptin in the blood (due to large stores of body fat) reduce the amount of leptin that can cross the blood-brain barrier.
There is an additional theory that inflammation also plays a role in blocking the transport of leptin across the blood-brain barrier. As adipose cells enlarge, an inflammatory protein called C-Reactive Protein (CRP) is released. It is thought that CRP binds to leptin and prevents it from crossing the blood-brain barrier (Singla et al, 2010).
Essentially, this means that as more body fat is stored and an increase in leptin production occurs, less leptin appears to reach the brain where leptin receptors are located. This leads to the brain thinking that little leptin is in the blood and the subsequent increase in appetite and decrease in motivation to expend calories leads to a rapid increase in body fat stores. A brain receiving no leptin signals, believes that the body has little to no fuel reserves (body fat), so resorts to protective measures including a sharp increase in appetite and a slowing of the metabolism (to conserve energy). It is thought that this double effect leads to rapid weight gain.
The following is a great video that explains the effects of leptin resistance, the mechanism of insulin resistance, and how the food industry and environment we live in have led to the global obesity crisis.
To summarise, becoming obese triggers a number of alterations to hormone release and effectiveness which leads to disruption of the body’s normal weight management mechanisms. Many of these changes are driven by inflammation associated with the rapid increase in the size of adipose cells. These changes in hormone secretion lead to increased appetite, decreased motivation to move (and burn calories), and altered substrate use resulting in a propensity to store body fat rather than use it for energy. These things combined result in a cycle of fat storage that results in continuing weight gain. Add to this a food industry that promotes easily accessible, highly palatable foods and obesity becomes rife.
The great obesity debate
While the basic cause of obesity is undoubtedly an imbalance of calorie expenditure to calorie consumption, as we have already discussed, the factors that contribute to wide-spread obesity in a population are multidimensional. Jenkin et al (2011) believe the true explanations for the obesity epidemic in NZ are often convoluted by the input of various stakeholders which has led to a debate over the key casual factors. These debates are often played out in the media which cause confusion in the general public as a multitude of core reasons for obesity are discussed. They may also be the reason why progress in halting the increase in obesity is slow.
The competing interests of the food industry and their marketing teams, the public health sector, the exercise industry and political groups result in the blame for obesity being constantly shifted from one cause to another.
Jenkin et al (2011) performed an inquiry into the way the causes of obesity in NZ are framed by two of the main stakeholder groups involved in this debate: “Industry” - which included Food Manufacturers and Marketing Agencies; and the “Public Health Sector” - which included non-government organisations, professional associations and independent advisors. The inquiry collected the opinions of 17 major food companies and marketing agencies along with 14 public health organisatons. Here are the key findings of the report:
- Both groups described the key contributing factors to obesity as “complex”
- Industry referred to obesity as an “issue” or “concern” and labelled it a “health-threat/problem”. Public Health referred to obesity as an “epidemic” and recognised the wide-reaching costs associated with obesity across our economy.
- Both groups accepted that genetics were not responsible for increases in obesity.
- The industry group maintains that the main cause of obesity is freely chosen individual lifestyles characterised by over-consumption of food and lack of physical activity. They denied that advertising and the cost and availability of high-calorie, nutrient-poor food was the main issue and argued instead that poor attitudes to food, lack of motivation to change, lack of knowledge, poor willpower and denial of weight issues were the key factors.
- The Public Health disagreed strongly that increases in obesity were down to individual characteristics instead blaming an “obesogenic environment” where nutrient-poor energy-dense food was cheap, readily accessible and “shamelessly promoted”. They identified the key contributors as sugary drinks, highly processed foods and foods high in fat, sugar or both. Of course, the industry contests these suggestions and has drawn on evidence to refute these claims.
As you can see, the different agendas of these key players leads to an ultimately pointless debate that takes energy and focus away from a solution to the issue of obesity in NZ. This constant debate slows the potential for solutions and strategies to combat the issue. The industry group maintains that the “self-regulation” approach to food advertising is working and has described in detail its voluntary efforts that have already been employed to address obesity (for example, product ingredient changes, food labelling and sponsorship of education, community sport and physical activity events). The public health group disagrees labelling the approach as one where “the wolves are guarding the henhouse" and instead would like to see more regulations, restrictions or bans (across all advertising mediums) on the marketing of unhealthy foods.
The food industry argues that the main issue is a lack of physical activity rather than overeating, the exercise industry believes a combination of excess food and lack of activity causes, while public health groups believe obesity is due to ubiquitous marketing and availability of low-cost, energy-dense/nutrient food. Those with political affiliations argue that social inequity is the root cause.
In truth, all of these factors contribute to the obesity crisis we find ourselves faced with in this country, but a lack of cohesion between stakeholders and the constant debate leads many New Zealanders to place the blame for their increasing waistlines on factors outside of their control.
To summarise, the factors contributing to widespread weight gain are absolutely multi-faceted, but the over-riding fact remains. The reason people are becoming overweight is because they consume too many calories. This is most likely due to the result of personal choice and living in an obesogenic environment. The extent to which individuals are affected is also influenced by genetic factors and hormonal alterations. Regardless, we have an obesity issue in this country, and it appears that it will get worse before it gets better. Personal trainers will continue to play a key role in disseminating quality advice to overweight clients and in enabling clients to achieve their weight loss goals through a structured programme of exercise and healthy eating practices.
When you lose fat, where does it go?
While the answer is somewhat complex and involves high-level math and science, this question is answered beautifully (and simply) in this great video.
Note: While this video is 20 minutes long, it is definitely worth it!
Try it out
Let’s turn our focus to what research suggests regarding the best way to assist our weight-loss clients in achieving a healthy body weight (and maintaining it).
Let’s discuss some commonly used and researched approaches for weight loss.
If the root cause of obesity is consuming an excess of calories over time, then the solution for obesity (and a return to a healthy body weight) is pretty obvious. Create a calorie deficit.
There are two primary ways in which you can create a calorie deficit:
- Consume less calories
- Expend more calories
Research has found a few proven methods in relation to helping people create a calorie deficit and achieve meaningful and sustainable weight loss. There are a number of weight loss strategies that can be employed to lose weight that have been backed up by research. The most common of these include:
- Nutrition advice.
- Calorie restriction diets.
- Exercise approaches alone.
- Calorie restriction diets and exercise.
- Very low-calorie approaches.
- Meal replacement approaches.
- Prescribed obesity medications (outside the scope of this module).
- Obesity surgeries (outside the scope of this module).
There is plenty of evidence to suggest that a number of these approaches can lead to meaningful weight loss. Franz et al (2007) performed the largest systemic review and meta-analysis of weight-loss clinical trials that had a minimum 1-year follow-up (to date). The review included 80 clinical intervention studies and articles including over 26,000 participants.
- 51 of studies included a “diet alone” weight loss strategy
- 17 included diet and exercise strategies
- 7 studies used meal replacement interventions
- 11 studies used very low-calorie diets
- 20 studies included a weight loss medication intervention (Orlisatat and Sibutramine)
- 28 studies included a “nutrition advice only” intervention
- 2 studies included exercise-only interventions.
Here are the key findings of the review:
- All weight loss interventions that included a reduced calorie diet and/or weight loss medication resulted in weight loss during the first 6 months.
- After 6 months, weight loss plateaus were evident but none of the groups experienced a complete regression to baseline weights at the one-year mark.
- Those in the “nutritional advice only” or “exercise only” interventions experienced minimal weight loss across all time points.
- Those who were in diet-only groups experienced a mean weight loss of 4.9% at 6 months, 4.4% at 12 months, 4.4% at 24 months and 3% at 48 months.
- When exercise interventions were added to diet interventions mean weight loss was increased to 7.9kg at 6 months, with 4kg of weight loss maintained at 48-months.
- Stricter calorie restriction through the use of meal replacement shakes resulted in 8.6kg weight loss at 6 months and 6.7kg loss maintained at 12 months. Very low-calorie diet subjects lost 17,9kg at 6 months followed by rapid regain (10.9kg at 12-months, 5.5kg at 36 months).
- Exercise alone groups experienced only 2.4kg of weight loss at 6 months reducing to 1kg at 12 months.
The results are shown in visual form below:
In summary, all of the subjects lost weight in these clinical trials, showing that initial weight loss is possible using a variety of approaches. What is also clear from the data is that neither nutrition advice nor exercise approaches alone are effective means of achieving weight loss. The addition of exercise to reduced calorie diets results in better initial weight loss outcomes but it appears obesity medications can achieve much the same results. Very restrictive diets lead to the most significant initial weight loss.
It should also be noted that Interventions and follow-up in these studies were provided by registered dietitians in 51 studies, by behavioural specialists in 17 studies, and in three studies by nurses or physicians. Support was also available to the subjects when needed in the form of behavioural therapists, exercise physiologists, and physicians throughout the trials. This level of support is often absent for individuals attempting weight loss on their own.
What is also apparent from the data is that there is a general trend towards regaining lost weight, the longer the trials continued. Also of note is that 31% of the participants of these studies dropped out with the most common reason given being that the intervention was too hard to adhere to. This means that the majority of data used in this review was from those who completed the trials. If the data of the 31% of the subjects who failed to complete the trials was added, the authors suggest that the longer-term follow-up weight loss data would likely show even less of a weight loss outcome at 12, 24 and 48 months.
Therefore, while a range of weight loss approaches work in the short term, it appears that a return towards baseline weight appears to occur in most instances.
Diet only approaches
The term “diet” (in reference to weight loss) is a practice by which calories are often severely restricted to achieve a substantial daily calorie deficit. Diets (by design) are goal-orientated, and as such they end at some point. This means that while all calorie restriction diets work in the short term, research suggests almost none work long-term, as when people end reduced calorie approaches the weight piles back on.
Here is what the research has to say about calorie-restrictive dieting as a long-term approach to weight loss:
- In 2002, 231 million Europeans attempted a diet through an organised weight loss management group. Almost all reported initial weight loss but only 1% kept the weight off after an additional 12 months (Kravitz, 2009).
- Dieting leads to unfavourable eating habits in the long term. A history of dieting is often associated with rigid control of diet, followed by disinhibited eating patterns (Gallant et al, 2012). This means people swing between severe calorie restriction and uncontrolled binging. These authors concluded that dieting damaged the chances of maintaining a healthy weight. Alonso et al (2015) also suggest that dieting leads to neurological mechanisms that cause dieters to become overly responsive to food, increasing temptations. This results in food having increased reward value making it harder to resist.
- A meta-analysis of 29 long-term weight loss studies reported that more than half of the lost weight was regained within two years, and by five years more than 80% of the lost weight was regained (Loveman et al, 2011). The National Eating Disorders Association of America (2005) suggests that weight regain is even higher with 95% of all dieters regaining their lost weight and more within 1-5 years.
- Tomiyama et al (2013) reviewed 22 research articles examining the long-term effects of dieting completed between 1993 and 2013. To be included in the review, studies needed to have a minimum follow-up period of 2 years. The average amount of weight loss maintained by participants from baseline to 2-year follow-up was only 0.94kg. Dieters showed non-significant improvements in blood pressure, blood glucose and blood lipid levels compared to control groups but none of these correlated with weight changes.
This is just a selection of findings from a vast number of studies and reviews that have looked at dieting as a form of weight loss. The same themes come through time and time again. Rigid dieting results in meaningful initial weight loss, but very few people are able to maintain this approach for long periods of time, resulting in the regain of at least some, if not all of the weight lost within the next few years. There are a number of suggestions for why this happens:
- A body will not simply put up with ongoing calorie restriction forever. It will more likely adapt. When you begin restricting the number of calories a body usually receives, the body adapts to run on fewer calories by slowing down metabolism and attempting to store the calories it receives. This appears to be a built-in biological mechanism that exists to allow us to survive in times of food scarcity (Mattson et al, 2019). This causes people to regain most of the weight they lost.
- Benton and Young (2017) suggest that hormonal mechanisms that stimulate appetite remain raised even a year after dieting has been maintained. Given that most diet approaches end well before this time period, the same drivers that led to over-consumption in the first place will still be present at the end of the diet period.
- Jean and Malkova (2016) reviewed the available research around appetite signals in obesity and concluded that diet-induced weight loss results in long-term changes in appetite gut hormones that appear to favour increased appetite and weight regain.
- The National Weight Control Registry at the University of Colorado has tracked over 10,000 people over at least 5 years on their weight loss journey. Those who supplied data to the registry reported that weight maintenance became easier after 2 years of adherence to a calorie-deficit diet and that the chances of long-term weight loss management increased after 2-5 years on a calorie-deficit diet. This time period appears to be well outside of the time an average dieter is prepared to subsist on a calorie deficit for.
Add to these findings the fact that those obese individuals who start dieting are still bound by potential genetic, hormonal and environmental and social factors that have contributed to their weight gain and it is easy to see why weight loss is a very difficult undertaking to be successful in long term.
This was evidenced by the systemic review and meta-analysis by Franz et al (2007) discussed earlier where 31% of the subjects withdrew from the various studies by the end of the 1-year follow-up citing that the approaches were too difficult to adhere to. Franz et al (2007) also report that community-run weight management programs tend to experience higher dropout rates than clinical trials (like the one’s involved in their review).
It appears that even commercial weight loss approaches fail to produce meaningful weight loss outcomes. McEvedy et al (2017) reviewed 25 trials and reviews of meal replacement, calorie-counting and pre-packaged meal programmes run by commercial organisations (e.g. Jenny Craig) and concluded that these programmes frequently fail to produce clinically meaningful weight loss and have high dropout rates suggesting many consumers find the dietary changes unsustainable.
However, there is no getting away from the fact that in order to lose weight, individuals must achieve a chronic calorie deficit. There are a number of ways to achieve this (e.g. diet, exercise, or both). According to Johnston et al (2014) who conducted a meta-analysis on a number of diet approaches for weight loss, calorie restriction is the primary driver of weight loss, followed by macro-nutrient composition. However, as previously discussed, diet interventions that create a substantial energy deficit are likely to be countered by physiological or biological adaptations that resist weight loss. The first and most obvious question in relation to this is, how much of a calorie deficit do we need to create?
Most low-calorie diets suggest consumption of 1000-1500 calories per day, with many studies and weight loss societies recommending a 500-750 calorie deficit in their guidelines for weight loss (Kim, 2021). Very low-calorie diets of less than 800 calories per day have also been used in trials but are not recommended for routine weight management despite showing evidence of effectiveness. The reality is, there is no recommended calorie deficit for enhancing the chances of long-term weight loss maintenance as there are many and varied factors associated with long-term outcomes. The ideal calorie deficit for an individual is one that they can adhere to for the foreseeable future and that satisfies their basic health requirements. That said, the majority of the literature points towards a deficit of at least 500 calories per day with suggestions that this level of deficit should be possible without experiencing extreme hunger or fatigue issues (Van De Walle, 2019).
Macronutrient manipulation
Research to date is pretty clear, any sustained calorie deficit will result in weight loss regardless of the macronutrient composition of the food you eat. Wait what? That would mean a person could lose weight on a diet of beer and pies (as long as a calorie deficit is maintained). Well....yes.
Christchurch-based Newshub reporter Julian Lee did just that when he set out to explore claims that it didn’t matter what you ate when trying to lose weight as long as you consistently achieve a calorie deficit. Lee had his calorie requirements estimated by a qualified nutritionist at 2,500 calories a day. On his beer and pie diet, he consumed 1600 calories in the form of 3-4 pies a day (depending on the calorie content of each pie). Once a week, he swapped one pie for 3 beers. After 4 weeks, Lee found that he had lost 8kg on the diet. Of course, there were negative effects of eating just pies including cognitive impairment. At the end of the experiment, he described himself as “delusional right now” and said he was “losing the plot!”.
The results of this non-scientific experiment have also been backed up by scientific literature. When calories are controlled, the macronutrient composition of food eaten does not impact the amount of weight lost with similar weight loss observed in those who consumed a variety of macronutrient compositions. Boaz (2015) conducted a meta-analysis comparing low-fat, high protein and low-carbohydrate diets in calorie-controlled trials and concluded that manipulation of macronutrient composition does not appear to be associated with significantly different weight loss outcomes. In other words, provided a calorie deficit is maintained, weight loss outcomes will be similar regardless of the macronutrient composition of the food eaten.
While the pie and beer approach is definitely not recommended, it does highlight the simplicity of the task for a weight loss client. To lose weight and keep it off, you must create a sustainable calorie deficit that can fit into your daily lifestyle and provide the nutrients you need for good health. There are a multitude of ways to do this, but the key is to find an approach you can adhere to. This is where macronutrient manipulation may be effective, and this has led to a number of popularised diets promoting low carbohydrate and high protein intakes. The theory behind low carbohydrate diets hinges on the fact that some carbohydrates elevate insulin secretion, thereby directing fat towards storage in adipose (fat) tissue.
While the type of macronutrient eaten may not impact weight loss outcomes in calorie-monitored situations, this may not be the case in situations where individuals are not calorie-restricted. There is clear scientific evidence that certain macronutrient intakes are easier to adhere to than others. This is critical to long-term weight loss outcomes, as while a number of approaches can lead to significant initial weight loss, keeping the weight off appears much more difficult.
Research has provided strong indications of the best way to manipulate macronutrients to enhance adherence to a calorie deficit diet long term. Larsen et al (2010) studied the effects of different dietary approaches on subjects who had already lost weight following calorie-restricted diets. Of the 938 subjects involved in the trial, all had lost at least 8% of their total body mass following a low-calorie diet. Larsen et al (2010) randomly placed each subject into one of five diet groups to assess how each diet approach prevented weight regain over the next 26-weeks. The key difference between this study and other studies was that the subjects were instructed to eat ad libitum (as much as they felt like) but were only able to eat foods from a list corresponding to the macronutrient diet group they had been placed in. The five diet groups were:
- A low-protein (13%) and low-GI carbohydrate diet.
- A low-protein (13%) and high-GI carbohydrate diet.
- A high protein (25%) and low-GI carbohydrate diet.
- A high protein (25%) and high-GI carbohydrate diet.
- A control diet – that followed the general dietary guidelines of the subject’s home country.
The results of the experiment are shown in the following image:
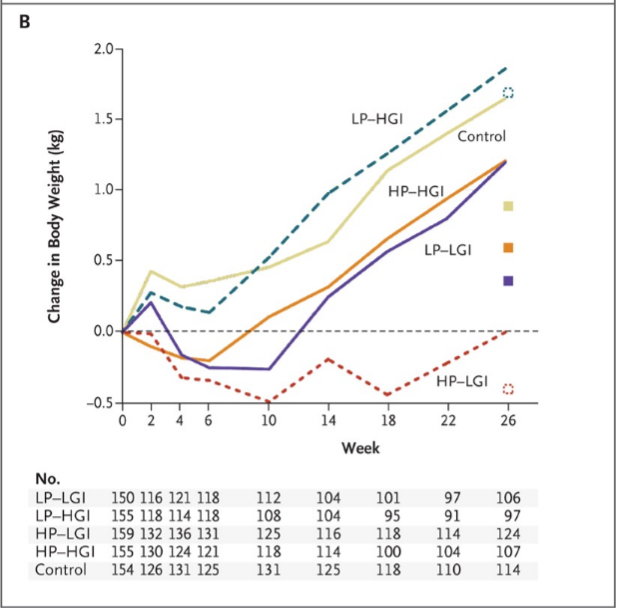
548 (71%) of the subjects completed the 26-week intervention they were assigned to. More subjects dropped out of the High GI carbohydrates groups and low protein groups than the high protein groups. The results show that the rate of completion and successful maintenance of weight loss were better in participants who were assigned to the high protein diets and to the low GI diets than the low protein/high GI diets. In addition, those in the high protein and low GI carbohydrate group continued to lose weight after the intervention began. The higher protein diets were achieved by reducing total carbohydrate load and the inclusion of only low GI carbohydrates in this group further reduced the glycemic load (total carbs x GI number). These results support a number of findings from previous research that indicate that reducing glycemic load is important for controlling body weight in obese patients. The high protein, low GI group was the only group that hadn’t gained weight by the end of the trial.
As an additional experiment, Larsen et al (2010) had some of the subjects receive their food free for the 26 weeks, while others received dietary advice only (and had to pay for their food). Those following high protein diets that were given their food for free gained 2.7kg less body weight than the low protein groups that were given food, whereas the difference was only 0.54kg between the groups that had to buy their food.
The authors concluded that a moderately high protein intake along with lower GI carbohydrate sources both improved adherence to the diet and maintenance of weight loss, therefore appearing to be the optimal macronutrient balance for the prevention of weight gain. This obviously has relevance to populations wishing to prevent the onset of weight gain in any context also. Another study by Larsen et al (2010) compared a high protein (HP) diet with a high carbohydrate (HC) diet. The two diets were calorie-matched, with similar amounts of sugar and fat in each, and calculated to provide a moderate calorie deficit. Details relating to the diets compared are shown in the following table:
| Nutrient | HP diet | HC Diet |
|---|---|---|
| Energy (kJ) | 5615 | 5602 |
| Protein (g) | 107 (32% of E) | 67 (20% of E) |
| Carbohydrate (g) | 138 (41% of E) | 191 (58% of E) |
| Sugars (g) | 73 | 83 |
| GI/GL | 46/61 | 52/93 |
| Dietary fibre (g) | 23 | 24 |
| Total fat (g) | 38 (25% of E) | 32 (21% of E) |
| Saturated fat (g) | 11 | 10 |
| Cholesterol (mg) | 298 | 87 |
The results of the study show that the participants lost weight on both diets, but that the HP diet was more successful for both short and longer-term weight loss. As the graph shows those on the HP diet (in green) not only lost more weight initially but had greater weight loss when the diet was maintained for a year.
The effectiveness of higher protein diets
A review of scientific evidence of diets for weight loss completed by Freire (2020) agrees that diets that contain at least 20% of total energy as protein appear to offer advantages in terms of weight loss and body composition in the short term. Higher protein diets assist weight loss in a number of ways but most probably because:
- Protein is the most satiating macronutrient (remains in the stomach for longer than other macros). This makes it easier to avoid over-eating. A critical review by Halton and Hu (2004) reported that there was convincing evidence that a higher protein intake increased thermogenesis (calorie burn producing heat) and satiety compared to lower protein intakes and that high protein meals led to reduced subsequent food intake. This is supported by Kohanmoo et al (2020) who performed a meta-analysis and systemic review on the effect of short- and long-term protein consumption on appetite and appetite-regulating hormones. These authors review 68 studies and articles on the subject and concluded that acute ingestion of protein not only suppresses appetite by staying in the stomach longer, but also decreases production of the hunger hormone ghrelin.
This effect can be quite powerful. Weigle et al (2004) found when they increased the protein content of subjects’ diets from 15% of total calories to 30%, the subjects consumed an average of 441 less calories each day of the trial without intentionally restricting anything.
- Protein uses more calories to digest than the other macros giving it a higher thermic effect (TEF). About 25% of protein calories ingested are used to break down protein for absorption (when eaten in food form). This compares with carbohydrates (6%) and fat (around 2%).
- A high protein intake increases the chances of maintaining good levels of Iron intake (also benefits levels of other micro-nutrients such as B12, Folic acid, calcium).
Important
While the term “high protein” diet is used a lot in weight loss circles, in reality, a high protein diet does not require eating lots of meat, drinking protein shakes, and generally seeking protein sources out every time you eat. The research that has been completed in this area typically uses “high protein” diets that contain around 25% of total energy as protein. In Western populations (and especially in those that consume animal products) achieving this much protein in the diet requires no additional focus on protein. The WHO suggests most people who eat a balanced diet achieve daily protein requirements with ease.
Active populations require more protein than sedentary individuals. However, there is no compelling evidence that consuming over 2g of protein per kilogram of body weight offers additional benefits to athletes. A 70kg athlete involved in a mix of resistance and cardio training would require between 1.3-1.5g/kg of protein a day. This translates to 91-105g of protein a day. Here is an example from the Australian Institute of Sport (2009) that shows just how easily protein these protein levels can be attained.
| Quantity of food required to provide needs for a 70 kg athlete | Amount of protein (g) | ||
| Breakfast | 2 cups cereal 300 ml milk 2 slices toast 2 tablespoons jam 1 cup juice |
6 12 8 0 2 |
|
| Lunch | 2 bread rolls each with 50 g chicken + salad 1 banana 1 fruit bun 250 ml flavoured low-fat milk |
41 2 6 13 |
|
| Dinner | Stir-fry with 2 cups pasta + 100 g meat + 1 cup vegetables 1 cup jelly + 1 cup custard |
50 13 |
|
| Snacks | 750 ml sports drink 1 carton yoghurt 1 piece fruit 1 cereal bar |
0 10 1 2 |
|
| Analysis | 166 g (2.3 g/kg) |
Table source: Australian Institute of Sport "Position on Protein" (2009)
As you can see, the athlete has not focused on consuming large portions of meat or relied on protein shakes to easily attain their protein needs. Protein is found in a variety of foods, so before dramatically increasing the protein intake of a client, consider the amount of protein they are actually consuming. A simple diet log analysis will help you confirm this.
High-fat diets
There has been a lot of recent interest in the ketogenic diet and weight loss. While the ketogenic diet appears to have some advantage over high carbohydrate diets in terms of reducing appetite and hunger and has shown significant weight reductions, many studies of the diet have been largely uncontrolled. Additionally, a number of negative effects such as constipation, halitosis, headaches, muscle cramps and muscle weakness were commonly observed. Studies into more worrying effects on lipid profiles, liver function and cardiovascular risk factors also remain inconclusive (Freire, 2020).
So, for now, higher protein diets appear to carry less risk, although this author warns that while high protein, low carbohydrate diets on balance are useful to elicit initial weight loss effects, they should be used in the short term rather than a diet for life. This is due to some concern that remains over the effects this diet approach can have on metabolism and gut health, and because animal-derived protein and fat have been associated with higher mortality (death) than plant-based protein and fat (Freire, 2020). This author suggests that on current evidence, a more balanced macronutrient split (while maintaining a calorie deficit) could achieve similar weight loss results without the associated health risks. In particular, she references the fact that data shows an increased mortality rate with long-term intake of both low and high carbohydrate intake, but that an intake of around 50-50% carries minimal risk.
Weight loss on a plant-based diet
Adoption of plant-based diets is growing because evidence has shown some health benefits when compared with omnivorous diets. Plant-based diets have been shown to protect against chronic diseases, such as cardiovascular disease, hypertension, type 2 diabetes and some cancers, however, further research is required to clarify whether these benefits are related to a reduction in animal products or an increase in fruits, vegetables and fibre (Freire, 2020).
A plant-based diet appears to aid the maintenance of a healthy body weight with individuals on plant-based diets usually presenting with lower BMI than non-vegetarians. But are plant-based diets also associated with meaningful and sustainable weight loss?
Two meta-analyses on this subject would suggest they are. Combined evidence from reviews by Banard et al (2014) and Huang et al (2016) reported a clear association between adopting a plant-based diet and weight loss that was attributed to lower energy intakes on these diets. However, it should be noted that not all studies in the meta-analysis reported meaningful weight loss outcomes and many failed to achieve the same level of weight loss as the higher protein approaches discussed above. The authors of these reports also mentioned the importance of those adopting plant-based diets to seek appropriate nutritional guidance to avoid potential nutrient deficiencies.
Intermittent fasting
Intermittent fasting has recently received a lot of attention as a nutritional strategy for weight loss. The appeal of being able to “eat normally” during short periods of the day, resonates with many who struggle to give up the foods they enjoy. Several variations of intermittent fasting have become popular. The most commonly followed are the 16:8 (no food between 6pm and 10am) and alternate-day approaches. Weight loss experiments using an intermittent fasting intervention have resulted in average weight loss of between 4-10% over dieting periods of 4-24 weeks, although not all studies have reported meaningful weight loss (particularly those including alternate day fasting). Freire (2020) suggests there is growing evidence to demonstrate the metabolic health benefits of intermittent fasting (especially in animal studies), but that fasting approaches do not appear to offer superior weight loss outcomes than other continuous calorie restriction diets.
A systemic review of the literature regarding intermittent fasting and weight loss was completed by Welton et al (2020) who agreed that while intermittent fasting shows promise as a weight loss tool, more research is required to understand the long-term effects of this approach.
Following her systematic review on dietary approaches to weight loss literature, Freire (2020) concluded that people will continue to follow popular trends in weight loss, despite most evidence coming from personal accounts, blogs and weight loss articles, rather than from rigorously controlled research. At this point in time, clinical research evidence remains inconclusive making it impossible to recommend an optimal dietary approach for weight loss. In the short term, different diets promote different degrees of success with all that create a meaningful and ongoing calorie deficit resulting in weight loss. However, the long-term results of these dietary approaches elicit small differences which do not instil enough confidence to recommend one approach over another.
Freire (2020) believes there are a number of important questions still to be answered by research. Why do some individuals experience successful weight loss, whereas others are more resistant to weight loss (using the same approach)? How do different diets change things like hormonal secretion, gut microbiome composition, and gene expression, and how do they effect energy, function and appetite (in the long term)?
Knowing which weight loss approach works best
While the information on the various weight loss approaches doesn’t give a clear indication of what approach is best for weight loss, it does suggest that a variety of dietary approaches do result in meaningful weight loss. This is actually a good thing! It means that approaches can be tailored to individual preferences as long as three key concepts are understood.
- The dietary approach must create a calorie deficit to result in weight loss.
- The dietary approach must be something that a client can adhere to long-term.
- The dietary approach should contain high-quality foods to ensure basic health requirements are met (i.e. micronutrients).
In order to satisfy the first point, a client must seek the advice of a nutrition specialist to determine what their daily requirement for calories is. Once this is established a meaningful calorie deficit (typically around 500 calories a day) can be calculated.
Next, the client must be educated enough to make decisions about food choice. This will of course include understanding the calorie density of foods but should also include information to ensure they meet their daily needs for micro-nutrient intake.
Finally, the dietary approach must be something that the client can maintain for the foreseeable future. Adherence to a weight loss/maintenance diet is without question the most difficult part of this process.
It's important to consider adherence when exploring other weight loss options, so that you keep it in mind when evaluating each approach.
The reality is any calorie deficit dietary approach will result in weight loss if the client adheres to it. A study by Dasinger et al (2005) compared a range of dietary strategies for weight loss and concluded that the amount of weight lost was associated more with adherence to a diet, than the type of diet approach used. These findings have been supported by a number of other studies over recent years prompting Freire (2020) to conclude that the diet approach used is not nearly as important as the ability of an individual to adhere to it. There are many factors that influence adherence to a dietary programme including but not limited to food preferences, cultural or regional traditions, food availability, food intolerance and motivation. Having a wide range of dietary options to choose from is a positive, as clients can tailor an approach that gives them the best chance of adherence.
Weight loss solutions need to focus on approaches that can be maintained for the rest of a client’s life. This means they can’t be hugely restrictive as a person will never be able to adhere to them long-term. While a rigid “diet” may be a useful approach to lose an initial amount of weight, there needs to be a longer-term solution in place to ensure the hard work is not undone when the diet ends. Weight loss solutions also need to address the various environmental and social factors that may impact on a client’s ability to adhere to a reduced-calorie diet. All current evidence suggests that a diet approach alone is very unlikely to result in long-term weight loss and management.
Exercise and weight loss
The huge meta-analysis on weight loss approaches by Franz et al (2007) suggested that exercise alone did not compare well with dietary and medication weight loss approaches, but this doesn’t mean exercise is not a meaningful contributor to successful weight loss outcomes. Before we look at the added effect that exercise has when combined with a calorie deficit diet, let’s take a look at the impact of different forms of exercise alone on weight loss.
Cardio and weight loss

Cardio was long thought to be the best exercise to perform to lose weight. This was presumed on the basis that cardio burns more calories during a session than other forms of training. In recent years, however, cardio approaches have been sidelined in favour of resistance and HIIT training approaches with suggestions that doing cardio may even “make you fat”.
This has led to confusion about whether cardio is an effective tool for weight loss. Let’s clear up one thing immediately though. Cardio does not make you fat!
On a whole-body level, aerobic training increases cardiovascular function, aerobic capacity, basal metabolic rate and fat metabolism. Such changes in whole-body metabolism induced by regular aerobic exercise are undoubtedly beneficial to promote weight management.
Dr Jose Antonio (co-founder of the International Society of Sports Nutrition) has written dozens of peer-reviewed articles on the mechanism of weight loss and the role of exercise and states there is more than ample evidence to support the use of cardio exercise for healthy weight management and weight loss including:
- Longitudinal training studies on obese children showing aerobic training results in a loss of body fat.
- Longitudinal training studies on obese adults showing aerobic training results in a loss of body fat.
- Studies reporting that those who do the most cardio over a 15- to 20-year period exhibit the lowest levels of body fat.
- Studies that show athletes that are engaged in highly aerobic exercise have single digit body fat percentages.
- Studies that show cardio athletes with a higher training volume have a lower % fat than those with a lower training volume.
The problem is many of these studies were on athletes (who had never been obese) and those that were performed on obese populations did not account for the diets of the subjects involved.
Thorogood et al (2011) performed a systematic review and meta-analysis of randomised controlled trials assessing the effect of isolated aerobic exercise on weight loss in overweight adults. The review included 14 trials involving 1847 subjects. The duration of the aerobic exercise programmes varied from 12 weeks to 12-months duration. The authors concluded that moderate-intensity cardiovascular exercise induced modest reductions in weight and waist circumference in overweight populations. While consistent aerobic training resulted in multiple cardiovascular and additional health benefits, it was largely ineffective as a weight-loss approach on its own.
Swift et al (2014) agree that large, randomised trials that have evaluated weight loss following aerobic training programmes in line with ASCM physical activity guidelines of 150-250 minutes of moderate to vigorous physical activity a week have observed either no change in weight or modest effects on weight loss (less than 5kg). These authors concluded that overweight and obese adults who adhere to an exercise program consistent with public health recommendations without a dietary plan involving caloric restriction can expect to experience weight loss in a range of no weight loss to approximately 2 kgs. The authors also noted that despite the absence of dramatic weight loss, the numerous additional benefits of cardiovascular training (that can help reverse the negative health impacts of obesity) should not be ignored.
Resistance training and weight loss

Cardio on its own has a very modest effect on weight loss, what about lifting weights?
Unfortunately, it appears that resistance training on its own has a similar (moderate) effect on weight loss to cardio when performed in isolation. Wewege et al (2021) performed a systematic review and meta-analysis on the effect of resistance training in healthy adults. Their review of 58 studies found that resistance training elicits average reductions of 1.4% body fat percentage and 0.55kg of fat mass compared to non-exercise control groups.
In obese populations, the results were marginally better. Lopez et al (2022) performed a systematic review and meta-analysis on the effect of resistance training on the body composition and weight of overweight and obese individuals. They analysed 115 related articles and reported overall average reductions in fat mass of 1.6% or 1kg of fat mass in obese populations. The average duration of the resistance training programmes in the studies was around 16 weeks. Overall weight loss was not common in these trials (in fact some individuals gained weight), however, this was likely the result of increased lean body mass (muscle tissue).
So, it would appear that simply starting an aerobic or resistance training programme (and changing nothing else) will have little overall effect on weight loss, although both can offer numerous benefits in terms of health.
Choosing an exercise mode
Direct comparisons between the training modes have also been made in relation to weight loss. Willis et al (2012) compared the effects of aerobic and/or resistance training on body mass and fat mass in 119 obese adults. The subjects were randomly assigned to one of three groups.
- Resistance Training.
- Aerobic Training.
- Resistance and aerobic training.
The results of the 4-month trial were as follows:
- The aerobic training and resistance/aerobic training groups reduced fat mass and total body mass more than the resistance training group but were not significantly different from each other.
- The resistance training and resistance/aerobic training groups increased lean mass (muscle) more than the aerobic training group.
- While requiring double the time commitment, the resistance training/aerobic training group did not lose significantly more fat mass or body mass than the aerobic group
The authors concluded that balancing time commitments against health benefits, it appears that aerobic training is the optimal mode for reducing fat mass and body mass, while a programme including resistance training is needed for increasing lean mass.
Based on the discussion above, there is an argument that focusing on exercise is not the answer when it comes to weight loss. However, weight loss expert Dr Len Kravitz of the University of New Mexico maintains that “Exercise is the number one predictor of weight-loss success”.
While the individual effects of exercise modes have a modest effect on weight loss when done in isolation when exercise is combined with a calorie-deficit diet approach, we start to see more significant results.
Combining exercise with a calorie-deficit diet
A pioneering study performed by Kraemer et al (1999) looked at the influence of exercise training on weight loss in men over 12 weeks. In the study, 35 men were placed randomly into either a control group (who did nothing), or one of three diet/exercise groups. One group followed a calorie restriction diet only, one group followed the same diet and completed three 45-minute cardio sessions a week, the final group did the same as the second group but added 2 resistance training sessions a week. The results of the study can be seen in the image below:
While the overall weight loss resulting from each intervention was not significantly different, the percentage of weight tha was lost as fat was drastically affected by the intervention approach. Here are the most significant findings from the study:
- All three interventions resulted in a significant loss of weight (around 9kg) compared to the control group.
- Body mass was significantly decreased for all intervention groups at week 6 and continued to decrease (at a slower rate) from week 6-12.
- Percent of body fat and fat mass were also significantly reduced for all intervention groups at week 12, however, the group that performed aerobic and resistance training achieved significantly greater losses of body fat than the other groups.
- Further analysis showed that the percentage of weight lost as body fat was 69% for the diet-only group, 76% for the diet and cardio group and 97% for the diet, cardio and resistance group.
The authors concluded that while resistance training alone offers no clear benefit to weight loss over dieting, but it does preserve lean tissue despite consuming a calorie deficit diet. This is thought to be important as muscle is very metabolically active tissue and can contribute to elevated ongoing calorie expenditure even during periods of rest.
In contrast, 31% of all weight lost during dieting alone is reported to be lean tissue (mainly muscle and up to 1% bone. The addition of cardio preserves a little more lean tissue, but performing resistance training appears to preserve lean tissue resulting in similar levels of weight loss, but significantly more fat loss than dieting alone or dieting with cardio.
The research is clear on this. A meta-analysis by Wu et al (2009) that included studies involving over 1600 participants concluded that combining calorie-deficit diet approaches with regular exercise consistently resulted in significantly greater weight loss (and body fat loss) outcomes than diet interventions alone. This has been found to be the case in both short-term and long-term weight loss in adults. The inclusion of cardiovascular exercise modes elicits a number of other positive health benefits (particularly in regard to cardiovascular disease and diabetes risk). It is also thought to target dangerous visceral fat stores (i.e. the fat stored around organs). The inclusion of resistance training preserves lean tissue mass during weight loss, which may provide additional metabolic enhancements for weight loss.
A more recent review of the literature (116 studies) by Lopez et al (2022) agreed with the above findings suggesting that little separated cardiovascular and resistance training in terms of their individual impact on weight loss, but that when used in conjunction with a calorie deficit diet, exercise could maximise fat losses as opposed to simply weight. These authors concluded that resistance training combined with calorie restriction was the most effective exercise approach for reducing body fat percentage with an average reduction of around 4kg in most studies (averaging 16 weeks), but that the largest fat mass (kg) reductions were seen in interventions combining calorie restriction, resistance training and cardio (average of 5.1kg of fat lost in 16 weeks).
In summary, both cardio and resistance training approaches appear beneficial in conjunction with calorie restriction diets and offer complimentary benefits that cannot be obtained by doing one or the other. Evidence suggests that the most successful outcomes will come from multi-dimensional approaches that include both exercise modes.
Engaging in resistance training to build muscle mass has been proposed to potentially raise the basal metabolic rate. This could be advantageous for individuals aiming for weight loss, as it means they'll continue to burn calories at a heightened rate, even during periods of rest.
There are also claims that some forms of exercise elicit enhanced calorie expenditure in the hours following exercise that could also contribute to additional weight loss.
Let’s explore these claims.
A systematic review and meta-analysis performed by Mackenzie et al (2020) analysed 18 articles that explored the effect of exercise on resting metabolic rate and concluded that while aerobic exercise and combined aerobic and resistance training protocols did not significantly alter resting metabolic rate, resistance training protocols that increased muscle mass did appear to significantly increase resting metabolic rates compared to control groups. The mechanism by which this is achieved is thought to be that meaningful increases in lean mass (muscle) increases metabolic rate due to greater volumes of metabolically active tissue, and the increased rate of remodelling of muscle tissue post-exercise (repair of exercise-induced damage). While there were some limitations raised in the studies analysed, the authors were confident that resistance training protocols that increased muscle size, would lead to increased metabolic rate. This suggests that for weight loss clients, maintaining or increasing muscle mass through resistance training protocols will lead to an increase in BMR and result in additional calorie expenditure.
In order to answer this question, you need a measure of calorie expenditure. Elevated post-exercise calorie consumption (above resting values) can be measured as EPOC. EPOC stands for Excess Post Oxygen Consumption and represents the amount of additional oxygen consumed by the body tissues per minute following exercise. This is the additional oxygen that the body requires to replenish oxygen and ATP-PC stores in muscle and remove lactate from muscle. It is facilitated by increased breathing rate, blood circulation and body temperature that are maintained at rates above resting levels for some time after exercise (Vella and Kravitz, 2004).
EPOC can help you calculate additional energy expenditure after exercise, as for every additional litre of oxygen consumed above normal resting values 5 calories are burned (Vella and Kravitz, 2004). Studies have found that the magnitude (amount of elevation in oxygen consumption) and duration (length of time the oxygen consumption is elevated) of EPOC are dependent on the intensity and duration of exercise.
EPOC and cardio exercise
The intensity of cardio exercise has the greatest impact on EPOC. As exercise intensity increases, both the magnitude and duration of EPOC increase. This is thought to occur because, during higher-intensity efforts, the body goes into a greater amount of oxygen debt and has to pay this back at the end of the session. Therefore, the higher the intensity of the exercise session, the greater the EPOC (and therefore calories expended) post-exercise.
Bahr and Sejersted (1991) monitored the EPOC of subjects who completed 80 minutes of cardio at 29%, 50% and 75% of VO2 max effort and found that the exercise intensity dictated not only the magnitude of the EPOC effect (e.g. the 75% effort group achieved 187% more EPOC than the 50% effort group) but also the duration over which EPOC occurred. The group that trained at 75% effort continued to burn additional calories for 10.5 hours compared to 0.3 hours for the 29% effort group and 3.3 hours for the 50% effort group). These results have been replicated in a number of additional studies to date.
The following image depicts the effect of intensity on EPOC post-training. The orange segment represents the magnitude of EPOC following exercises of different intensities.
Studies have also compared the effect of high-intensity interval training vs. steady-state cardio on EPOC. The image below shows how the magnitude and duration of EPOC are affected by these different approaches. The top part of the image looks at the EPOC effect of a classic 1-hour constant-pace cardio session, while the bottom of the image depicts the EPOC effect of a 12-minute HIIT session (where the effects can be seen to last for upwards of 24 hours). It should be noted, however, that the calorie-burn during an hour's running would outweigh the calories burned in a 12-minute HIIT session.
Duration of cardio exercise also appears to have an important influence on EPOC. Chad and Wenger (1988) investigated the effects of exercise duration (30, 45, and 60 minutes) at 70% VO2 max on EPOC. They reported EPOC values of 6.6 litres (33 calories over 128 minutes), 14.9 litres (74.5 calories over 204 minutes) and 33 litres (156 calories over 455 minutes) for durations of 30, 45, and 60 minutes, respectively. It was concluded that increasing exercise duration would significantly increase total EPOC. These results have also been backed up by a number of subsequent studies (Vella and Kravitz, 2004).
Differences in EPOC have also been noted for the following exercise comparisons:
- Continuous running for 30 minutes at 70% of VO2 Max vs. an interval session of 20 x 1 minute 100% efforts. The interval training session resulted in 117% more EPOC effect (Larforgia et al, 1997)
- 2 x 25-minute runs at 75% VO2 Max vs. 1 x 50-minute run at 75% VO2 max. The 2-interval session resulted in double the EPOC effect (Kaminski et al, 1990).
EPOC and resistance training
It appears resistance training can also have a beneficial EPOC effect for weight management/loss although fewer studies have been conducted in this form of training on its own. Elliot et al (1988) compared the difference in EPOC between aerobic cycling (40 minutes at 80% HR max), circuit training (4 sets, 8 exercises, 15 reps at 50% of 1RM) and heavy resistance training (3 sets, 8 exercises, 3-8 reps at 80-90% of1RM) and found that heavy resistance training produced the greatest EPOC (despite having the lowest calorie burn during the session). The results of the study are shown below:
The intensity of resistance training also seems to matter. Thornton and Potteiger (2002) compared two resistance training workouts. One completed 2 sets of each exercise for 8 reps at 85% of 1RM, while the other performed 2 sets of 15 reps at 45% of 1RM. Results of the study clearly showed that the higher-intensity lifting session had a more profound effect on EPOC.
Finally, and most impressively, the difference in the duration of the EPOC effect between steady-state cardio and resistance training was examined by Shuenke et al (2002) who measured the EPOC effect of a 31-minute high-intensity resistance training workout consisting of 4 rounds of bench press, power clean and squat (10 reps at 10RM to failure) with 2 minutes rest between each exercise. This was compared to the EPOC effect of a steady-state cardio session of the same duration. As the image below clearly shows, the EPOC effect lasted for up to 48 hours for the resistance training session and only around 7.5 hours for the cardio session.
This effectively means that if a meaningful resistance training session is completed every 2 days, it is unlikely a person’s BMR will ever return to baseline levels.
Key Insights
- Train above 70% VO2 max for the highest EPOC effect.
- Longer is better for EPOC effect.
- High-intensity cardio intervals are more effective than continuous exercise.
- Two shorter workouts yield higher EPOC than 1 long one.
- Use high-intensity strength training over cardio for EPOC.
- Circuit training also elicits a meaningful EPOC effect
While different forms of exercise elicit different EPOC responses, the positive news is that any additional calorie expenditure post-exercise can add up over time and contribute to weight loss/management. However, in reality, most obese populations are incapable of working out at meaningful intensities and durations. The initial focus of any PT should be to gradually improve the physical condition of their weight loss clients so that they can perform meaningful intensity exercise for over 30 minutes in a session. This will enable them to benefit from additional EPOC calorie expenditure.
Combining exercise with a calorie deficit diet is the most effective strategy for achieving sustainable weight loss results. Nevertheless, it's important to acknowledge that individuals in the obese population often face challenges when it comes to embracing regular exercise.
Thomas et al (2008) conducted a qualitative investigation of dieting, weight loss and physical exercise, in obese individuals. They conducted open-ended interviews with 76 obese adults living in Victoria (Australia) to get a real sense of their feelings towards exercise. Here are the key findings of their investigation:
- While the participants of the study repeatedly turned to commercial diets in their attempts to lose weight, few had used or were motivated to participate in physical activity.
- When asked if they had tried exercising for weight loss, the participants gave a number of barriers that prevented them from doing so. 83% of the participants said they found exercising difficult because of their weight or physical health problems and could not afford gym subscriptions or personal trainers. Many stated that they didn’t have time to exercise or felt uncomfortable or embarrassed taking part in organised exercise activities. Many spoke of feeling emotionally humiliated, embarrassed or daunted when they attempted to exercise on their own.
- Other reasons for not exercising included it being too dark when they get home from work to go for a walk, or that they “felt fat”, were “too lazy”, or “couldn’t be bothered”.
- Many participants stated that it was very difficult to exercise on their own, and wanted interventions in which someone else would take responsibility for motivating them to be more physically active (e.g. a personal trainer).
There is also evidence that suggests unless a person does a considerable amount of structured exercise, their own body can simply work against them employing compensatory measures to counter the limited exercise they are doing. For example, after many people perform an exercise session, they often have increased appetites and this, combined with a reward mentality or “I’ve earned it”, can lead to consuming more calories than were burned in the exercise session. There is also evidence that once we have exercised, we tend to move less through the remainder of the day, and that metabolic compensatory changes may also occur leading to reduced metabolic rates as we get slimmer. This means it is becoming more obvious that exercise is simply part of the solution. This short video explains the drawbacks of relying on exercise to achieve weight loss goals and why this approach doesn’t always work.
The “NEAT” way to increase calorie expenditure
Indeed, we understand that engaging in regular exercise, along with adopting a calorie-deficit diet, is a proven approach to achieving and sustaining weight loss. However, it's important to acknowledge that individuals struggling with obesity may face challenges when it comes to embracing physical activity. Even those who manage to muster the motivation for a few weekly gym sessions may find it difficult to accrue a substantial amount of exercise, which could limit the initial impact on weight loss when compared to dietary changes alone. Additionally, external factors beyond their control may further affect the effectiveness of their initial exercise endeavours.
This is because clients new to exercise need to increase their “ability to exercise” before many of the scientific benefits of exercise for weight loss can be realised. But not all calorie expenditure through movement needs to be structured, or intense. Strategies that motivate obese clients to move more across their day can have a meaningful impact on calorie expenditure.
Non-Exercise Activity Thermogenesis (NEAT) is a term used to describe energy expenditure caused by movement that is not classed as “exercise”. Looking for simple ways in which to increase the amount a client moves during the day can have a significant impact on the calories they burn a day. Here is an example to illustrate the impact of these changes.
A 66kg person burns approximately 102 calories an hour while performing their office job seated at a desk (approximately 1.7 calories/minute). If they were to stand while performing the same duties, they would burn 174 calories an hour. While an additional 72 calories an hour doesn’t seem a lot, even if this person were to stand for a couple of hours a day at work, they would burn an additional 144 calories a day. Multiply that by 5 working days and it translates to 720 additional calories burned a week. Over the course of a 48-week working year, that adds up to 34,560 calories a year of additional calorie burn (around 10kg of body fat). That is the equivalent of over a hundred 30-minute jogs!
Increasing a client’s NEAT is a simple way to encourage additional calorie expenditure throughout the day and is less confronting than beginning a structured exercise programme. Comana (n.d.) recommends these practical steps for increasing daily NEAT:
- Stand more. Start by attempting to stand or move about for 5 to 10-minute increments while you complete various daily activities.
- Take the stairs instead of lifts and escalators
- Take the long way to the water cooler or bathroom at the office.
- Walk to a co-worker's desk instead of emailing or calling them.
- Stand or walk whenever you talk on the phone.
Once some of these are embedded into daily routines, more NEAT activities can be added like parking further away from the office, walking or taking public transport to work, taking walking breaks instead of just eating breaks and having standing or walking meetings.
Try it out
Let’s see what new knowledge you have managed to pick up about the best approaches for weight loss. Complete the three questions on each slide. Click on the arrows below to toggle between the slides.
Predictors of successful weight loss
Many people are successful in losing weight in the short term using a combination of diet and exercise, but a common problem faced by many is weight regain. Obesity interventions typically result in early rapid weight loss followed by a plateau and progressive regain. A meta-analysis of 29 long-term weight loss studies reported that more than half of the lost weight was regained within two years, and 80% of the lost weight was regained within 5 years (Wu et al, 2009). The image below shows the pattern of weight loss from clients in these 29 studies.
Before discussing the predictors of successful weight loss, it is important to fully understand why so many attempts at weight loss fail in the long term. Hall and Kahan (2018) believe that the reason most people are unsuccessful in their weight loss attempts is because of overlapping physiological changes that occur during initial weight loss (i.e. the way the body adapts to the initial weight loss).
The most identified of these physiological changes are reductions in metabolism and increases in appetite. Hall and Kahan (2018) suggest that the feedback circuit controlling long-term calorie intake has greater overall strength than the feedback circuit controlling calorie expenditure citing research that suggests that for every 1kg of lost weight, calorie expenditure decreases by about 20-30 calories a day, whereas appetite increases by around 100 calories a day (above baseline levels prior to weight loss). In simple terms, as weight is lost, metabolism begins to slow (as less cells to keep alive). The body also recognises it is in a state of caloric deficit, and so does what it is biologically primed to do – increase appetite. These are believed to be the key mechanisms that lead to weight plateaus and ultimately weight regain.
Rather than a lack of willpower on the part of the individual, the plateau and regain of weight following initial weight loss success is likely due to these compensatory physiological actions. It is thought that the steady increase in appetite as weight is lost leads a constant battle to avoid eating to match the new motivations to eat. This leads to constant thinking about food and allows sub-conscious biases (such as portion sizes creeping up over time). These increases are subtle. From a pure calorie perspective, these individuals may only be eating an additional 100 calories a day than someone who manages to keep the weight off (Hall and Kahan, 2018).
There are many factors that account for the ability of some individuals maintaining weight loss over the long term, while others experience substantial weight regain.
We have already discussed the importance of choosing to follow a weight loss strategy that can be maintained in the long term, but what are the predictors of long-term weight loss success?
Hall and Kahan (2018) completed a review of the literature and summarised the current understanding of the behavioural factors that correlate with successful maintenance of lost weight. Here are some of their key findings:
Long-term success requires ongoing support and attention
Even the most successful short-term weight strategy will fail to yield continued positive outcomes without maintaining some form of intervention and support. There are several studies that have shown that ongoing interaction with healthcare providers or groups that track progress significantly improves long-term weight outcomes. The longer the support and tracking continue, the better the outcomes appear to be. This graph from a study by Perri et al (1988) shows the effect of maintenance support visits on weight regain in weight loss clients.
Necessary client behaviours
Research has provided a series of strategies that appear to aid ongoing success including the following client behaviours:
- Frequent self-monitoring and self-weighing
- Ongoing reduced calorie intake
- Increased physical activity levels
- Eating breakfast
- Eating at home rather than buying food outside of home
- Reducing screen time
- Use of portion-controlled meals or meal substitutes for some intakes
Weight-loss counselling strategies
Strategies that have been proven to assist these ongoing client behaviours include:
- Assisting clients to help anticipate struggles and danger environments. This involves frank discussion about upcoming events (e.g. holidays, Christmas, work-do, etc) and formulating action plans for these.
- Helping clients recognise when “behavioural fatigue” is setting in (i.e. the inevitable point where they become bored with the process) and techniques to counter this (these are coming up).
- Helping clients put the inevitable slip-ups into perspective (bigger picture thinking) and the formation of contingency plans for when they do slip up.
- Helping clients develop “cognitive flexibility” - Many clients develop an “all or nothing” mindset to weight loss. It is important that clients are able to accept that perfect adherence to strict weight loss regimes is almost impossible over the long term and that they can develop cognitive flexibility to take in stride when things do not always go to plan. This is considered one of the core competencies for life-long sustainable weight management.
- Manage expectations – Allowing clients to have wildly unrealistic expectations about continuing weight loss is a dangerous practice. Ongoing weight loss is also not a linear progression. There will be plateaus and partial regain of weight throughout the rest of their life. A fully informed client with realistic expectations for weight loss is less likely to suffer the disappointment of not achieving weight loss at the rate they hoped. This disappointment often leads to waning motivation and conclusions that the effort is not worth the result. Preparing clients for the fact that longer-term improvements are harder earned and in smaller increments is vital to keep them motivated. This involves the setting of realistic goals, that are adapted for the stage of the process.
Ongoing use of results
During the initial weight loss, the key focus was on the scales (and the decreasing weight). Once a desirable level of weight loss has been achieved, the power of this external stimulus is reduced. To support motivation, it is important that other areas of improvement are given attention. Outcomes such as improvements in risk factors, girth measures, improvements in lean body mass, clothing size, progress photos, gym performance etc. are all powerful reminders of progress. Weight loss should not be the sole metric of obesity treatment success. A myriad of other health benefits can also be obtained from adopting healthier behaviours and can occur in the absence of major weight loss.
Appeal to a client’s deeper motivations
While external, superficial rewards appear to motivate short-term weight-loss, longer-term success is only likely when client’s take ownership of their behavioural changes and goals and engage in them because they actually enjoy them. Examples of how deeper motivations influence the ability of people to stick to strict diet patterns can be seen in the various religious or cultural kosher, halal, or vegan eating practices. Millions of people around the world stick to these practices because they align with their religious, ethical or other deeply held beliefs and values. If a client can connect meaningful value to ongoing healthy eating and behaviour practices, they are more likely to adhere to them long-term. Conversely, prescribing daily gym sessions to someone who hates the gym is unlikely to prove successful long term. As PTs, we should be supporting clients to find more enjoyable physical activities that they will engage in.
Recognise when it is time to refer on
Any clients who do not achieve sufficient weight loss or health improvement under your guidance should be referred to a registered dietician or alternative specialist (e.g. behavioural psychologist or hypnotherapist). This will allow an expert to delve deeper into why weight loss is not occurring, allow them to apply additional strategies to combat any barriers to weight loss, and may open up pathways for intensified therapies (such as surgery or obesity medications). These can only be prescribed by appropriately qualified specialists and can be used alongside regular exercise and diet to elicit results.
The National Weight Control Registry
Well-conducted research should always form the basis for any recommendations regarding nutrition or exercise. Much of the research presented on this topic has been derived from clinical trials and reviews. Personal experience and opinions of those who work in the field of weight loss can then be used to supplement what we know from research. However, sometimes the weight of anecdotal evidence is too large to ignore!
The National Weight Control Registry was established in 1994 at the Brown Medical School at the University of Colorado. It is the largest prospective investigation into long-term weight loss maintenance. Instead of relying on what previous research has to say, the registry collects data from individuals who have lost a significant amount of weight and managed to keep it off. In essence, the registry compiles data on the approaches that individuals (with long-term weight loss success) used and shares these to update public knowledge.
The data that the National Weight Control Registry compiles has come from well over 10,000 individuals enrolled in the study who have lost at least 13.5kg and kept it off for at least 1 year. The registry uses detailed questionnaires and annual follow-up surveys to examine the behavioural and psychological characteristics of weight loss “maintainers”, as well as the strategies they use to maintain weight loss.
Main findings from the data
Registry participant details
- 80% of participants in the registry are women and 20% are men
- The "average" woman on the registry is 45 years of age and currently weighs 66kg while the "average" man is 49 years of age and currently weighs 86kg.
Weight loss details
- The collective registry members have lost an average of 30kg each and kept it off for approximately 5.5 years.
- These averages, however, hide a lot of diversity: Weight losses have ranged from 13.5kg to 136kg.
- Duration of successful weight loss has ranged from 1 year to 66 years!
- Some have lost the weight rapidly, while others have lost weight very slowly--over as many as 14 years.
How they lost the weight
- 45% of registry participants lost the weight on their own and the other 55% lost weight with the help of some type of program.
- 98% of Registry participants report that they modified their food intake to achieve a calorie deficit
- 94% increased their physical activity, with the most frequently reported form of activity being walking.
How they kept the weight off
- Almost all participants report continuing to maintain a calorie-deficit diet (mainly achieved through a low-fat focus)
- Almost all report having high levels of activity - 90% exercise, on average, about 1 hour per day.
- 78% eat breakfast every day.
- 75% weigh themselves at least once a week.
- 62% watch less than 10 hours of TV per week.
Through the use of questionnaires, the registry is able to report that National Weight Control Registry members:
- Are now accepting of their body shape
- Have learned how to confront their problems (vs. eating to cope)
- Recognise that they need to continue the process ongoingly
- Found it easier to maintain weight after 2-years of adherence to their weight loss approach
- Are physically active (at least 250mins a week)
- Have identified and consciously limit their intake of known "danger foods"
- Consciously limit dietary fat
- Self-monitor their intakes and behaviours
- Eat a healthy breakfast every day
- Eat some favourite foods without associated guilt
- Are realistic about weight loss expectations
Continued adherence to diet and exercise strategies, low levels of depression and dis-inhibition, and medical triggers for weight loss were also associated with long-term success.
This information provides a wealth of information to supplement clinical research. It also offers some real motivation for those embarking on a weight loss journey because it shows weight loss (and maintenance of weight loss) can be achieved and it can be achieved in a number of different ways. The information also highlights that there are some consistent behaviours shown by the members of the registry that may offer insight into the best way to approach a weight loss goal. Of these consistent behaviours three key facts stand out:
- The members report being highly active and limit screen time to less than 10 hours a week
- The members maintain a calorie deficit, but still allow themselves some of the foods they enjoy
- The members self-monitor their progress showing that they are taking ownership of their progress
Additional research has also helped us understand the traits of individuals who are successful in their long-term weight loss journey. The following table is a collection of the key traits collated from a number of sources that are associated with long-term success vs weight re-gain:
| Those who are likely to succeed | Those who are least likely to succeed |
|---|---|
|
|
Enhancing motivation and adherence in weight loss clients
So, what can we yield from all the information we have covered so far?
Eat a controlled diet that ensures a calorie deficit (but provides all the healthful nutrients you need). Avoid known danger foods but allow yourself some treats. Do daily activity (a mix of cardio and resistance training), while increasing the amount you move across a day also. Ensure your goals are realistic, monitor yourself regularly, and limit your screen time. Do all of this, even when you don’t feel like it, and you will lose significant weight. If you continue to do it for more than a couple of years, your chances of regaining weight diminish.
But what of your average PT client? Would this approach appeal? Is it realistic in a PT setting? Outlining this approach in full would scare off most new clients on the first day of their weight loss journey!
The best nutrition plan and exercise regime in the world won't work unless a person sticks at it over time. The most important thing in all of this is that we help create a weight loss approach that can be maintained for the foreseeable future.
One of the keywords in reversing the effects of obesity is “motivation”.
The following acronym emphasises various aspects of motivation that can be particularly important for obese individuals working towards weight loss goals.
| Mindset | Maintaining a positive and determined mindset is crucial. |
| Obstacle | Overcoming barriers and challenges along the way. |
| Tracking | Monitoring progress and celebrating small victories. |
| Initiative | Taking proactive steps towards a healthier lifestyle. |
| Variety | Incorporating diverse exercises and nutritious foods. |
| Adaptability | Being flexible and adjusting to changing circumstances. |
| Tenacity | Showing persistence and not giving up easily. |
| Incentives | Providing rewards or motivations for achieving milestones. |
| Optimism | Focusing on the potential for success and positive outcomes. |
| Nurturing | Taking care of oneself physically and emotionally. |
To be successful long-term, a client must be motivated to do the following:
- exercise daily.
- modify the diet to create a consistent calorie deficit.
- modify their lifestyle. (This may involve changing their living and social environments in some cases).
- do all of the above even when they don't feel like it.
Overweight clients typically seek external motivation from a personal trainer (PT) due to a lack of intrinsic drive. Initially, external motivation, whether it be financial incentives or the desire to please others, can effectively kickstart weight loss. However, for sustained success, fostering intrinsic motivation becomes paramount. Encouraging clients to assume some accountability for their progress should be a central emphasis for any PT working with individuals on a weight loss journey.
We have learned that a successful approach to long-term weight loss outcomes is multi-factorial. Many individuals attempting to lose weight (and their trainers) try to change too many elements of their lifestyle at once. This may be possible at the very start of the process as their motivation is usually higher at this point, but very quickly this can lead to them becoming overwhelmed and giving up.
Personal trainers must remember that in order to become obese, these clients have likely made poor dietary choices over a long period of time (maybe even a lifetime) and followed a very sedentary lifestyle. Expecting these clients to simply flick a switch and convert to a healthy diet and regular exercise is a mistake that many inexperienced personal trainers make. This usually results in a very hungry, tired and sore client within a very short period of time.
A guide for adherence in weight loss journey
The simpler we can make the transition to a healthier lifestyle, the better the chances of adherence and success. Here are some considerations for PTs and their clients who are starting out on a weight loss journey:
Set realistic goals and timelines
Set realistic goals and timelines for weight loss. The client needs to understand that sustainable weight loss is not a quick fix. Most research indicates that a person following a 500-calorie deficit diet combined with exercise could realistically expect an average of 500g per week of weight loss. Share your knowledge with the client, answer their questions and explain in detail the approaches that have been proven to elicit the best long-term outcomes. This may require frank discussions with the client who will likely have pre-conceived (and often unrealistic) expectations of what works.
Make small initial changes
Make small changes initially. While the best weight loss approaches are multi-dimensional, don’t try to implement every strategy at once! As a personal trainer, your primary objective is to help the client with the exercise component of their weight loss journey. If they are new to exercise, ease them into things slowly. Understand that carrying additional weight comes with an increased likelihood of discomfort and joint pain. The initial goal of the exercise sessions should be to make the client feel comfortable in the environment and gradually build their tolerance for exercise.
Choose modes of exercise that you think the client will enjoy (or hate least). Seek feedback from the client at regular intervals and adjust workouts based on this feedback. The research on this is clear, adherence is the most important factor when it comes to the benefit of exercise for weight loss. In weight loss experiments involving exercise interventions, those who attended the most sessions achieved greater weight loss (Byrne et al, 2012).
The same approach should be used for dietary measures. Rather than completely overhauling the client’s diet, start with the “big rocks”. It is very unlikely that a client can simply convert immediately to a calorie-deficit diet on day one. Instead, have discussions with the client and identify the "danger foods" that the client eats often and finds hard to limit their intake of. From there, you can continue to implement small to the diet working towards a dietary approach they can maintain for the long term.
Schedule regular check-ins
Have regular, scheduled check-in sessions with clients. During these sessions, you should discuss how the changes that the client has implemented are going. Have they been able to adhere to the dietary changes? How are they finding the exercise programme? Use the information you gain from these discussions to tweak/progress the approach for continued results. Remind clients that slip-ups are likely to occur from time to time, but that no one event should derail the overall approach. Helping clients deal with slip-ups is a vital part of the process.
Share diverse measures of progress
Regularly share results with the client. It is important that a variety of measures are taken (not just weight loss alone). Weight loss during different periods of the approach will be irregular (sometimes lots, sometimes a little and sometimes none at all). Measures other than weight loss can include:
- Health measures like girths, blood pressure, resting heart rate and cholesterol levels
- Performance measures like weight lifted, endurance improvements, or volume of exercise completed
- Mood measures like happiness, positivity, self-confidence, stress levels etc.
Sharing and celebrating client success is paramount to a successful weight loss outcome. Regular feelings of success build self-efficacy in the client. This is the feeling that what they are doing is working. Byrne et al (2012) suggests changes in self-efficacy during a weight loss intervention is one of the main predictors of long-term success. Most obese people starting a weight loss journey have reservations as to whether the interventions will work. This is often because they have tried multiple times to lose weight before and failed. Remind clients of how far they have come and the great results they have already achieved.
Shift responsibility to the client
Once the initial approach starts to show results, it is time to start working on shifting the responsibility of the exercise approach to the client. Strategies to achieve this include setting daily activity goals for the client to complete (away from scheduled sessions). These do not have to be structured exercise sessions but could revolve around reducing time spent sitting, reaching a designated step count, or completing a walking distance challenge. There are many free apps that a client can use to collect this data so that it can be shared with the PT at regular intervals. If the client is to achieve long-term weight loss, they cannot simply rely on sessions with their PT. They must find the motivation to move with purpose daily.
Watch for signs of behavioural fatigue
Watch out for signs of “behaviour fatigue”. This means a client is starting to tire of the process. It often creeps in as the rate of weight loss plateaus or slows down and clients start to question the value of putting in the work. Signs of behavioural fatigue can be both verbal and physical in nature. Negative comments or irritability around the process and reduced rates of adherence to exercise or dietary measures are obvious signs. This is where PTs can make a big difference. Change the exercise approach by introducing something new, fun or different. Change the dietary approach for a short time. An example often used by PTs to kick-start motivation is to combine a light, fun exercise approach, with a lower carbohydrate diet for a week. This can often refresh the client and lead to a quick drop in water weight (which can also be motivating). Often these slumps are associated with other work or relationship stresses. Simply getting through the week can lead to a change in mood and motivation the following week.
Four steps to behavioural change
Certified Nutritionist and weight loss specialist Robert Yang developed a "4-steps to change" approach for weight loss in 2013 that has been used by thousands of trainers around the world with great success. His approach works on the belief that “the more changes you make to a client’s diet at once, the less chance they will adhere.”
Yang’s 4-step process is simplistic and cyclic (i.e. it is ongoing). It provides a simple framework for health professionals to use to implement progressive change to the weight loss approach without overwhelming the client. Each of the four steps is implemented in a four-week approach.
Week 1: Eliminate some of the bad (and introduce some good stuff)

Help the client identify the worst parts of their diet and start by cutting back on these things. For example, if a client drinks a 1.5L bottle of Coke every day, start by reducing the amount back to 1 600ml bottle. If the client buys takeaways 5 times a week, reduce this to twice a week. The next step is to help them find lower-calorie solutions to replace the bad stuff, while not completely changing everything. An example of this could be replacing the additional Coke with soda water and a dash of lime cordial. The reduction in takeaway meals might require a couple of simple recipes that the client can use to make food at home. Remember, it is only week one! Changes do not have to be drastic to start getting results. The objective of this week should be to make small, easily implemented changes that will add up to significant calorie reductions (and therefore a calorie deficit over current practices). For example, simply cutting the Coke back will reduce calorie intake by over 400cal a day. The items that need reducing are usually easy to identify (e.g. whole blocks of chocolate at night, big bags of chips as a snack etc.). From an activity perspective, simple attempts to increase NEAT could be made during this week. The focus should be about implementing a few strategies to increase calorie expenditure across the day. These should be simple strategies to reduce time spent sitting and increase time spent moving. Setting movement targets is a great way of doing this but it is vital that the targets are achievable.
Week 2: Increase the amounts of good foods
In week two, the changes you made in week one continue. Additionally, begin to identify some simple ways in which the client can start to increase their intake of healthy foods. This can be as simple as introducing a healthy breakfast daily and suggesting snacks of fruits, vegetables and low-fat, high-protein items when hungry instead of regular processed foods. Another much-used approach is to make and take a healthy lunch to work. These are two simple changes that are easily controlled but can make a huge difference to both the quality and calorie density of food consumed. Again, this should not be a complete swap out of foods, but rather the replacement of a few key items that will have the most significant impact on calorie intake. This week can also involve a focus on portion size and appetite monitoring. Small additions to increase NEAT would also be appropriate during this week.
Week 3: Increase activity levels
The changes made in weeks 1 and 2 are simply maintained. The focus of week three is exercise. This client has come to you in a personal training environment. It is time to start ramping up their exercise this week. This could involve a small shift in training volume or intensity, or an extra scheduled session (either with you or on their own). This week will see the setting of some new exercise goals that can be reviewed in 4-weeks time. The usual rules of exercise progression should apply here. Pay particular focus to pre-exercise nutrition to ensure that the client is still well-fuelled prior to these sessions so you are able to get the most out of them.
Week 4: Check in, re-balance and mood
Changes made in weeks 1-3 continue. The focus of this week is to assess how the changes you have implemented so far are going. How well is the client adhering to these changes? How hard have they been to stick to? If the client has had real trouble with the initial changes, there is little point in making even more changes at this point. Instead, the focus should be on developing strategies that will improve adherence. This should also be a time for assessing other peripheral factors that contribute to weight loss like mood, sleep, motivation and overall mind space in response to the changes that have been initiated. If all indications are that the initial changes are being coped with well, it’s time to roll out the next 4-week cycle!
This 4-week approach is continuous. The first week of each cycle would see a focus on further cleaning up the worst parts of the diet that remain. As time goes on, you will often notice that the client makes more of these changes on their own. The second week of each cycle will see more good foods introduced. Depending on the cooking skills of the client, these suggestions may also include simple recipes for tasty, healthy snacks and meals. The third week of the cycle is where the activity levels are further progressed. Once an increased tolerance for exercise has been developed, you can start to employ progressive overload strategies to achieve even better results through exercise. The fourth week of the cycle is arguably the most important. Don’t expect each cycle to result in linear improvements. There are times when the changes you have made will be too much for the client and a re-think of the approach will be necessary. This re-balance week is a chance to measure progress and share results, understand how the changes you have implemented are impacting the client and offer the opportunity to apply strategies to help the client problem-solve when sticking points arise.
Ultimately, the aim of this process is to have the client take responsibility for the ongoing dietary and exercise approach. This can only happen if you fully involve them in the decision-making processes throughout the early part of the process and explain to them at every point along the way the rationale for the changes being made. By slowly handing over the reins to the client, you develop their ability to control their own destiny, while still being a source of support. This is the only way to ensure long-term success.
It is well within the PT's scope of practice to work with obese populations to help them achieve weight loss as long as they are using evidence-based approaches. Under no circumstances should a PT prescribe or validate the use of a fad diet or weight loss supplement to a client. Using the approaches discussed above and applying the Ministry of Health eating and activity guidelines will go a long way toward positive outcomes of weight loss with obese clients.
If the approaches above do not appear to cause positive change, or if you suspect deeper psychological or medical issues are the root cause of the weight issue, then it is recommended that a client should be referred to a qualified nutrition expert for assessment. Clear communication between this expert and the personal trainer should then be initiated, so that all parties are working together to achieve the same goal and the client is not subjected to mixed messages.
Referral is also suggested if initial approaches involving dietary intervention and exercise are unsuccessful. This indicates that another area of the client’s behaviour is undermining the approaches and a deeper level of analysis may be required. Referral to a specialist may also be useful in times when weight loss plateaus and intervention adaptions are unable to rectify this. This is especially true if a client is starting to reconsider the benefit of maintaining weight loss interventions.
A referral will also offer the opportunity to explore different pathways for weight loss like surgery or prescribed obesity medications. While these topics fall outside the scope of this course, they are options that certain clients may benefit from if previous attempts to diet and exercise have proved ineffective in the long term, or if the health risk of the client is particularly high.
Right, time to apply what you have learned. Head to your assessment for an assessment guide video and instructions on submitting your assessments. This assessment will require you to apply the knowledge you have learned and practised by completing a case study relating to obesity and fat loss strategies.
The assessment guide video explains your assessment task in detail, which requires you to use the information you have learned on this topic to help a case study client.
