Welcome to another week of your programme.
Parts
So far, we have looked at compounding calculations where we are using metric units of measurement such as grams and millilitres. We are now going to look at compounding situations where the units of measurement are ‘parts’.
Consider this question: Calculate the quantities of each ingredient required to prepare 100ml of the final product.
| Cream | |
|---|---|
| Ingredient | Amount |
| LPC Liquid (ml) | 2 parts |
| Salicylic Acid Power (g) | 1 part |
| Cream Base (g) | 5 parts |
How would you go about calculating the answer? Click the heading or '+' symbol below to reveal the method and answer.
- LPC Liquid (ml)
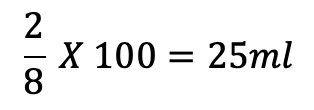
- Salicylic Acid Power (g)
- Cream Base (g)
Answer the following questions for formulations using parts by filling in the gaps in the tables.
International units
Some medications are measured in International Units (IU). The unit measures the medication's action (biological activity), not its weight. This is a more accurate way to measure medications that have large molecules. Examples of medications that are measured in units include:
- insulin
- heparin
- some hormones
- some vaccines
- some vitamins
- penicillin for injection.
Insulin
Insulin is a hormone that the body produces. It helps the body to use sugar (glucose) for energy. In conditions such as diabetes, the body does not produce insulin as it should, and therefore, insulin needs to be provided to the body by injection or via an inhaler.
When prescribing insulin, it is considered best practice for the prescriber to use the brand name and for the medication label to reflect the same. This is a safety measure to reduce the likelihood of medication errors.
Injected insulin may be administered in the following ways:
The majority of insulin preparations are 100 units per ml. Be vigilant - occasionally higher strength preparations may be available. There are always 100 units (U) per ml of insulin. Although most insulins are stable for 30 days at room temperature (<25C), some are stable for up to six weeks. The Pharmacy Procedures Manual specifies that all insulin calculations are based on the premise that insulin expires 30 days after opening.
There are different types of insulin grouped according to their duration and onset of action. A health provider will describe the types of insulin a person requires based on their individual requirements. Therefore you may receive a prescription for a patient with more than one type of insulin ordered. Types of insulin may include:
- rapid-acting insulin
- short-acting insulin
- intermediate-acting insulin
- long-acting insulin
- mixed insulin.
Insulin is a non-stat medication which means it should be dispensed in monthly (30 days) lots.
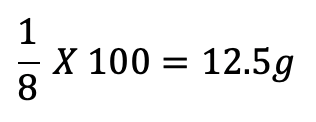
Activity – Help Mr Weston with his insulin prescription
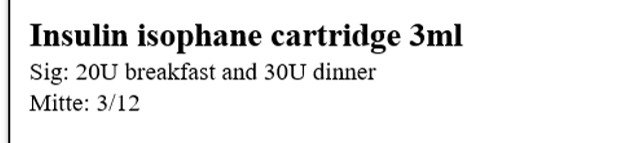
In the prescription below, Mr Weston has been prescribed Insulin neutral, which is a short-acting insulin, and Insulin isophane, which is an intermediate to long-acting insulin.
We will calculate how many of each cartridge should be dispensed to ensure that Mr Weston has enough insulin for the prescribed period.
Open each scenario label to help Mr. Weston get his insulin.
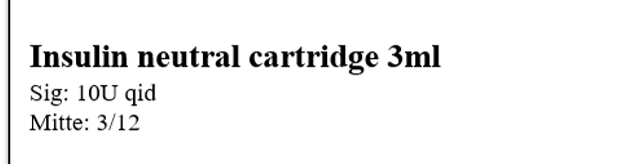
We know that insulin is a non-stat medication, which means we can’t give Mr Weston all 12 of the cartridges at once. We should dispense one month’s supply at a time. To calculate the number of cartridges to dispense each month, we can use the following method:
12 cartridges ÷ by 3 months =
- 4 cartridges for the first month
- 4 cartridges for the second month
- 4 cartridges for the third month
Which we can write as 4 + 4 + 4 or 4OPx3
Apply what you have learnt about the calculations for insulin neutral cartridges:
The next thing we want to know is how much Mr Weston needs for a one-month supply.
Looking at Mr. Weston’s prescription once more, calculate the total number of units of insulin required for one month for each type of insulin. Carry out the calculation before expanding the label to check your answer below.
Did you use the same method or a different method to get to the same result?
- Insulin neutral
10U x qid = 40U for one day
40U x 30 days = 1200U for one month
- Insulin isophane
20U + 30U = 50U for one day
50U x 30 days = 1500U for one month
Self-directed learning activities
To consolidate your learning, complete the following calculations:

A pharmacist helps a customer.
Step 10: Final check
![]()
In this step, the pharmacist is carrying out the final dispensing check on the tasks you have carried out up to this point. When the pharmacist confirms that the prescription is correct and ready for the customer, they will date and sign the pharmacy stamp that shows it has been checked, and initial each item on the script.
Read the following case study:
Pharmacy technician, Sarah, was working in a busy pharmacy that was short-staffed that day. The pharmacy was packed with customers, and Sarah was trying her best to keep up with the demand for prescriptions. One prescription that needed to be filled was for a regular customer who was well-known to the pharmacy. The customer had been on a medication for a long time and knew their medications well. Sarah carefully prepared the medication, checked it against the prescription, and labelled it correctly. Sarah informed the pharmacist that the prescription was ready for the final check. She responded that she would be available in a few minutes.
10 minutes later, she could see the pharmacist was still busy with another task. Sarah felt the pressure mounting as the customer was becoming impatient with the wait, and she knew there was a long line of customers waiting for their prescriptions. In a rush, Sarah decided to bypass the final check with the pharmacist, thinking that she had done everything correctly and that there was no need for an additional check.
Sarah handed the medication to the patient and quickly moved on to the next prescription, hoping to catch up on the backlog of orders. However, a few minutes later, the customer returned to the counter with their medication. She had noticed that the tablets in the container she was given looked different to the ones she normally took. Upon further investigation, it was discovered that the tablets were the correct medicine, but they were 25mg tablets instead of the 50mg tablets that were prescribed.
As you can see, the Final Check is a task that CANNOT be missed under any circumstances.
Step 11: Collection of prescription
![]()
Now that the prescription has had its final check, it is time to hand the customer their completed prescription. This is when you want to be sure that the correct customer receives the correct prescription. In a busy pharmacy, there is the potential that a prescription may be collected by the wrong person. A good way to ensure this doesn’t happen is to do the following:
- Confirm you have the right person by asking the customer for their full name and home address and checking this against the prescription.
- Confirm the medications with the customer. Ask them what medications they are picking up or show them what you have dispensed. They may be able to tell you what medicines they are expecting to collect.
- If it is another person picking up the prescription on the customer’s behalf, confirm by asking the customer’s full name and address.
- Remember, a CD prescription cannot be given to someone other than the patient to collect unless the patient has sent a written authority or the pharmacist knows that the person collecting is an authorised caregiver.
Customer advice
At this stage, you are also going to explain any instructions to the patient and give appropriate advice. You will be using your communication skills to clearly explain the following points about each medication.
- Point out directions
- Where the directions for use are on the label, package, or package inserts.
- Explain the route
- How to take the medicine — this is the route.
- Some medicines, such as eye ointment, might need extra explanations and visual aids, such as pictures, to fully explain how to apply.
- How much to take
- The dose — which will be on the label, but it is good practice to reinforce the written information by repeating it verbally.
- When to take
- This is the frequency or how many times per day. There may be other special instructions such as ‘take with food’ or ‘take at night’.
- Any common side effects
- Any C&A label warnings
- such as ‘do not use after’ date.

Packaging a prescription.
Storage and expiry advice
It is important that you ensure your customers know how to store their medicines at home for the following reasons:
- Maintain the efficacy of medicines
Proper storage of medications is essential to maintain their efficacy.
Medicines can lose their effectiveness when exposed to certain conditions, such as heat, humidity, light, and air. - Ensure safety and prevent harm
Medications can be dangerous and cause harm if they are accidentally ingested. It is important to follow instructions for resealing safety containers and to keep them out of reach of children. - Avoid contamination
Proper storage of medications can also help prevent contamination of the medication. This is important as contamination can alter the chemical composition of the medication and cause adverse reactions in the patient. Therefore, it is important to advise customers to keep their medications in their original packaging and avoid transferring them to other containers.
The instructions for storage may be on the packaging, so draw the customer's attention to this and verbally explain the storage instructions.
You will also be checking if they require any accessories, such as a spacer for an inhaler or measuring devices for suspensions. People may forget that they will need an accurate measuring device until they get home and may be tempted to use a household spoon which is not accurate for measuring medicines.
This is also a useful time to offer accompanying written information, such as a self-care card where appropriate, and let them know who to contact if they have questions or concerns at a later date.
Once you have discussed all of this you should ask if they have any further questions. This may involve looking up information you are unsure of, or referring to other technicians or the pharmacist. Your job is not to know everything but to be able to find out anything.
In summary:
No patient should leave the pharmacy without knowing:
- HOW to use their medicine,
- how MUCH and
- how OFTEN.
At all times, the written instructions should be regarded as a backup to the verbal counselling.
Self-directed learning activities:
Now that we have explored all steps in the dispensing process, let’s take a moment to identify ONE potential risk, error or mistake that may arise at each stage. Then state an effective measure for preventing that issue.
Complete the following worksheet.
Bring your completed table to your next class for a class discussion. After you have discussed, take a look at the issues others have identified and their ideas on measures to prevent them from occurring.

Eyes
Eyes are protected by tears, which moisten them and clean out dirt, dust, and other irritants that get past the defenses of the eyelashes and eyelids. Tears help protect against infection. With each blink, eyelids spread a layer of mucus, oil, and tears over the cornea, which covers the eye. The lacrimal glands in the upper outer corner of each eye socket produce tears, which, after moistening the eyes, flow into canals in the eyelids. These canals drain into the lacrimal sac, a pouch in the lower inner corner of each eye socket. Tears then exit through a passage that leads to the nose.
There are a variety of conditions that can affect the eye, and it is important that pharmacy technicians do a thorough assessment of each patient. This is where your excellent communication skills come in. You will be listening, asking questions, and using the appropriate communication techniques in order to assist the patient. Eye concerns often require the input of a pharmacist. Let’s look at when you should refer.
⚠When to refer to the pharmacist:
- Reports of seeing halos or yellow/green colours when looking at lights
- Deterioration of vision
- Pain in the eyes, light sensitivity, foreign object in the eye
- The cornea (transparent cover over the eye) is cloudy
- Swollen iris (coloured part of the eye), eyeball or tissue around the eye
- Pupils
- Different sizes
- Irregular shape
- Localised redness around the pupil
- Coloured discharge or mucus from the eye
- Eye problem that persists despite treatment or keeps recurring
- Has systemic symptoms like vomiting or headache
- Suspected herpes zoster (shingles) infection indicated by painful rash near eyes
- Contact lens wearer
- Family history of eye problems (glaucoma)
- Taking medications that adversely affect the eye such as amiodarone and others
- Young children, pregnant people, the elderly
- Health conditions that may cause eye problems such as diabetes or immunosuppression
- Have allergies to topical eye products or certain preservatives.
Eye conditions
Let’s start with a scenario to give you practice with diagnosis.
Tama is 55 years old. He approaches you to get some advice about his painful eyes. You ask him to describe his symptoms, and he tells you the following:
“Well, my eyes often feel itchy and irritated. They become a bit red and feel sore, especially towards the end of the day. I also notice a burning sensation and a gritty feeling, as if there's something in my eyes.”
You listen to Tama’s description and wonder if his problem is made worse by something in the environment or by any activities. You ask him to tell you more about his symptoms. He replies:
“Yes, it seems that my symptoms worsen when I spend a long time reading or using the computer. And now that I think about it, the dry feeling becomes more noticeable when I'm in air-conditioned or heated environments, like my office or shopping malls.”
Do you recognise these symptoms?
See if you can work out what Tama’s health condition is before you check the answer by expanding the '+' sign below.
Tama has the symptoms of Dry Eye.
Other symptoms can include:
- Fine crusting on the eyelids
- Stringy discharge from the eye
- Episodes of blurred vision
- Episodes of excess tear flow following dry eye periods
- Heavy eyelids
- Eye fatigue
- If a contact lens wearer then lenses may not sit properly on the eye or feel uncomfortable.
This condition is caused by not enough tears being produced or an imbalance in the components that make up the tears. This means the tears are no longer functioning as a protective film over the eye. People at risk of Dry Eye include:
- People over 65 years of age
- People with hormonal changes such as pregnancy, menopause or taking the oral contraceptive
- Contact lens wearers
- Those using computers
- Those on certain medications or with other eye conditions.
Treatments and advice
Treatment and advice include preventative measures as well as lubricant products to mimic the effect of tears and relieve the symptoms. Examples include Poly-Tears® Lubricating Eye Drops and Systane® Lubricant Eye Gel.
Conjunctivitis – Pokenga whatu
The conjunctiva is a thin clear membrane that lines the inside of the eyelids and covers the white part of the eyes. Its function is to block allergens and pathogens from getting into the eye. It helps to make tears and keeps moisture and lubricants sealed in to protect the eye.
Conjunctivitis is a condition where the conjunctiva becomes inflamed and irritated. It can be caused by various factors, as shown in the graphic.
Treatments and advice
Treatment and advice for conjunctivitis will depend on the underlying cause and may include local treatment of the eye with drops or ointments. It also includes oral medications.
Take a look at the following scenario and answer the related questions:
Jazz is a 32-year-old woman. She is a regular customer. She has partial hearing and reads lips. She comes into the pharmacy looking for antihistamine eye drops for itchy eyes. She thinks she may have seasonal allergies. You take Jazz to a quiet corner so she will be able to hear you better without background shop noise. You face her and ask her to describe her symptoms. She tells you the following:
“Both eyes have been watery and feel sore. You can see this left one is looking a bit pink.”
You can see that the white of the eyeball is indeed pink. You need more information before you can decide what this eye problem is. While Jazz is looking at your face, you ask her if she has noticed any discharge from either eye. She replies:
“Yeah, you can’t see it now, but when I wake up in the morning, my left eye is sticky, like it’s hard to open it, and there are bits of yellow sticky stuff.”
On further questioning, you confirm that Jazz doesn’t presently have, nor recently had a cold, flu, cough, or sore throat. Her eyes sting, and her left eyelid is also slightly swollen.
1. Do you think Jazz has hay fever? If not, what do you think her eye condition is likely to be?
Based on her symptoms, Jazz does not have hay fever; she has bacterial conjunctivitis.
Are antihistamine eye drops an appropriate treatment? If not, why not?
No, antihistamines are not appropriate because her eye condition is not caused by an allergy.
As a pharmacy technician, what treatment and advice would you provide?
You would advise Jazz that based on her symptoms, you will refer her to the pharmacist.
What is the likely treatment and advice for this condition?
Go to this page on the Healthify website to find out the appropriate treatment and advice. In your notes, describe what treatment and advice you would give Jazz.
Skin
In your level 3 programme, you looked at the skin and the following skin conditions:
- Wounds
- Blisters
- Burns
- Cancer
- Eczema.
Here is a reminder of the different layers of the skin.
We are now going to look at two other skin conditions:
- Fungal infections
- Acne
Fungal Infections of the Skin
There are three main groups of fungi:
- Yeasts
- Moulds
- Dermatophytes.
⚠When to refer to the pharmacist:
If a customer has a fungal infection and the following are present, refer to the pharmacist:
- Fungal infections inside the mouth
- The area involved is large, or multiple toenails are infected
- Signs of bacterial infection- oozing, crusting, swelling
- The skin is broken or bleeding
- The condition persisted or reoccurs despite treatment
- Other symptoms- flu-like, increased thirst or urination
- Suspected vaginal infection
- Young children
- People with diabetes, circulatory problems
- Immunosuppressed or pregnant
- Allergies to topical medicines.
Dermatophytes are the main group of fungi to cause infection. They cause the following infections:
- Ringworm of the scalp -Tinea capitis
- Ringworm of the body- Tina corporis
- Jock itch -Tinea cruris
- Athletes foot -Tinea pedis
- Fungal nail infections -Tinea unguium.
Look at the picture below. See if you can identify the fungal infection and then select the label to see if you are right.

Ringworm of the body – Tina corporis
As you can see, this type of infection is a circular, red rash with raised edges. There is usually a patch of clear skin in the middle of the circle. The patient will indicate that the rash is itchy and you can see that it looks scaly and cracked.
Treatments and advice
Treatment and advice will depend on the type of fungal infection and where is it on the body. Antifungal creams, powders, or other dose forms may be prescribed or purchased over the counter. Advice will also include how to prevent the spread of the infection as well as how to prevent an infection occurring.
Acne – Mate hunahua
Acne is a common skin disease that causes pimples. Pimples form when hair follicles under your skin clog up. Most pimples form on the face, neck, back, chest, and shoulders. Anyone can get acne, but it is common in teenagers and young adults. It is not serious, but it can cause scars.
No one knows exactly what causes acne. Hormone changes, such as those during the teenage years and pregnancy, probably play a role. There are many myths about what causes acne. Chocolate and greasy foods are often blamed, but there is little evidence that foods have much effect on acne in most people. Another common myth is that dirty skin causes acne; however, blackheads and pimples are not caused by dirt. Stress doesn't cause acne, but stress can make it worse.

⚠When to refer to the pharmacist:
- If the customer is under 12 or over 30
- If the acne is extensive, moderately severe, or severe
- Previous acne treatments used for at least 3 months have not been successful
- If the skin does not have the typical features of acne - it could look similar but be another condition
- The customer is unable to avoid exposure to the things that make the acne worse
- Women with excessive facial hair, irregular periods, or prone to weight gain
- Taking medicines or supplements that are known to make acne worse
- Sensitive skin or allergies to topical products
- Other health conditions, immunosuppressed, pregnant or breastfeeding.
Carry out your own search for information on the following and record your findings.
Treatment and advice for acne
- OTC products for the treatment of acne (name one & how to use it).
- OTC skin care products for maintaining healthy skin (name one & how to use it).
- Advice for ongoing care and management of acne (name one piece of lifestyle advice).
Self-directed learning activities
To complete these activities, you will need to create a document with your responses to the questions and research.
EYES
- Find out what each of these eye conditions are and write a 1-2 sentence definition:
- Presbyopia
- Myopia
- Hyperopia.
- Read the following interaction between a customer and a pharmacy technician.
Customer: Hi, I'm having some trouble with my eyesight lately, especially when I try to do needlework in the evenings. It's becoming difficult for me to see clearly.
PT: I'm sorry to hear that. Let's see if we can figure out what might be causing this issue. First, may I ask your age?
Customer: I'm 58 years old.
PT: Have you experienced any other symptoms besides difficulty seeing clearly during your needlework? Any discharge from your eyes, pain, or swelling?
Customer: No, not really. It's mainly when I'm focusing on fine details or doing close work.
PT: Ok, looking at your eyes now, I don’t notice anything unusual, has the appearance of your eyes changed at all?
Customer: Nope, nothing like that. I’ve not been sick, and I don’t have headaches. I wonder if it’s just old age? I do tend to have trouble reading the directions on those heat and eat meals I get from the supermarket. - Which of the three eye conditions do you think this customer has — record your answer.
- You inform the customer what you think their eye condition is and that they should get their eyes checked. The customer replies:
Ok, I’ll book an appointment. In the meantime, is there anything I can get from you to improve my vision for doing my needlework?
What does the pharmacy stock that this customer could use?
SKIN
Jono is 26 years old. He has just been to the doctor for itchy spots around his ankles. The doctor has told him they are insect bites. He can take a systemic treatment such as an oral antihistamine or use an OTC topical cream. He has decided he wants to use a topical cream.
Identify one OTC cream he could use. List the following information:
- Name of the cream (trade or generic).
- The purpose of the cream.
- The directions for use.
