Homeostasis means regulation. Our body has many clever and complex ways to make sure that the systems are working in the most ideal environment possible. This means that it must adapt to changes in the external environment, such as hot or cold weather, and to changes inside the body, such as low blood sugar levels.
The body must regulate many different factors. When homeostasis cannot be achieved effectively, many organs or systems may be affected, and the person will become unwell. If the body is unable to achieve homeostasis, especially over a long period, the person can become very unwell and can die.
By the end of this chapter, you will understand:
- How the body achieves homeostasis
- The support that you can give to the person to keep these functions and processes healthy.
Example
Homeostasis must be maintained in many different functions and conditions. These include keeping the body stable in relation to:
- Temperature
- Fluids and electrolytes
- Wastes and toxins
- Disease causing organisms
- Delivery of oxygen to the cells
- Heart rate
- Fat deposits
People, like other organisms, need to have a consistent body temperature for our systems to function properly. If our temperature becomes too high or too low, our organs, cells and tissues cannot function effectively. If extremes of body temperature continue, the result to the body can be fatal.
The process that keep our temperature within a normal range is called thermoregulation. When we are exposed to heat and cold, thermoregulation keeps our internal body (core) temperature constant.
Note
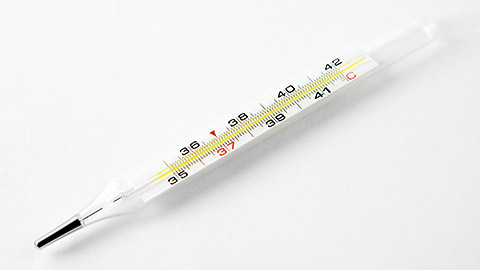
A normal temperature range is between 37°C and 37.8°C.
| Hypothermia | A core temperature that is too low and can lead to brain damage, heart attack and eventually death. |
Factors that lower body temperature includes:
|
|---|---|---|
| Hyperthermia | A core temperature that is too high and can lead to brain damage and death. |
Factors that can raise body temperature include:
|
Thermoregulation is controlled in the hypothalamus which is a gland of the brain. When the core temperature of the body becomes too high or too low, the hypothalamus sends messages to organs such as muscles, glands, skin and blood vessels and to the nervous system.
Together these organs and systems work together to return the core temperature to normal.
These processes include:
Maintaining Body Temperature
Older people can have more trouble regulating their body temperature than younger people.
Sensible clothing and bedding helps the person to retain heat in cold weather. Remember that people who have less hair, such as baldness, can cause heat loss through the head, so help the person to wear a warm beanie or other head coverings to prevent this.
When the temperature is over 30°C, you can support them to regulate temperature using some or all of the following:
- Encourage them to stay indoors and out of direct sun
- Help the person to drink plenty of fluids
-
Reduce tea, coffee and alcohol intake in hot weather so that the person does not lose too much fluid through the diuretic action of these fluids
- Report any signs of dehydration, such as headaches and dark coloured urine
- Suggesting a visit to an air-conditioned place such as a shopping centre can help in extreme heat if the person lives in their own home but does not have air conditioning
Watch
Take a look at this video that provides a good discussion about Homeostasis.
Activity
You are working with Mary, she is 76 years of age and has not been feeling well the past few days and when you check her temperature it is 39.6°C. What questions might you ask Mary to assess her health based on this heightened temperature.

We need fluids and electrolytes to function and stay alive and well. Adults are made up of around 60 per cent water. If this level drops, we can become seriously unwell.
Electrolytes take on a positive or negative electrical charge when they are in bodily fluid such as blood. We need these charges to help send messages and create vital chemical reactions such as growth and movement.
We take electrolytes through our diet. Some examples are:
- Salt
- Potassium
- Magnesium
- Calcium
- Chloride
Maintaining Fluids
Fluid is contained inside our cells (about 40%) and outside our cells (about 60%). We need to have the correct percentages on both sides of the cell walls, in our blood cells and in the blood, in our tissues and in our lymph and in our muscle cells and in the spaces around them.
Fluid Balance Charts
A fluid balance chart helps to measure the amount of fluid that is taken in and excreted out of the body over a 24-hour period. The amount of fluid taken in and excreted out in one day should be roughly the same. Measuring the persons fluid intake (what they drink) and comparing it to their urine or other liquid output (urine, diarrhoea or vomit) can help medical staff to identify problems.
Read more to see an example of a completed Fluid Balance Chart.
This person’s fluid balance over 24 hours is roughly equal. If there were major differences in this balance, however, it might alert nurses and doctors to problems such as the following:
- The person might be dehydrated
- The person’s medications might be causing them to produce too much urine and require a review
- They might have a problem with emptying their bladder fully
- They might have a problem with producing urine in the kidneys (kidney failure)
- They might have a condition causing them to retain too much fluid, such as a heart condition
- They might be at risk of breathing problems, high blood pressure and a condition called oedema from not being able to remove enough fluid
Electrolytes
Electrolytes help to keep fluids balanced. If our electrolyte balance is too high or too low, fluid moves between the cells and the spaces around it, changing the balance and creating serious problems like dehydration or high blood pressure.
Some of the major electrolytes needed by our bodies include:
Sodium (salt)
- Maintains blood pressure
- Controls fluid
Potassium
- Regulates the heart and blood pressure
- Helps transmit nerve impulses
- Muscle contraction
Magnesium
- Nerve and muscle function
- Helps maintain heart rhythm
- Helps regulate blood glucose levels
- Supports the immune system
Calcium
- Strengthens bones and teeth
- Nerve impulses and muscle movement
Chloride
- Balances electrolytes
- Maintains a healthy pH
- Essential to disgestion
Electrolyte Imbalance
Electrolyte imbalance can be caused by:
- Exercise and excessive sweating
- Vomiting and diarrhea
- Dehydration
- Eating disorders and malnutrition
- Some medications
- Excessive alcohol intake
- Heart or kidney disease
- Diabetes
- Severe burns
You can help to prevent electrolyte imbalance by providing the following support:
- Help clients to eat a well-balanced diet with plenty of fluids, fruits, and vegetables
- Encourage clients to drink more fluid in hot weather
- Report nausea and vomiting and encourage the person to drink small sips of fluid
- Carefully follow fluid restrictions that have been ordered by the resident’s or client’s doctor
Dehydration
Older people are at higher risk of dehydration, particularly in hot weather. People can also become dehydrated if they have been vomiting or have diarrhea, or if they are frail and unable to help themselves to fluids.
Symptoms of dehydration include:
- Feeling thirsty
- Feeling dizzy or tired
- Dry mouth
- Dry lips
- Sunken eyes
- Dark coloured urine with a strong smell
- Passing small amounts of urine
- Not passing urine very often
It is important to encourage residents and clients to drink fluids throughout the day.
Here are some tips to help people at risk of dehydration to drink more fluid:
- Offer small sips frequently, rather than a large drink every now and then
- Fluid does not have to be in liquid form. Frozen or thick desserts such as ice cream, icy-poles custard, milkshakes, jelly, soft lollies such as jubes, sauces, and pureed food all contribute to fluid intake
- Offer the drinks the person prefers. If they do not like water, try milk or cordials. Tea and coffee contribute to fluid intake but they should not be the only source of fluid
Dehydration can be especially dangerous in frail older people and small children. Report any signs of dehydration as soon as you see them.
Watch
Watch this short video that provides some great information about Electrolytes and why they are so important!
Check your knowledge
What is pH and why is it important?
pH stands for the Potential of hydrogen. It is important for us to maintain a healthy pH ratio as bad bacteria thrive in an over-acidic environment.
pH Balance
pH balance is also called acid-base balance. It refers to the acid content of your blood. The body functions best with a blood pH level of around 7.4.
The lungs and kidneys help to maintain this balance. If the lungs or kidneys are not working correctly, the pH level can become too high (acidosis) or too low (alkalosis). These are dangerous conditions.
Respiratory acidosis occurs when a disease or condition in the lungs or respiratory system means that the lungs cannot remove enough carbon dioxide.
Metabolic acidosis occurs when the kidneys cannot control the acid levels. This can be the result of kidney disease, severe vomiting or diarrhoea, diabetes, alcoholism or an overdose of certain medications.
Maintaining pH Balance
Older people and people with certain diseases such as diabetes can be more prone to pH imbalance. This can be dangerous.
Some ways that you can help the person maintain a healthy pH balance include:
- Help them to maintain a healthy weight
- Encourage them to reduce smoking and alcohol intake
- Take all care to avoid medication errors if you assist with medications
- Check the person’s urine pH level regularly when ordered, especially if they have diabetes, and report any changes in urine pH
- Help the person to eat a healthy diet and have adequate fluids
- Report changes in the person’s condition, especially nausea and vomiting
- Follow instructions from the person’s doctor if they are diabetic, and report immediately if they have skipped a meal
- Give the person extra fluid in hot weather or when they have been vomiting or have diarrhea.
Watch
The following video discusses the pH scale and its importance.
Wastes are removed mainly by our digestive system, as faeces, and by our urinary system as urine. People who are older are especially at risk of having difficulties with their bowel and bladder function. Other people, such as those with spinal cord injuries, might also need support to maintain healthy bowel and bladder habits.
Urinary System Health
Our kidneys must excrete at least 30ml’s of fluid per hour to stay healthy. Most people empty their bladder four to eight times every day (every three to four hours). As we age, the muscles that help us to control our bladder become weaker. This can lead to incontinence or loss of control of the flow of urine. It can also lead to incomplete emptying, which in turn increases the chance of infection.
Keeping the urinary system healthy helps it to stay efficient at excreting waste.
Some ways that you can support the client to do this include:
- Help them to drink at least six to eight glasses of water or other fluid a day
- Teach them and encourage them to exercise their pelvic floor muscles
- Maintain exceptional hygiene when attending to personal care to help avoid urinary tract infections
- Report any signs of infection, such as odour or burning pain when urinating
- Report highly concentrated urine that is dark in colour
- If the person has an indwelling catheter, report to a supervisor immediately if their urine output is less than 30ml’s per hour
If the person does not have a catheter, report an unusually low urine output over 24 hours
Fluid Retention
Some conditions, including ageing, can cause the body to become less effective at eliminating excess water and other wastes via the urine. If the kidneys are not functioning well, the person might have too much fluid and other waste products in their body. This might lead to what is called fluid overload or fluid retention.
Here are some signs to look for:
- Swollen feet, ankles, legs and hands: The fluid can become trapped
- Quick weight gain: The fluid is heavy
- Pitting Oedema: The skin stays indented for a few seconds if it is pressed. This is where the capillaries are full of fluid.
Watch
Take a look at this YouTube video by Vivo Phys – Evan Matthews about pitting oedema:
Some people who have fluid overload will be placed on a fluid restriction by their doctor. This means that the person should drink no more than their maximum fluid allowance every 24 hours.
Example
You might see a sign on the person’s file that says:
Fluid restriction 1500ml
This means that the person should not drink more than this amount of fluid in a day.
Remember that some foods such as jelly or custard can also count towards this amount.
Eliminating Wastes from the Digestive System
A healthy bowel produces soft, well-formed bowel actions (faeces) on a regular basis, such as every day.
Constipation

As people become older, the smooth muscles that push the faeces through the bowel without our conscious control slow down and become slower and weaker. This makes the person more prone to constipation because the faeces stays in the bowel for a longer time while water is being absorbed as it travels down the intestine.
Other conditions, such as spinal injuries and multiple sclerosis can also make it more difficult for the person’s body to move faeces through the bowel.
Constipation results in hard stool that have spent too much time in the bowel. They cause the person to strain, which can lead to problems like haemorrhoids and it can also make the person very unwell. Severe constipation can lead to serious problems like bowel blockages.
The Signs of Constipation
A person with constipation might show the following signs:
- Not opening their bowels very often
- Passing hard, small faeces
- Straining to pass faeces
- Abdominal pain
- Bloating in the abdomen
- Abdominal cramps
Preventing Constipation
Fibre is important to help reduce constipation, which can be a major problem for many older people and people with physical disabilities. Vegetables, grains and fruits are all excellent sources of fibre. Prunes, liquorice and fibre supplements stirred into a drink are great ways to boost fibre.
You can support good bowel health and prevent constipation by encouraging the person to:
- Drinking at least six-eight glasses of water per day
- Exercising regularly
- Eating high-fibre foods such as grains, fruits and vegetables
Recording Bowel Motions
Most aged care facilities require staff to document daily bowel motions on a chart. This helps nursing staff to be alert for signs that the person might be constipated or at risk of infection and dehydration due to diarrhoea.
The bowel actions are usually charted using standard Roman symbols like this:
| Date | Monday 1/3 |
Tuesday 2/3 |
Wednesday 4/3 |
Thursday 5/3 |
Friday 6/3 |
Saturday 7/3 |
Sunday 8/3 |
|---|---|---|---|---|---|---|---|
| Bowel motions | i | iii (Loose, watery) |
õ | ii | i | õ | õ |
If the person has not used their bowels for two or more days, as on Saturday and Sunday above, report this to your supervisor or nurse.
If the person has several bowel actions in one day, particularly if they are loose or watery, such as on Tuesday above, report this to your supervisor.
The Bristol Stool Chart

Separate hard lumps

Lumpy and sausage-like

Sausage share with cracks
Like a smooth soft sausage or snake

Soft blobs with clear-cut edges
Mushy consistency with ragged edges
Liquid consistency with no solid pieces
The Bristol Stool Chart is a commonly used chart to help you to document the consistency of the person’s stool (faeces). You might be asked to use the chart to help you document the person’s bowel motions.

Blood pressure is the measure of force that the blood exerts on the walls of the arteries as it is pumped around the body.
Measuring Blood Pressure
Blood pressure readings are taken with an instrument called a sphygmomanometer or blood pressure machine.
A blood pressure reading produces two measurements.
- Normal systolic pressure is usually between 110 and 130mmHg. The systolic reading is the highest reading.
- Normal diastolic pressure is usually between 70 and 80mmHg. The diastolic reading is the lower reading.
The final reading is represented with the systolic reading written over the diastolic number. You might be asked to record blood pressure readings on a chart, like this:
Read more to see the final reading of the blood pressure results.
This person’s blood pressure readings are not regular. The high readings on Wednesday, Friday and Saturday should be reported to your supervisor.
Watch
Watch the following YouTube video by RegisteredNurseRN called Blood Pressure Measurement: How to Check Blood Pressure Manually to see how to take a manual blood pressure reading:
High Blood Pressure
High blood pressure is called hypertension. It means that there is too much force from the blood on the arteries.
High blood pressure can be caused by:
- Arteries that are clogged with fatty deposits or cholesterol (atherosclerosis)
- Smoking
- Ageing
- Stress
- Heart disease
- Kidney disease or fluid retention
- Too much salt and fat in the diet
- Obesity
- Certain medications
Most people have a raised blood pressure shortly after exercise, or when they are in pain or stressed. A continuously high blood pressure, however, can have serious effects such as stroke and heart attack.
Low Blood Pressure
Low blood pressure is called hypotension. It means that there is not enough force on the arteries. This can be caused by dehydration, heart problems and certain medications. Postural hypotension happens when a person’s blood pressure drops quickly when they stand or sit up after lying down, such as first thing in the morning. This causes the person to feel dizzy and could cause them to faint or fall. This is more common in older people and people with spinal cord injuries. Help to reduce the effects of postural hypotension by encouraging the person to sit on the side of the bed for a few minutes before standing.
Maintaining a Healthy Blood Pressure
There are many ways to help residents and clients lower their blood pressure. Their GP might order them medications to keep their blood pressure and cholesterol levels down.
Your role can include:
- Encouraging a healthy diet
- Supporting the person to maintain their health
- Supporting the person to reduce unhealthy habits
Watch
Watch this YouTube video from the Heart Foundation titled Keep your blood pressure down about how to support a healthy blood pressure:
Activity
The Healthy Eating Pyramid
Read The Healthy Eating Pyramid article.
Note the types and proportions of food that we should eat daily to maintain a healthy body. Consider the following questions:
Q1. How does your diet compare to that of the recommended types and proportions of food?
Q2. How does the calorie intake for a seventy-year-old person differ from that of a sixteen-year-old?
Heart Health
Complete the quiz at the Australian Heart Foundation’s website.
Q1. How healthy is your heart according to the calculator?
Q2. What could you do to improve your own heart health?
Some infections can be especially common, and dangerous, in residential settings where a number of people live and work together. They can be easily spread through performing close tasks like personal care. Older people and people with disabilities, especially those with chronic health conditions, can have lower immunity and can catch some infections more easily. Some infections can be more dangerous in these people, too.
Common infections include:
- Gastroenteritis
- Colds and flu
- Conjunctivitis
- Scabies
- MRSA
Practicing Good Hygiene

Standard precautions include three things that you must do every time you provide close support or personal care to a client or resident, no matter who they are or what you know about them. They are the three most important things you can do to protect yourself and others from many different types of infection including hepatitis, staph infections, conjunctivitis and fungal infections.
Here are the three standard precautions:
- Wash your hands before and after close contact
- Wear gloves when you are potentially in contact with the person's body fluids
- Dispose of body fluids in the correct water receptacle
Clean hands are particularly important because we use our hands in most tasks for supporting clients with physical and personal care activities.
Additional Precautions
Additional precautions are used when there is a known infectious or contagious condition that cannot be contained by standard precautions alone. For example, when a client or resident has gastro enteritis, scabies or the flu.
Additional precautions do not replace standard precautions. They are used as well as standard precautions. They can include wearing gloves more frequently, wearing a mask, gown, shoe and hair protection and isolating the person from others.
Example
Keep surfaces of equipment such as shower chairs and hoists clean by wiping them with disinfectant after each use. This is especially important if the equipment is shared between residents.
Supporting Hygiene Routines
Bacteria and moisture left on the skin for long periods can lead to infections, disease and pressure sores. Supporting the person’s personal care needs and hygiene are important in helping protect the person from infection.
Good hygiene includes:
- Reminding the person to wash their hands before eating, after toileting and before entering public areas of a facility
- Showering, bathing or washing to remove dirt, bacteria, urine, faeces and sweat from the person’s skin
- Helping the person to care for their mouth and teeth, to remove food and bacteria, and prevent ulcers, gum disease and tooth loss
- Supporting the person with continence aids if they are required
Oral Health
Dental diseases and infections are almost entirely preventable with good daily oral care.
Good oral care includes:
- Helping the person to clean their teeth and dentures after each meal
- Checks of the person’s mouth and gums regularly for signs of cuts, pain or infection
- Caring for the tongue, lips and gums
- Supporting the person to have regular check-ups with a dentist
- Keeping the mouth and lips moist by making sure they have a good fluid intake
- Reporting pain or ulcers
Nutrition

A good diet can help to increase the person’s immunity and also provide them with a better ability to fight off infections if the person does contract them.
Older people can need more protein, calcium and vitamin D than many younger people.
Note
Australian Dietary Guidelines recommend minimum quantities of certain foods.
These recommendations include:
- 2 1/2 servings of meat, chicken, fish or eggs every day
- 3 to 4 servings of calcium rich foods (such as milk, cheese, yoghurt or ice cream) per day
- 3-4 servings of breads, cereals, rice and noodles per day
- 2 servings of fresh, frozen, canned or dried fruit each day
- 5 servings of vegetables, nuts or seeds each day
Being underweight is much more of a problem in aged care than overweight. In disability services, however, inability to exercise can make younger people prone to being overweight.
Residents in aged care must be weighed at least monthly, and you must report any unplanned weight loss or slow wound healing. A doctor or dietician can help to assess the reasons for the weight loss and help the person to gain healthy weight.
Example
Nutrients that support healthy teeth and gums include Vitamin C and calcium. Dairy foods are the best source of calcium.
Note
It is just as important to attend to oral hygiene for people with dentures as it is for people with their own teeth. Dentures should be cleaned twice a day and be cleaned professionally on a regular basis. All dentures in an aged care facility should be marked with the person’s name. This is usually done with engraving.
Example
In aged care and in disability, regular checks of the older person’s mouth and skin can help to find infections early.
Check regularly for:
- Pain in mouth or gums
- Gums that are moist and pink, and not bleeding
- Sores, redness or ulcers on the skin
- Signs of dryness or flaky skin
- Moist lips and mouth
Document and report any problems that you notice or that the person reports to you.
Reporting Physical Condition Changes
No one expects you to understand the full range of diseases or conditions that might affect the people you support. It is, however, important that you are able to look for and report changes in health and well-being that might mean that the person is unwell, or that they need additional help or referral to a professional such as a GP.
Signs that a person might be experiencing illness or that they are at risk of poor health include:
- Pain or discomfort, especially if it is ongoing
- Sudden signs of confusion
- A high temperature, or feeling hot and sweaty for no good reason
- Nausea and vomiting
- Dizziness or weakness
- Rashes, redness or other skin problems
- Pale or flushed skin
- Changes in the person’s physical abilities
- Withdrawal or depression
Your service will have a system for reporting these and other signs of illness. If you have concerns, report them as soon as possible, because some signs and symptoms can deteriorate quickly or can be indications of a serious health problem. In community settings, this will often be via a phone call to your supervisor. In a facility, this will usually be to the supervisor or nurse in charge.
You will also need to document the person’s signs and symptoms carefully. Documentation helps to support your verbal report and can help to ensure that the information is passed on correctly to others such as health professionals. Documentation in community settings will often be via a form called a monitoring form or an incident and illness report. In an aged care facility, it will be via a file note in the resident’s file.
Regular physical activity helps nearly every organ and system of the human body, including the muscles and brain, to function better.
Physical activity can:
- Help the person to maintain a healthy weight and reduce fat around the body’s organs such as the heart and blood vessels
- Reduce high blood pressure
- Pump blood more effectively around the body and into the tissues, providing energy to our cells and to our brain
- Work muscles and other structures to keep them strong, supple and efficient and to reduce the chance of falls
- Strengthen bones and reduce osteoporosis and fractures
- Help lift mood
- Provide the person with a purpose and an enjoyable pastime, such as sport or games
- Increase the person’s lung function and support breathing
- Increase appetite
Active Exercise
Active exercise means that the person moves their own limbs or body to exercise them.
Exercise does not have to mean high impact or energetic workouts. If the person has a physical disability, an illness or if they are frail, a physiotherapist or occupational therapist can help them to tailor exercise to suit their needs and abilities.
Example
The person can exercise in a chair or wheelchair, using their legs and arms if they can.
Ball games can be adapted to use a balloon instead of a ball, giving a safer and gentler form of exercise.
Walking is a very beneficial exercise for everyone. The more the person walks, the less chance they have of injury from falls.
Weight bearing exercises can improve bone strength and reduce the effects of osteoporosis. Weightbearing can still be done in a chair or wheelchair. Ask the person to push down with their feet onto the plates of the wheelchair or onto your hands while they are sitting. Ask them to push against your hands with their hands. This can help strengthen both the muscles and bones, even if the person does not stand up.
More complex weight bearing and weight training exercises can be designed by a physiotherapist to help the person maintain strong and healthy bones and muscles.
Cardio exercise increases the strength and resistance of the heart and lungs. A good rule of thumb for a healthy person is to try to help the person to reach a heart rate of 70 percent of their maximum heart rate (220 minus their age). If a person you support is aged 50, with a disability but otherwise healthy:
220 minus 50 = 170
70 percent of 140 = 119
So, cardiac exercise that achieves good heart exercise increases the person’s pulse to 119.
(Always remember to check with the GP or physio if you are helping an older person or a person with chronic health conditions to exercise.)
Older people and people with health conditions are likely to benefit more from low-intensity cardio exercise.
Water Exercise

Swimming and aqua aerobics can benefit many people because it is easy on joints and muscles. Your local recreation centre is likely to have programs that suit different age groups and abilities, including programs for older people. People with arthritis can benefit from moving their joints in warm water. Many centres also have disabled access to pools via hoist or water chairs.
Exercise Program Support
Older people should speak to their GP about any new exercise program to ensure that they can do so safely and without risk to their health.
Help the person to choose activities that interest them. For example, they might prefer dancing to swimming. They are more likely to stick to a program that is fun and enjoyable, and that they can do with people with similar interests and abilities.
Try to make exercise a social event. For example, exercise in small groups or arrange for a coffee or chat after the activity.
Help the person celebrate improvements by charting weight gain, noticing and commenting on fitness or other improvements. This can help motivate the person to keep going.
Use technology such as watches that measure pulse and that track fitness. These can be an excellent way to track progress.
Help the person to dress in clothing and shoes that maximise movement and safety. Have a water bottle nearby and encourage them to drink plenty of fluids.
Consider any sensory losses, such as hearing or vision loss, and keep the exercise environment safe to reduce the chance of injury.
Read
You will find more information and suggestions in the Australian government’s physical activity guide for older Australians called Choose Health: Be Active
Resource
A pre-exercise screening tool can help a person who is older or who has chronic illness to determine their risk level. They can use the tool by themselves or with their doctor. You might help the person to complete the tool so that they can take it with them to an exercise professional, exercise classes or to their GP or physio. Download copy of the pre-exercise screening tool.
Passive Exercise
Passive exercise means that other people move the person’s limbs for them. This can be beneficial to people who are frail and people who have paralysis of all or part of their body, such as after a stroke or spinal cord injury.
If a person is not able to move their limbs, the muscles slowly contract and shorten. This can become permanent and result in contractures. Contractures happen when the limb, fingers or toes have curled up and are unable to be straightened. Contractures are painful and can cause other medical and health problems including infections.
Passive exercise is important for people who cannot move their limbs to help prevent contractures. The exercises usually involve gently moving the limb, fingers or another body part into a straight and then bent position several times a day. A passive exercise program is usually designed by a physiotherapist.
Website
Learn more about passive exercise.
Activity - Research
Questions:
- Can you explain the difference between active and passive exercises?
- Describe three (3) of each type of exercise.
- What issues may develop from a lack of exercise? Particularly for an individual that spends a lot of time seated or in bed.
Use the following questions to check your knowledge.
- Outline the meaning of homeostasis.
- Give two examples of how the body can increase the core temperature if a person becomes cold.
- List three signs of dehydration.
- Give two examples of how you can help a person maintain a healthy blood pressure.
- Explain the difference between active and passive exercise.

