In this section you will learn to:
- Identify the legal and ethical responsibilities of a health worker
- Identify and discusses child safe practices and requirements within the workplace, including mandatory reporting
- Identify legal and ethical responsibilities when responding to and reporting a breach
- Complete electronic and written workplace documentation
- Follow organisational policies and procedure for using digital media
Supplementary materials relevant to this section:
- Reading F: Digital Health Policy Templates for allied health practices

In the previous unit, you would have been provided with a thorough understanding of the legal and ethical responsibilities of a health worker. In this section, we will touch on some of the same concepts, legislations, and rights with emphasis on referring and reporting any breaches or issues.
Competent Service and Roles/Responsibilities
It is important for health workers to meet mandatory requirements qualification requirements, follow relevant practice standards, and work within their scope of practice. Scope of practice refers to the work-role boundaries and responsibilities expected of you as a health worker. Day-to-day duties of a health worker can vary depending on the allied health practice you’re working for. The core responsibilities of a health worker refer to respecting the client’s rights, privacy and confidentiality, safety and well-being, and with delivering competent service. But can include other duties depending on the specific allied health organisation you end up working for.
Regarding specific tasks related to your role, we are going to revisit the advice from MAT (n.d.) provided in a previous unit, Work Legally and Ethically, whereby if a health worker is unsure what their role entails or needs advice regarding work instructions that they should seek advice from colleagues; clarify their position description, scope of practice, and any relevant policies and procedures; ask for a performance review; and/or consider seeking regular support and supervision and inform team leader of any situations. Due to the nature of allied health industry, it is vital that health workers keep on top of professional development, which will be explored in more detail in the module.
Informed Consent
Informed consent must be obtained from the person seeking help before commencing with care in order to respect client autonomy. This involves both providing the client with all of the information relevant to the treatment or options of care, and that they consent without coercion. Information relevant to treatment and options may involve the nature, purpose, risks, and benefits of any proposed treatment. Clients have the right to decline treatment once the risks and benefits have been made available to them.
Translation Services
Clients have a right to access an interpreter if they need one and should be informed of this when accessing health care. Interpretation services should be provided by a certified interpreter and should be free and confidential for the client. According to the Guide for Clinicians Working with Interpreters in Healthcare Settings by Cultural Diversity Health (2019) “clinicians should not engage minors and not rely on family members, intimate partners, friends, and web-based translation applications to facilitate interpretation.” Allied health professionals should ensure that the need for an interpreter is clearly documented including specifics regarding the client’s preferred language, and/or gender of interpreter. When assessing whether a client may require an interpreter, it is important to err on the side of caution. Cultural Diversity Health (2019) says the following regarding assessments for an interpreter: “people may have gaps in confidence and competence between receptive English (understanding what a clinician says) and expressive English (being able to ask questions in English).” People who may need interpreters include those who speak a language other than English, those who are Deaf, and/or people who may suffer from mental or other language barriers that may inhibit their capacity to discuss and understand health related matters. It is also important to note that, while an interpreter may assist with removing a communication barrier, the responsibility for establishing that the client comprehends what is being said remains with the allied health professional/worker.
Tip
Find Out More
The Guide for Clinicians Working with Interpreters in Healthcare Settings offers a framework for effective communication when working with interpreters and clients. It is a very useful resource for future health workers and includes additional resources for interpreting services and a comprehensive glossary.
Mandatory Reporting and Child Protection
Australian legislation, the Child Protection Act 1999, mandates sharing otherwise confidential information in limited circumstances, such as cases where child abuse is suspected or confirmed. This applies even when the child is not the client, and in case of adult disclosure of abuse when they were a child. It also applied for vulnerable individuals such as elderly, and people with disabilities. While mandatory reporting legislation does differ between jurisdictions, a child’s right to safety is considered paramount in all states and territories, and health workers have a legal and ethical obligation to act where they have reason to believe a child has been abused, is being abused, or is at risk of abuse. Health worker should understand the mandatory reporting pertaining to their state and territories. There are penalties for nondisclosure where a mandatory reporter has reason to suspect abuse but fails to report this information. It is important to consider indicators of risk in these scenarios also. Indicators could be previous abuse or neglect of a sibling, a family history of violence, or the ability of the parent to care for the child in their care).
| Mandatory Reporters within Australia | What must be reported |
|---|---|
|
|
Find Out More
Privacy and Confidentiality
Health workers have a responsibility to ensure their client’s information is kept confidential. The client’s identify, any detailing pertaining to their treatment or other helping service, and all notes and points of discussion between a health worker/allied health professional and their client should be kept confidential and stored in a private and secure manner. Clients should be made aware how their privacy is being protected from unauthorised access. This might include how their electronic data and information are stored and backed up, and what security measures are used, such as password protection and data encryption.
Case study
Martina is a health worker who has been provided written consent from the Cooper family for documents to be sent from another allied health professional who is working in collaboration with the organisation Martina works at. When receiving the email response from the allied health professional, Martina notices she has received documents for a different family, with their personal information in the document. What should Martina do?
- Inform the allied health professional of the breach in confidentiality
- Delete the email
- Inform supervisor
Boundaries
Health workers have an ethical responsibility to maintain appropriate professional boundaries and avoid any client exploitation. There are a range of behaviours that have the potential to blur the professional boundaries of the practitioner relationship. These are often thought of as ethical dilemmas and, though they are more likely to occur in professions such as counselling, are still important dilemmas to consider for any helping profession. These can include engaging with a client socially outside of the workplace or accepting gifts from clients.
Responsibility of the health worker
As a health worker, there are several legal and ethical legislations that are pertinent to your role. These legislations are protections for clients, and they operate under a rights-based approach. That is, an approach based on “international human rights standards and operationally directed to promoting and protecting human rights” (United Nations Sustainable Development Group, 2023). Within these, and in addition to the above ethical and legal considerations, there is the United Nations Declaration of Human Rights and anti-discrimination legislation. As mentioned previously, health workers also have a duty of care towards clients, which means they have a responsibility to take reasonable steps to avoid clients coming to harm either through their actions or lack of actions. Failure to fulfil duty of care can result in legal liability, disciplinary action, or client harm; all of which can have significant consequences for the professional and/or organisation involved.
As stated in the previous unit, there are a wide range of resources that you can consult to access specific acts or regulations, or information about specific pieces of legislation.
For example:
| Resource | Website |
|---|---|
| Commonwealth Legislation & Related Information | |
| The Federal Register of Legislation (the Legislation Register) is the authorised whole-of-government website for Commonwealth legislation and related documents. | https://www.legislation.gov.au/ |
| Commonwealth acts and regulations, the Constitution, and links to links to state and territory legislation. | https://info.australia.gov.au/information-and-services/public-safety-and-law/legislation |
| The Australasian Legal Information Institute (AustLII) publishes public legal information (legislation, treaties, decisions of courts and tribunals, etc.) | http://www.austlii.edu.au/ |
| The Australian Law Reform Commission is a federal agency that reviews Australia’s laws to promote improved access to justice for all Australians, encouraging laws and related processes to become more equitable, fair, and efficient | https://www.alrc.gov.au/ |
| State Legislation & Related Information | |
| Australian Capital Territory | https://legislation.act.gov.au/ |
| New South Wales | https://legislation.nsw.gov.au/ |
| Northern Territory | https://legislation.nt.gov.au/ |
| Queensland | https://www.legislation.qld.gov.au/ |
| South Australia | https://legislation.sa.gov.au/ |
| Tasmania | https://www.legislation.tas.gov.au/ |
| Victoria | https://www.legislation.vic.gov.au/ |
| Western Australia | https://www.legislation.wa.gov.au/ |
In addition to the above legislations, other relevant resources are:
The Australian Association of Practice Management (AAPM) has a Code of Ethical Conduct intended to provide standards of professional conduct that can be followed. Depending upon the circumstances, compliance or non-compliance with the Code of Ethical Conduct may be admissible in some legal proceedings.
Allied health organisations are also required to comply with all relevant legislation and facilitate this process for their workers. As such, organisations develop specific policies and procedures that comply with these requirements and which detail specific processes for workers to follow.

Health workers should be aware of their responsibilities to the community at large. As discussed earlier, this raises problems regarding confidentiality. Whenever a member of the community is at risk, property is likely to be damaged or other illegal actions are likely to occur or have occurred, then a health workers needs to decide what action is needed. Often such decisions do not involve choosing between black and white, but rather between shades of grey, and sometimes health workers may find it difficult to decide what is most appropriate to serve the needs of the person seeking help and the community in the long term.
In the previous unit, you were taken through a range of potential ethical dilemmas and ways in which these can be handled, through both individual problem-solving, and through seeking assistance from others. Though it is important to be self-sufficient and competent, which may at times involve resolving issues independently, there are times where this may not be possible. The below list provides a list of instances and scenarios that may prove challenging, especially if you’re new to the industry:
- Difficulty understanding legal and ethical responsibilities
- Difficulty understanding work role and responsibilities
- Reporting a breach or non-adherence to procedures or code
- Adverse event
- Unresolved conflict situations
- Ethical dilemma (e.g., conflict of interest)
At these times the sensible approach is for the health worker to talk through the ethical issues with their supervisor. In some instances, further action may need to be taken such as would be the case with mandatory reporting (i.e., discussing your concerns with a manager or internal supervisor before making a report and using a specific organisational form or process to make the report), or an incident report (reporting for both organisation and policy purposes).
In the cases of potential or actual boundary violations, this usually involves consulting with a supervisor to determine the most appropriate course of action to reinstate professional boundaries or to make other appropriate changes for the client, such as assigning a different health worker to their care. If conflict situations escalate or are unable to be resolved independently, it is best to consult a supervisor or allied health professional. Critical incident reports will need to be used to document any events or situations in which there is a risk of or actual serious harm, injury, or death to clients, workers, or others. Because of the serious nature of these situations, there will be specific policies and procedures in place for workers to follow at each organisation.
Lastly, a conflict of interest occurs when the personal interests of the worker conflict with their responsibility to act in the best interests of the client (AAPM, 2022). A conflict of interest can be actual, potential, or perceived and could result in risks to reputation, transparency, accountability, governance, and law. Health workers may encounter various instances of conflicts of interest, including:
- Personal relationships: Workers may have personal relationships with service users or colleagues that could compromise their professional judgment or impartiality.
- Financial interests: Workers may have financial interests in service users or organisations they work with, which could influence their decision-making.
- Professional relationships: Workers may have professional relationships with colleagues or organisations that could create conflicts of interest, such as dual relationships or conflicts between professional duties.
- Personal beliefs and values: Workers may have personal beliefs or values that could conflict with their professional duties or the best interests of service users.
When a conflict of interest does arise, health workers will need to discuss the issue with their supervisor as soon as possible to determine the most appropriate actions to take. If a health worker is ever unsure if something is a conflict of interest, they should seek guidance on the situation with a supervisor or allied health professional to allow an independent third party to decide. Where possible, the worker should manage the conflict of interest which may involve recusing themselves from certain tasks or decision, or avoiding situations that could create a conflict of interest.
Health workers can protect themselves by remaining up to date with relevant legislation, following standard practices, confirming their practices with more experienced colleagues, allied health professionals, and supervisors, and complying with the appropriate codes of conduct.
Here are some examples of responses to breaches:
- Intervene – Intervene immediately if you observe a breach taking place and it is safe to intervene. For example, a child is outside with another worker without a hat or sunscreen in summer. Approach the worker or the child and remind them about the sun safe policy.
- Report – Report observations or information about a breach to the relevant person. For example, a worker arrives at work to find the filing cabinet that contains confidential information about a person accessing services is unlocked. He writes an incident report and gives it to his team leader.
- Seek advice – Seek advice from senior staff members when unsure of how to respond to a breach. For example, a worker tells a colleague that she intends to visit a person accessing services in her own time on the weekend. The colleague is not sure what to do or if she should make a report, so she asks her supervisor for advice.
- Take action – Take action when aware that a staff member under your own supervision contributes to a breach. For example, a supervisor walks into the staffroom where workers are talking about a person’s confidential information inappropriately and unnecessarily. She reminds them of their confidentiality obligations and the disciplinary consequences if breaches continue.
Reporting Problems to the Supervisor
Part of organisational policies and procedures is to report to and notify the supervisor about problems, issues, and concerns. Issues and problems which are required to be reported include the following but are not limited to:
- Suspected cases of neglect and abuse on clients.
- Work health and safety hazards, risks, and incidents, including near misses.
- Grievances and complaints about workplace matters.
- Behaviours of concern.
- Problems regarding work routines and processes.
- Needs and requirements of clients that are not within the scope of the individual support worker’s role (e.g., providing psychological counselling, diagnosing medical conditions, and prescribing medication, etc.).
- Client’s changing needs (e.g., client’s increasing pain that requires a higher dosage of pain medication).

Documentation is necessary for meeting legislative requirements, communication between health-care providers, quality improvement and research, and legal proof that health care was provide. As a health worker, there will be times when you are required to complete documentation in accordance with legal requirements (such as mandatory reporting) and/or organisational standards and procedures. Types of documentation you may need to complete as a health worker includes:
- Documenting meetings/minutes
- Confidentiality forms
- Incident reports
- Forms associated with payments
- Referral forms
- Order forms for office supplies or medical supplies
- Other types of letters (such as a letter of attendance that a client attended the clinic or allied health organisation on a particular day)
These forms may be completed via paper and scanned digitally or completed electronically. Regardless of method, it is important that all written communication, including documentation, is completed using clear and accurate language. Objectivity is especially important – which means the information recorded should be only that which is directly seen, heard, felt, or smelled. Any subjective information, that is, information pertaining to speculation or judgement of the client and/or their situation, or any inclusion of personal bias should be avoided (Allied Health Professions’ Office of Queensland, 2019).
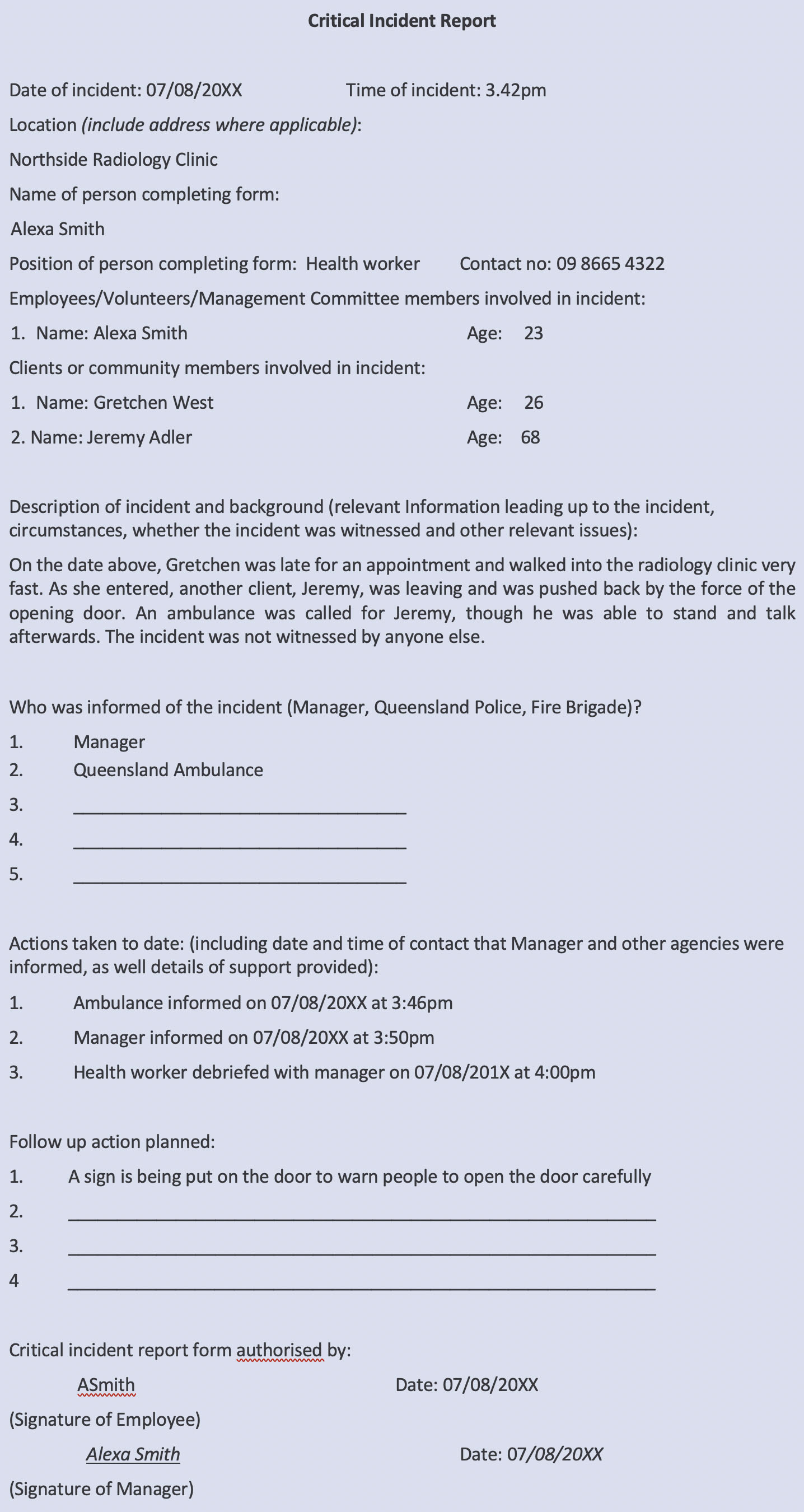
Incident report example
If a health worker is involved in a critical incident, they should follow their organisations policies and procedures which will involve documentation of the incident through filling out an Incident Report. Incident Reports are important as they document the event, any actions that have been taken, and are used to review and improve policies and procedures and safe workplace environments. As mentioned above, it is important to use clear, accurate and objective language when documenting events. An example of a scenario and corresponding Incident Report have been provided below.
Case Study
Incident Example
Alexa Smith works as a health worker at a radiology clinic called Northside Radiology Clinic. A new client, Gretchen, was running late for her first appointment and rushed through the door when they arrived. An older client, Jeremy, was leaving the clinic at the same time as Gretchen was arriving after having had a scan on his hip following hip replacement surgery. As Gretchen pushed open the door, Jeremy was hit by the door and fell back. He hit the back of his head and hurt his hip when he fell. He was able to stand afterwards, but Alexa called for an ambulance due to Jeremy’s age and medical history. Alexa was the only staff member in the waiting room at the time, and so had to fill out an Incident Report. An example of this report has been provided below.

As outlined above, there are various different uses of digital media in the healthcare industry. As such, each organisation will have policies and procedures surrounding digital media use that you will need to read and understand.
The Digital Health Policy Templates for allied health practices covers Policies and Procedures for Social Media, Website, electronic patient communication, and secure messaging. The Policy regarding social media states:
Regardless of whether social media is used for business related activity or for personal reasons, the following standards apply to members of our practice team. Practitioners and team members are legally responsible for their postings online. Practitioners and team members may be subject to liability and disciplinary action including termination of employment or contract if their posts are found to be in breach of this policy.
(Allied Health Professions Australia, 2020)
It also outlines that all staff have a responsibility to obtain approval before posting any public representation of the organisation for which they are working on social media. Posts should respect copyright, privacy, fair use, financial disclosure and any other relevant laws, and should contain a disclaimer regarding personal views not being representative of the particular practice/organisation for which they are a part of.
Access and ability to update or alter website information is generally restricted to those who’s role encompasses such activities, as is the case for SMS messages to patients/clients. Each staff member holds accountability for emails that are sent in their name or that are stored in their inbox including being aware of and cautious of spams, hoaxes, viruses; using appropriate language with electronic communications, and encrypting confidential client/patient information.
Read
Reading F: Digital Health Policy Templates for Allied Health Practices
The Allied Health Professions Australia has provided a set of digital health policies to guide for organisations to consider when implementing for their specific healthcare/discipline. It is a good tool for understanding the basic principles surrounding Digital Media use in allied health.
This section provided a refresher on the legal and ethical responsibilities of a health worker. Potential breaches, difficulties, non-adherences, adverse events, and ethical dilemmas were then discussed within the context of appropriate reporting and referring actions that should be taken.
- Allied Health Professionals Australia. (2023). Privacy. https://ahpa.com.au/privacy/#:~:text=AHPA%20will%20keep%20your%20personal,on%20our%20interaction%20with%20you.
- Allied Health Professions Australia. (2020). Digital health policy templates. https://ahpa.com.au/wp-content/uploads/2020/10/Digital-Health-policy-template-GEN.docx
- Australian Association of Practice Management Ltd (AAPM). (2022). Code of Ethical Conduct. 2nd Ed. https://www.aapm.org.au/Portals/1/AAPM%20Code%20of%20Ethical%20Conduct_FINAL_12OCT22.pdf
- Australian Human Rights Commission. (2016). Topic 8: Legal and ethical considerations of service delivery. https://humanrights.gov.au/sites/default/files/VET%20Disability%20Unit%20Trainer%20Manual%20-Topic%208.docx
- Australian Institute of Family Studies. (2020), Mandatory reporting of child abuse and neglect. https://aifs.gov.au/sites/default/files/publication-documents/2006_mandatory_reporting_of_child_abuse_and_neglect_0.pdf
- Child Safe Organisations. (2018). National Principles. https://childsafe.humanrights.gov.au/national-principles/download-national-principles
- College of Registered Nurses of Manitoba. (2022). Documentation Guidelines for Registered Nurses. https://crnm.mb.ca/wp-content/uploads/2022/01/Documentation-Guidelines-for.pdf
- Medical Administration Training (MAT). (n.d.). Roles and Responsibilities. https://mathealthclinic.com/wp-content/uploads/2019/05/roles-and-responsibilities-of-a-med-recept.pdf
- Migrant and Refugee Women’s Health Partnership. (2019). Guide for Clinicians Working with Interpreters in Healthcare Settings. https://culturaldiversityhealth.org.au/wp-content/uploads/2019/10/Guide-for-clinicians-working-with-interpreters-in-healthcare-settings-Jan2019.pdf
- NSW Government. (2019). Child at risk of harm and neglect. https://www.facs.nsw.gov.au/families/Protecting-kids/reporting-child-at-risk/harm-and-neglect/chapters/signs-of-abuse#:~:text=Risk%20factors&text=previous%20abuse%20or%20neglect%20of,young%20person%20in%20their%20care
- United Nations Sustainable Development Group. (2023). Human Rights-Based Approach. https://unsdg.un.org/2030-agenda/universal-values/human-rights-based-approach
- Workplace Health and Safety Queensland. (2021). How to manage work health and safety risks – Code of practice (pp. 5-25). https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0022/72634/how-to-manage-work-health-and-safety-risks-cop-2021.pdf
- The Compliance & Ethics Blog. (2018). [ Photo of post-it-notes with ‘wrong’, ‘right’ and question marks on the notes]. https://www.complianceandethics.org/ethics-not-as-simple-as-right-or-wrong-or-is-it/