In this section you will learn about:
- Legal frameworks and how they apply in practice management work.
- Sources of information about legal compliance.
- How to research information required for legal compliance.
Supplementary materials relevant to this section:
- Reading A: Universal Declaration of Human Rights
- Reading B: Mandatory Reporting of Child Abuse and Neglect
- Reading C: Easy Read Guide to the Anti-Discrimination Act
This module will introduce you to the legal and ethical frameworks and requirements which relate to practice management practice. You will learn about the specific laws that apply to practice management work and how to effectively perform your role while fulfilling your legal and ethical duties and responsibilities. This knowledge will enable you to become a more competent and confident practice manager and, as your career progresses, you will be able to use this knowledge to monitor legal and ethical compliance within your organisation.
Arriving at this point of your study, you are already aware of some legal and ethical requirements in practice management work. Unfortunately, the full range of information about these requirements involved in practice management is not found in one convenient place. Instead, specific pieces of information can be found in various places depending on whether the information is legal or ethical in nature, and general or workplace specific. While they are located in different places, they are also interrelated. For example, industry practice standards and ethical guidelines are, in part, developed to comply with relevant legislation; organisational policies and procedures are developed in accordance with legal and industry requirements.
The diagram below sets out some of the most important sources of information related to your legal and ethical practice – which we will explore in more detail shortly.
We encourage that you keep this in your mind as you read through this module. We will begin this exploration with an overview of the legal framework on which practice management (and allied health organisations) is founded in Section 1, followed by ethical framework in Section 2, and policies and procedures in Section 3.
It is vital that you possess a thorough understanding of these frameworks as they will provide you with a basis for understanding your role as a practice manager and will guide your decision-making processes in all of your work, including when monitoring and responding to compliance issues – which will be the focus of the final section.
Self Reflection
Before reading on, take a few moments to consider the importance of having a legal framework for practice management. What would practice management be like without a legal framework? Why do you think it is important for practice managers to understand the legal side of practice management?

Practice management, along with all of the other human services professions, is framed by international, Commonwealth state/territory, and local laws. These laws provide the foundation for what organisations and individuals who work for them can and cannot do. In order to understand how Australian legislation applies to practice management, you should first have a basic understanding of Australia’s legal framework.
Australian legislation complies with international legislation passed by the United Nations and abides by the principles outlined in the Universal Declaration of Human Rights.
Australia also has three levels of government for ‘law-making’, as shown in the diagram on your right. Laws made by each level of government follow a hierarchy.
In the event that there is a conflict between two levels of law, federal law can overrule state/territory laws and the state/territory law can overrule local laws, for the part of law that is inconsistent (Parliamentary Education Office, 2021a).
Australian legislation is split into Acts and Regulations. Act is a law made after a bill is passed by the Parliament. Regulation is a type of delegated law that often consist of specific details of how the provisions of an Act are applied. Changes to Act must be debated and passed by the Parliament, whereas regulation can be made or changed without these procedures.
Laws made by the Australian Parliament usually involve wide-ranging, complex issues that affect many Australians, such as taxation or the environment. These laws provide a general framework rather than specific detail of when, where and how the laws might be applied.
Delegated law allows the specific details of these existing – primary – laws to be made or changed without having to be debated and passed by the Parliament. Examples of delegated laws are regulations, standards and ordinances.
(Parliamentary Education Office, 2021b)
Some of these Acts and regulations provide the foundation for, and inform, the development of documents such as codes of practice, practice standards, and organisational policies and procedures which guide service provision in community services sector.
Practice managers can work in a variety of settings that provide a wide range of services. This means that there is a large range of legislation that can impact upon practice management, depending on your organisational context, role, and clientele. This module aims to review legal frameworks that impact upon practice management in general; however, you are encouraged to explore legislation that may be relevant to specific areas that you wish to work in (e.g., chiropractic, physiotherapy, podiatry, psychology, and other allied health professions). Whether you are a practice manager or managing an allied health organisation, you are not expected to become a legal expert. Nevertheless, it is essential for you to familiarise yourself with legislation relevant to your work context and develop the capability to source, access, and interpret information about legal frameworks to promote compliance (i.e., applicable requirements are met sufficiently and appropriately).
Now, let’s begin from an international framework that is an important influence on the formation of Australian laws as well as ethical frameworks of general helping professions.

The Universal Declaration of Human Rights is a declaration created by the United Nations General Assembly in the aftermath of World War II to protect and define human rights and fundamental freedoms. Many countries, including Australia, have ratified the document and incorporated the principles into their law. Because Australia has ratified this document, we have an obligation and duty under international law to respect, protect, and fulfil human rights. This is achieved through legislation and the day-to-day governance of our country. Each person is entitled to their human rights and must also respect the human rights of others.
Human rights recognise the inherent value of each person, regardless of background, where we live, what we look like, what we think or what we believe.
They are based on principles of dignity, equality and mutual respect, which are shared across cultures, religions and philosophies. They are about being treated fairly, treating others fairly and having the ability to make genuine choices in our daily lives.
Respect for human rights is the cornerstone of strong communities in which everyone can make a contribution and feel included.
(Australian Human Rights Commission, 2019)
The Universal Declaration of Human Rights highlights the importance of meeting a human’s basic needs for survival and protection in order for them to be able to develop in educational and cultural activities. The document also provides a benchmark for standards which the international community can refer to when they observe another country violating human rights.
Reading
Reading A: Universal Declaration of Human Rights
The full Universal Declaration of Human Rights is included in Reading A. Take a moment to browse through this document and consider how that influences the legal and ethical principles underpinning practice management and general helping services.
Before moving on, it is worth pausing a moment to think about what rights are. How is a right different from a human need?
Needs and Rights
Rights are things that we are entitled to – whether for survival, ethical, or legal reasons – and are related to human needs. We all know that there are basics that we need to survive, and still more if we are to live in a way that gives us a decent chance at physical and mental health, engagement with our families and communities, educational and work opportunities, and so on. Some of our basic needs include water, food, shelter, clothing, access to healthcare, and social contact – each of which can be classified as physiological needs to survive. Among the many things we need if we are to function well and be active in our communities and societies include access to education, news and other information, and ways of communicating.
Some rights are largely a recognition of a human need: we might say that we have a right to a safe home, a right to access to clean drinking water, a right to an education, and so on. In this way, rights extend beyond needs, to help people flourish. We also recognise that particular groups have additional rights based on their membership of that group. Children, for example, have the right to protection, with parents (or others where parents cannot or do not provide this) having the responsibility to provide protection, food, shelter, education, healthcare, etc., for their children. Similarly, people in groups that are marginalised within their societies have rights to freedom from discrimination. There are also rights that go beyond having particular needs met. For example, in democratic countries we have a right to vote, and in societies with legal systems that aim for fairness and justice, there is a recognition of the right to a fair trial.
But just because someone has a need does not mean that this need will be met. So, these rights are often formalised in legislation, such as federal and state or territory laws that outline – and provide mechanisms to promote or enforce – the rights of people in general, children, women, culturally and ethnically diverse groups, people of diverse sexualities, people with disabilities, and so on. There is no guarantee that a right will be respected either, but at least the international conventions and domestic laws that are endorsed and enacted provide accountability and encourage mechanisms to make it more likely that they will be. In some cases, they also provide for the punishment of people or organisations who abuse others’ rights or fail in their responsibilities to meet them.
You might be wondering why we are talking about rights here, but as you will see in the remainder of this unit, throughout your studies, and in the work that follows, much of what practice managers do is guided by human rights, including, children’s rights and the right to be free from discrimination. So, the United Nations Declaration of Human Rights is a great starting point.
Rights-Based Approach
An example of how human rights framework applies to allied health organisations is the adoption of a rights-based approach. The rights-based approach goes beyond addressing clients’ immediate needs (i.e., needs-based approach) to supporting the clients to claim the rights they are entitled to, applying the principles of empowerment and self-determination. Common principles have been identified as:
Participation: Everyone has the right to participate in decisions which affect their human rights. Participation must be active, free and meaningful, and give attention to issues of accessibility, including access to information in a form and a language which can be understood.
Accountability: Accountability requires effective monitoring of compliance with human rights standards and achievement of human rights goals, as well as effective remedies for human rights breaches. For accountability to be effective, there must be appropriate laws, policies, institutions, administrative procedures and mechanisms of redress in order to secure human rights.
Non-discrimination and equality: A human rights based approach means that all forms of discrimination in the realisation of rights must be prohibited, prevented and eliminated. It also means that priority should be given to people in the most marginalised or vulnerable situations who face the biggest barriers to realising their rights.
Empowerment: Everyone is entitled to claim and exercise their rights and freedoms. Individuals and communities need to be able to understand their rights, and to participate fully in the development of policy and practices which affect their lives.
Legality: A human rights-based approach requires that
- The law recognises human rights and freedoms as legally enforceable entitlements, and
- The law itself is consistent with human rights principles
(Australian Human Rights Commission, n.d.)
Self Reflection
Consider the above information about rights-based approaches and consider:
- If you were to engage in designing processes or procedures for your organisation, how can you make sure that human rights principles are integrated?
As such, allied health organisations are expected to proactively integrate human rights norms and principles into every aspect of organisational operations, such as through:
- Reviewing policies and procedures to check and maintain compatibility with human rights frameworks.
- Incorporating human rights consideration in planning and designing of service programs and delivery.
- Implement decision-making processes that incorporate consideration of human rights, and that staff and clients are informed of their rights.
- Incorporating human rights in staff induction, performance management and professional development processes.
- Making sure there are support and procedures in place to encourage staff and clients to raise any human rights concerns.
Anti-Discrimination Legislation

In Australia, it is considered a fundamental principle that all people, regardless of age, disability, race or sex are free to enjoy human rights. This principle is not only protected by the Universal Declaration of Human Rights but it is also reflected in specific Australian federal legislation, including:
- Age Discrimination Act 2004. This is a Commonwealth law that protects individuals from age-based discrimination in areas such as employment, education, access to premises, provision of good and services, renting or buying, requests for information, and the administration of Commonwealth laws and programs.
- Disability Discrimination Act 1992. This is a Commonwealth law that protects people living with a disability (such as physical, intellectual, psychiatric, sensory, neurological or learning disabilities, physical disfigurement, disorders, illness or diseases) from discrimination in areas such as employment, education, access to premises, accommodation, buying or selling land, the activities of clubs, administration of Commonwealth laws and programs, and the provision of goods, services and facilities.
- Racial Discrimination Act 1975. This is a Commonwealth law that protects people from discrimination on the basis of their race, colour, descent, and national or ethnic background in areas of employment, provision of goods and services, access to places and facilities, housing and other accommodation.
- Sex Discrimination Act 1984. This is a Commonwealth law that protects people from sexual harassment and discrimination due to their sex, sexuality, marital status, pregnancy, and family responsibility in areas of employment, partnerships, qualifying bodies, registered organisations, employment agencies, education, accommodation, clubs, superannuation, enterprise agreements, and the provision of goods, services and facilities.
- The Australian Human Rights Commission Act 1986 is the legislation that makes provision for people who believe they have been discriminated against.
- The Mental Health Act 2007 (Commonwealth) and State/Territory Mental Health Acts are designed to provide and facilitate the care and provision of mental health services whilst protecting the civil rights of those persons undergoing treatment through community care facilities.
Anti-discrimination legislation also operates at a State/Territory level, as outlined in the table below (Attorney-General’s Department, 2021).
| State/Territory | Anti-Discriminatory Law |
|---|---|
| Australian Central Territory | Discrimination Act 1991 |
| New South Wales | Anti-Discrimination Act 1977 |
| Northern Territory | Anti-Discrimination Act 1996 |
| Queensland | Anti-Discrimination Act 1991 |
| South Australia | Equal Opportunity Act 1984 |
| Tasmania | Anti-Discrimination Act 1998 |
| Victoria | Equal Opportunity Act 2010 |
| Western Australia | Equal Opportunity Act 1984 |
Informed Consent
Another key practice set out to protect client rights is informed consent. Practice managers have a responsibility to make sure that client has given their informed consent to the service they will be offered. Informed consent involves two core components. The first involves providing the client with the information he or she needs to make a reasoned decision about whether to engage in the services being offered (e.g., what service provision will involve as well as its risks and potential benefits). The second is free consent – practice managers need to ensure that that this agreement is given freely and without coercion (Welfel, 2016). Inherently, by engaging clients in informed consent processes, practice managers confirm and respect the client’s right to manage their own lives and choose their own care (Welfel, 2016).
In most cases, informed consent means that clients have the opportunity to decline service once they have had an opportunity to find out about the risks and benefits.
Organisations generally develop strict policies around contracting as well as formal written contracts to assist in the process of obtaining informed consent. Of course, practice managers do not just provide clients with a written contract – they also have a detailed conversation with each client, including confirming the client’s understanding. This means making sure that, before service is offered, the practice manager informs the client about the purpose of services being offered, how services will be provided, any risks involved, the limits of each service, and their rights and responsibilities. It also involves ensuring that the client understands confidentiality, its limitations, and consents to the release of their personal information.
Below is a sample client rights and responsibilities statement that could be provided to clients during informed consent processes.
| CLIENT RIGHTS |
|---|
|
| CLIENT RESPONSIBILITIES |
|
Among other key legal and ethical requirements, this statement highlights the importance of informed consent governing how a practice manager may work with a client and their personal information, which we will discuss next.
Privacy Legislation

The Privacy Act 1988 is designed to protect people’s personal information. It provides a legal framework which regulates how personal information is to be collected, stored and disclosed, as well as who is allowed to access and make amendments to stored information.
This Commonwealth legislation forms the basis of many practice management, policies, practices, and procedures. It specifies that information should only be used for the purposes for which it was gathered as well as the right for clients to be able to access information held about themselves, to change information held about them, or to make a complaint if they believe that their privacy has been compromised. The case study below demonstrates the Privacy Act 1988 in action.
Case Study
Bronwyn is a practice manager of a small allied health organisation. She is a new worker and wanted to review all the files of the clients in the organisation’s records. Bronwyn would like to know the history of the people she may be working with. However, the allied health assistant pointed out to Bronwyn that according to the Privacy Act 1988 Bronwyn should not be given access to this information. Bronwyn was disappointed but understood that clients are entitled to feel confident that their personal information is collected only for the purposes of being provided the service, that their information is stored in a secure place, and that only essential people have access to their personal details. Bronwyn will be given details about clients only when directly related to her role.
All allied health organisations and practice managers are required to abide by Privacy legislation. The organisation you work for will have their own specific policies and procedures (such as confidentiality policies, privacy policies, and file storage policies) in place to ensure that their workers comply with this legislation. Organisational policies and procedures concerning these issues must be compliant with the Privacy Act 1988. We will now review some of the key organisational practices influenced by the Privacy Act.
Confidentiality and Disclosure
Policies and practices about confidentiality are influenced by the Privacy Act 1988. Most individuals seeking assistance from allied health organisations will want assurance that their personal information will remain private and confidential.
Confidentiality is both an ethical principle and a legal right. It is the most basic right of any person, either in treatment or receiving services, to know that what the person is sharing in your office will remain confidential. It is important to protect individuals to whom we give service by not disclosing their personal situations without the people having authorized such a disclosure.
(Summers, 2016)
Issues of confidentiality must be discussed with clients at the beginning of service provision. Practice managers also have a responsibility to ensure that clients are aware of the limits of confidentiality and the circumstances in which it may be overridden, including:
- When the client needs to be protected from harming themselves (e.g., suicide).
- Where others need to be protected (e.g., if a client has threatened to harm others; risk of harm to a child or elderly person).
- If the health and/or welfare of a client is at risk (e.g., family violence).
- If a worker (or the client’s file) is subpoenaed by a court of law.
- If the client gives consent for the practice manager to share their information with another service provider.
If a situation arises in which you are required to break client confidentiality, it is good practice to discuss this with the client and explain the specific steps you will be taking to keep them or others safe.
Many health and community services organisations provide clients with a written explanation of the limits of confidentiality as part of the informed consent processes. While it is good practice to provide clients with such a document and allow them to keep it for future reference, it is also important to take the time to carefully explain confidentiality and its limits. Practice managers should also ensure that the client has an opportunity to ask questions and clarify their understanding if necessary. Below is an example of a confidentiality statement.
CONFIDENTIALITY STATEMENT
It is the responsibility of the practice manager and the organisation to ensure confidentiality of your information. However, some situations result in limitations of confidentiality. These situations are:
- If there is a danger of you harming yourself or another person.
- If you report the abuse or neglect of a client.
- If required by the courts to release information.
- If you give consent to sharing your information for the purpose of service provision.
It is a legal and ethical responsibility for us to contact relevant professionals under these circumstances.
I………………………….……understand and accept the limitations of confidentiality.
Signed……………………………
Date……………………………
Practice manager signature……………………………
Date……………………………
Practice managers also need to ensure that they provide information that is appropriate for their clients, taking into account their age, literacy, and developmental status. For example, if the client is a young child or has an intellectual disability, they may require more simplified language or a simplistic confidentiality statement, as depicted in the example below. Information may also be provided in plain English and/or cultural languages. In all circumstances, it is important to check and confirm client’s understanding.
CONFIDENTIALITY STATEMENT
What You Say in here
Stays in here
Exceptions:
Someone is hurting you
You want to hurt someone
You want to hurt yourself
Maintaining confidentiality also means that practice managers do not share information about their clients with anyone except as a direct part of their role or of the supervisory process (e.g., sharing information with your supervisor according to your organisation’s policies and procedures). Any discussion of client information should only ever take place in the workplace and should not be audible to other unrelated members of staff or the general public. It is also important to note that practice managers should never discuss their clients’ information with their own family or friends. While it is often tempting to discuss work with your family and friends, doing so can actually be a breach of your client’s confidentiality. This is highlighted in the extract below.
It is tempting to talk about your clients and their stories, especially as others are usually curious about what you do. It may give you a sense of importance to be able to tell interesting anecdotes. You may talk more freely than you should when you feel overwhelmed by your clients and need to unburden yourself. As a professional helper, you must learn how to talk about clients and how to report without breaking confidentiality. Clients should know that confidentiality cannot be guaranteed absolutely, but they should have your assurance that you will avoid talking about them except when the law requires you to disclose information or it is professionally necessary to do so.”
(Corey & Corey, 2021, p. 242)
The following scenario demonstrates the importance of maintaining client confidentiality.
Case Study
Alice is sitting at a café enjoying a coffee with one of her friends. Soon enough her attention is caught by a familiar voice conversing with another person at the table behind her. Alice realises that the person behind her is her practice manager, Jacinta. Alice can hear that Jacinta is venting to her friend about the stressful week she had at work. At one point Alice realises that Jacinta is talking about her own conversation with Jacinta. While Jacinta does not use Alice’s name, it is clear based on the details of the story that she is the client Jacinta is talking about.
Self Reflection
Reflect on Case Study
Reflect upon the case study above. How do you think you would feel if you were Alice?
What legislation and workplace policies did Jacinta violate?
Imagine that you are Jacinta’s team manager and Alice made a complaint against Jacinta. What might you do?
Maintaining client confidentiality is sometimes tricky in cases in which a practice manager runs into a client outside of the work environment. Particularly if you are working in regional areas, it is not uncommon to see your clients in social situations. To protect a client’s confidentiality, we must never indicate to anyone else that that they are our client, unless the client wishes for it to be disclosed. Consider the following case study.
Case Study
Rachel is a practice manager at an allied health organisation. One afternoon Rachel was out walking with her friend at a park when one of her clients, Patricia, who has also been out for a stroll greets Rachel. Rachel chats briefly with Patricia, then excuses herself and continues her walk with her friend. Rachel’s friend then asks who Patricia is and how Rachel knows her. Rachel responds, “Oh she is just a girl I have met once or twice”. Rachel was careful not to identify Patricia as a client.
As you can see, practice managers are required by law to ensure that their clients’ information is kept private and confidential. Apart from the exceptional circumstances, there may be other occasions when you may obtain client’s permission to share their information, for example:
- When working in collaboration with other practitioners or services (e.g., when a client has multiple co-occurring needs that can only be addressed by accessing services concurrently, certain information may be shared to ensure client needs are met).
- To gain client’s permission to use their information/identification for additional purposes (for example, using their picture in marketing publications).
In these events, you must make sure the client has been informed of and provided their written consent for information to be shared or used to that particular purpose. Such conversation also provides an opportunity for clients to ask questions, if any, or choose not to provide their consent.
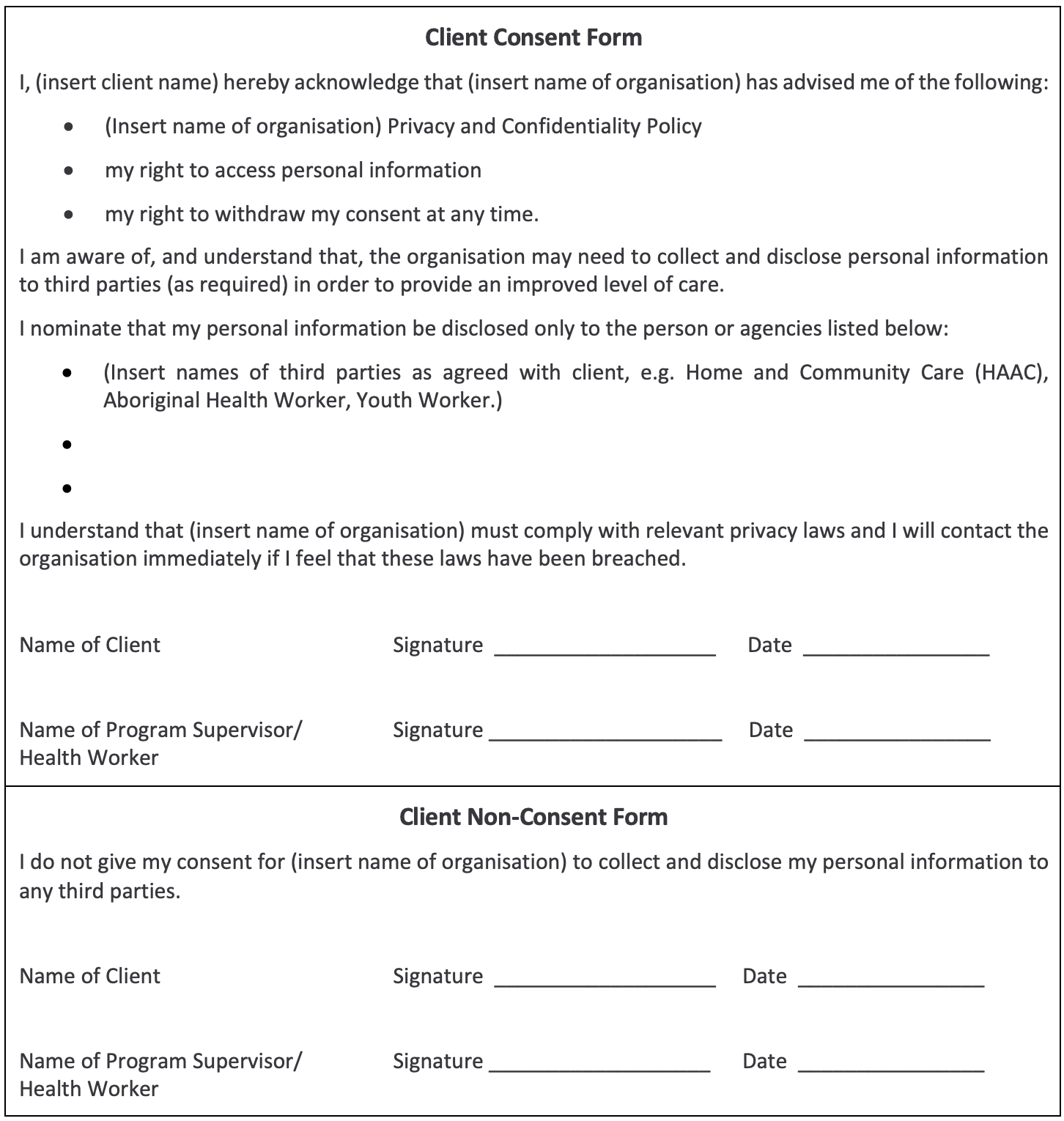
On the following page, you will see a template of client consent form and non-consent form developed by Community Door (n.d.) that community services organisations may adapt for their own use.
One situation in which confidentiality may be overridden is when information about suspected or actual child abuse has been disclosed. Most practice managers will have a mandatory reporting duty under the child protection and family law legislation.
Child Protection Legislation

Within Australia, child protection legislation differs by State and Territory. However, all these laws are founded upon the principle of the “best interests of the child”. Together, they establish the legislative framework governing child wellbeing and the provision of child protection and out-of-home care services in Australia. All agencies must work together to achieve the safety, welfare, and wellbeing of children or young people in all decisions made.
The table on the following page outlines the key child protection legislation for each state and territory. These state/territory child protection laws, along with the Commonwealth legislation – Family Law Act 1975 (Cth) – set out the mandatory reporting duty for people in particular professions or roles.
| State/Territory | Child Protection Legislation |
|---|---|
| Australian Central Territory | Children and Young People Act 2008 |
| New South Wales | Children and Young Persons (Care and Protection) Act 1998 |
| Northern Territory | Care and Protection of Children Act 2007 |
| Queensland | Child Protection Act 1999 |
| South Australia | Children and Young People (Safety) Act 2017 |
| Tasmania | Children, Young Persons and their Families Act 1997 |
| Victoria | Children, Youth and Families Act 2005 |
| Western Australia | Children and Community Services Act 2004 |
Mandatory Reporting
Mandatory reporting is a term used to describe the legislative requirement of certain classes of people to report suspected cases of child abuse and neglect to government authorities (Australian Institute of Family Studies, 2020). While all States and Territories have some form of mandatory reporting legislation, the specific details do vary. Different jurisdictions (e.g., States and Territories) differ in the types of abuse that must be reported.
Reading
Reading B: Mandatory Reporting of Child Abuse and Neglect
Reading B outlines the reporting requirements within each jurisdiction in Australia and highlights the major differences between the different State and Territory laws. For example, with the exception of sexual abuse, which must always be reported, some states only require significant abuse to be reported whereas more minor abuse can be referred to child and family welfare agencies.
In your own work practice, if you suspect risk of harm or abuse to a child or young person, you should report your concerns to your supervisor and discuss the next step. Depending on your organisation’s policy, either you or another specialist member of staff will be responsible for reporting your concern. Most organisations have a mandatory reporting responsibility. Organisational managers, including unpaid members of management committees, are typically mandatory reporters and are also supervisors of mandatory reporters. This means that, as a supervisor, they need to provide support and make sure their staff are reporting situations in which a client is at risk of harm. This includes training their staff in the organisation’s policies and procedures (e.g., documenting relevant information and actions carried out) as well as their legal responsibilities in relation to mandatory reporting. Additionally, organisations who are government funded will typically have an agreement with the government that requires everyone in their organisation to make a report if they suspect a client is at risk.
Case Study
Hudson is a practice manager and has commenced working with a new client, Dylan. Dylan is twelve years old and Hudson notices that Dylan has several burn marks on his legs in various stages of healing. When Hudson asks Dylan about his injuries, Dylan is not able to provide a clear explanation of how they occurred, and Hudson is unable to engage him further on the topic.
Hudson is aware that he must report his suspicions and refers to his organisation’s policies and procedures about reporting. The policies advise that Hudson should contact his supervisor and make a report of his concerns.
Self Reflection
Reflect on Case Study
What legislation would Hudson have breached if he failed to report his suspicions? What are the possible consequences to Hudson, as well as Dylan?
How would you feel about doing a report if you were in Hudson’s position? If necessary, how might you go about developing your competence in this area?
A Note on Working with Children Check
Another legal requirement relevant to child safety and children’s rights is the requirement for people who work with children and youth to undergo necessary checks and working with children clearances. There is no national framework for working with children checks – each State or Territory has its own legislation and screening requirements related to this. Community services organisations that offer services to children and young people need to ensure that workers have acquired the relevant check related to the jurisdiction in which they work, as these checks are not transferrable across jurisdictions. The following table outlines the screening check names and relevant legislation by State or Territory in which screening requirements can be found (Australian Institute of Family Studies, 2021).
| Jurisdiction | Legislation | Name of the Check |
|---|---|---|
| ACT | Working With Vulnerable People (Background Checking) Act 2011 (ACT) | Working with Vulnerable People (WWVP) registration |
| NSW | Child Protection (Working with Children) Act 2012 (NSW), Child Protection (Working with Children) Regulation 2013 (NSW), Child Protection (Working with Children) Amendment (Statutory Review) Act 2018 (NSW) | Working with Children Check (WWCC) |
| NT | Care and Protection of Children Act 2007 (NT) | Working with Children Clearance/ Ochre Card |
| QLD | Working with Children (Risk Management and Screening) Act 2000 (Qld) | Blue Card/ Working with Children Check |
| SA | Child Safety (Prohibited Persons) Act 2016 (SA), Children’s Protection Law Reform (Transitional Arrangements and Related Amendments) Act 2017 (SA) and Child Safety (Prohibited Persons) Regulations 2019 (SA) | Working with Children Check |
| TAS | Registration to Work with Vulnerable People Act 2013 (Tas.) | Working with Vulnerable People check |
| VIC | Worker Screening Act 2020 (Vic.) | Working with Children Check |
| WA | Working With Children (Criminal Record Checking) Act 2004 (WA) | Working with Children Check |
Workplace Health and Safety Legislation
Another key type of legislation that impacts practice management is workplace health and safety legislation. While you will learn much more about this legislation and WHS practices in HLTWHS004 Manage Work Health and Safety, in a nutshell, this legislation requires both organisational management and workers to contribute to the development and maintenance of a safe and healthy workplace. Each worker should become familiar with their own legal obligations in relation to ensuring workplace health and safety under WHS-related federal and state legislation. Additionally, each organisation will have specific WHS-related policies and procedures for workers to follow and each worker must comply with these requirements.
Learn More about WHS
For more information about WHS you can go to the Safe Work Australia website. Alternatively, you can also access the website of the WHS regulator in your jurisdiction:
- SafeWork NSW
- WorkSafe ACT
- WorkSafe WA
- Workplace Health and Safety Queensland
- SafeWork SA
- WorkSafe Tasmania
- WorkSafe Victoria
- NT WorkSafe
- Comcare (Commonwealth WHS)
Most of these websites offer newsletters that you can subscribe so that you can stay on top of any recent updates or changes in the WHS area.
Industrial Relations Legislation

Another key type of legislation that impacts all employment relationships, including community services organisations and practice managers, is industrial relations legislation. The employee/employer relationship in Australia is currently governed (from a national context) by the Fair Work Act 2009 and the Fair Work Regulations 2009. This legislation outlines the minimum obligations and entitlements of employers and employees. It also helps to ensure access to flexible working arrangements and fairness at work and helps to prevent discrimination against employees (Fair Work Ombudsman, n.d.).
The following extract provides a brief outline of the National Workplace Relations System (i.e., The Fair Work system) that is currently in place within Australia.
The Fair Work system
The Fair Work system was created by the Fair Work Act 2009 and started on 1 July 2009. The Fair Work system is the name used for the minimum employment laws and agency bodies that were created by the Fair Work Act. It is the national workplace relations system. [...]
Key features of the Fair Work system
The key features of the Fair Work system are:
- 11 minimum National Employment Standards
- awards that apply nationally for specific industries and occupations
- the national minimum wage
- protection from unfair dismissal.
Awards, together with the National Employment Standards and the national minimum wage, make up a safety net of entitlements for employees covered by the Fair Work system.
There are 5 bodies that have roles in the Fair Work system:
- Fair Work Ombudsman (us)
- Fair Work Commission
- Australian Building and Construction Commission
- Registered Organisations Commission
- Fair Work Federal Division of the Federal Court and the Federal Circuit Court
Who is covered by the Fair Work system
The Fair Work system covers most Australian workplaces. Working out who is covered is important because we work with employers and employees covered by the Fair Work system (the national system).
Employers and employees who aren’t covered by the Fair Work system should contact the relevant state body or their internal human resources department for help.
(Fair Work Ombudsman, n.d.)
As you can see, an important aspect of the Fair Work System is the National Employment Standards, which outline the 11 minimum entitlements that must be provided to all employees. It is important for you to be aware of these entitlements in order to understand your rights as an employee. These entitlements include (Fair Work Ombudsman, n.d.):
- Maximum weekly hours
- Requests for flexible working arrangements
- Offers and requests to convert from casual to permanent employment
- Parental leave and related entitlements
- Annual leave
- Personal/carer's leave, compassionate leave and unpaid family and domestic violence leave
- Community service leave
- Long service leave
- Public holidays
- Notice of termination and redundancy pay
- Fair Work Information Statement and Casual Employment Information Statement
The Fair Work Ombudsman is responsible for working with employers/employees to educate and encourage compliance with Australian workplace laws. If at any time in your career you feel that something is not right or you have a grievance with an employer, the role of the Fair Work Ombudsman is to provide information and mediation to assist in resolving the matter. Matters that the Ombudsman can assist with include:
- Pay – e.g. penalty rates, allowances and loadings
- Leave – e.g. annual, sick, maternity and parental leave
- Ending employment – e.g. notice, final pay and redundancy
- Discrimination and other workplace protections
- Sham contracting
- Union membership and right of entry
Anything else covered by an award, enterprise agreement or other registered agreement from January 2010, each State/Territory migrated the majority of their industrial relations responsibilities to the National Workplace Relations System (i.e., The Fair Work System). However, some public sector employers/employees were excluded. It is a good idea to check what system you work under. If you are not covered by the national system, you should contact your relevant state body (Fair Work Ombudsman, n.d.):
- New South Wales - NSW Industrial Relations
- South Australia - SafeWork SA
- Queensland - Queensland Government
- Tasmania - Tasmanian State Service Industrial Relations
- Victoria - Business Victoria
- Western Australia - WA Labour Relations
- Note: All employers and employees in the ACT and Northern Territory are covered by the national system.
Stay in the Know
As an employee it is essential you know your rights in relation to workplace issues and staying up-to-date with these issues helps you know whether your rights are being met and protected. You can subscribe to Fair Work’s email updates to stay in the know.
Self Reflection
Pause for a moment to reflect on the range of legal requirements we have covered in this section of the Study Guide. Is there any that you would like to find out more about? How might you go about finding relevant information?
Finding the right information for legal compliance may not be an easy task. Particularly, practice managers can work in a wide variety of different allied health organisations. As you can imagine, some legislative requirements relate more to certain organisations than the others due to the organisational context, nature of work, and clientele involved. For example, practice managers working in mental health or psychology sector will need to be familiar with certain mental health legislation. Additionally, allied health services are provided through both the private and public sector and are subject to both Commonwealth and state/territory legislation. Due to the broad and varied nature of practice management work, it is difficult to provide a concise and definitive list of legislation you will need to comply with as a practice manager – it depends upon the specific role, industry, and jurisdiction you are working in.
Often, the selection criteria or job description of your role will direct you towards the relevant legislation you need to be aware of in performing your duties. You are also likely to find reference to legislation in your organisational policies and procedures (which are developed to support and monitor compliance in the first place). However, if you are ever unsure about your legal obligations, you must seek out a supervisor or manager for advice on which legislation is relevant to your role.
Ultimately, practice managers and their organisations are required to comply with legislation set out in Commonwealth and State Acts and that failure to comply with such legislation may result in a punishment determined and enforced by the courts. As a practice manager, you may need to research about particular pieces of legislation relevant to a new role or a client’s circumstances. You may also be engaged in reviewing and/or developing policies and procedures for the organisation you are working in. Moreover, legislation can be reviewed and updated, hence it is important that you know where to source information about these legal requirements.
There are a wide range of resources you can consult to access specific acts or regulations, or information about specific pieces of legislation. The table on the following page lists some of the websites you may use to retrieve legislation and related information.
| Resource | Website |
|---|---|
| Commonwealth Legislation & Related Information | |
| Commonwealth | https://www.legislation.gov.au/ |
| Commonwealth acts and regulations, the Constitution, and links to links to state and territory legislation. | https://info.australia.gov.au/infor-mation-and-services/public-safety-and-law/legislation |
| The Australian Law Reform Commission is a federal agency that reviews Australia’s laws to promote improved access to justice for all Australians, encouraging laws and related processes to be-come more equitable, fair, and efficient | https://www.alrc.gov.au/ |
| State Legislation & Related Information | |
| Queensland | https://www.legislation.qld.gov.au/ |
| New South Wales | http://www.legislation.nsw.gov.au/ |
| Australian Capital Territory | http://www.legislation.act.gov.au/ |
| Victoria | http://www.legislation.vic.gov.au/ |
| Tasmania | https://www.legislation.tas.gov.au/ |
| South Australia | https://www.legislation.sa.gov.au/ |
| Northern Territory | https://legislation.nt.gov.au/ |
| Western Australia | https://www.legislation.wa.gov.au/ |
For most helping professionals, interpreting legislation can be challenging. Even for those in managerial positions, they are not usually expected to have legal expertise. However, you will find that there are a range of plain English documentation developed to explain legislation in a ‘user-friendly’ way. These documents are usually written for general public or specific groups of audience, using day-to-day or simpler language, while remaining legally accurate and do not distort or change the impact of the respective legislation.
Reading
Reading C: Easy Read Guide to the Anti-Discrimination Act
Reading C demonstrates an easy read guide to the Anti-Discrimination Act 1991 (Qld). Documents as such are not only useful for practitioners, but also for clients to understand what their legal rights are, particularly for clients who may not have high literacy or prefer other languages than English.
Of course, not all your responsibilities are set out in legislation. Sometimes, a practitioner’s actions (or failure to act) can come under the ruling of common law. Common law refers to the decisions that are made in court by judges guided by legal precedents (or previous rulings). For example, there is no direct legislation outlining what constitutes duty of care in a practice manager’s role. Therefore, if a practice manager is accused of failing in their duty of care it is not simply a case of consulting a specific Act. The case will need to be decided in a court according to legal precedents and what the profession and community believes constitutes an appropriate level of care. The court may also refer to instruments such industry codes of ethics and conduct and organisational policies and procedures in order to determine whether a worker has failed in their duty of care. However, if there is a conflict between legislation (i.e., statutory law) and common law, legislation will override the common law.
Allied health organisations will need to take these into account to promote, monitor, and maintain legal compliance in the organisation. As you will notice in Section 3, different policies and procedures are created and reviewed regularly to make sure the staff and the organisation operate in a way that complies with these legal frameworks.
This section of the module has introduced you to the legal framework surrounding practice management. You have learned about some of the key legislation that practice managers and allied health organisations need to comply with, including legislation relating to human rights, discrimination, client privacy and confidentiality, informed consent, mandatory reporting, workplace health and safety, and industrial relations. These legislative frameworks inform and are interrelated to the ethical frameworks we will be exploring in the next section.
- Attorney-General’s Department. (2021). Human rights and anti-discrimination. Commonwealth of Australia. https://www.ag.gov.au/rights-and-protections/human-rights-and-anti-discrimination
- Australian Human Rights Commission. (2019). What are human rights? https://www.humanrights.gov.au/about/what-are-human-rights
- Australian Institute of Family Studies. (2020). Mandatory reporting of child abuse and neglect. CFCA Resource Sheet – June 2020. https://aifs.gov.au/cfca/publications/mandatory-reporting-child-abuse-and-neglect.
- Australian Institute of Family Studies. (2021). Pre-employment screening: Working with children checks and police checks. CFCA Resource Sheet – June 2021. https://aifs.gov.au/cfca/publications/pre-employment-screening-working-children-checks-and-police-checks
- Community Care Options. (2017). Policy Manual: Section 3 - Access and Service Delivery. http://cco.net.au/wp-content/uploads/2013/08/Policy-Manual-Section-3-Access-and-Service-Delivery-2017.pdf
- Community Door. (n.d.) Policies, procedures & templates. https://communitydoor.org.au/resources/administration/policies-procedures-templates
- Corey, M. S. & Corey, G. (2021). Becoming a helper (8th ed). Cengage Learning.
- Corey, G., Corey, M. S., & Corey, C. (2019). Issues & ethics in the helping professions (10th ed.). Cengage Learning.
- Fair Work Ombudsman. (n.d.). The Fair Work System. https://www.fairwork.gov.au/about-us/legislation/the-fair-work-system
- Hepworth, D., Rooney, R., Dewberry Rooney, G., & Strom-Gottfried, K. (2017). Direct social work practice: Theory and skills (10th ed.). Cengage Learning.
- McPherson, J. (2020). Now is the time for a rights-based approach to social work practice. Journal of Human Rights and Social Work, 1–3. Advance online publication. https://doi.org/10.1007/s41134-020-00125-1
- National Disability Services. (2015). Restricted Practice Authorisation Panel Workshop: Safeguarding the Rights of Individuals Learning Guide. http://www.idfnsw.org.au/images/RPA_LearningGuide.pdf
- Office of the Australian Information Commissioner. (2018). Guide to securing personal information. Australian Government. https://www.oaic.gov.au/agencies-and-organisations/guides/guide-to-securing-personal-information
- Parliamentary Education Office (PEO). (2021a). Three levels of government: governing Australia. Commonwealth of Australia. https://peo.gov.au/understand-our-parliament/how-parliament-works/three-levels-of-government/three-levels-of-government-governing-australia/
- Parliamentary Education Office (PEO). (2021b). Delegated law. Commonwealth of Australia. https://peo.gov.au/understand-our-parliament/how-parliament-works/bills-and-laws/delegated-law/
- Substance Abuse and Mental Health Services Administration. (2019). Trauma and violence. https://www.samhsa.gov/trauma-violence
- The Compliance and Ethics Blog. (2019). [Image of cartoon outlines and corresponding relevant text relating to work safety]. https://www.complianceandethics.org/the-occupational-health-and-safety-rights-of-workers/
- Training.com.au. (2020). [Image of a young man with a collared, buttoned up shirt assisting an elderly lady; both are smiling]. https://www.training.com.au/ed/6-pathways-into-community-services-career/
- World Health Organization. (2023). [Photograph of a gavel and stethoscope]. https://www.who.int/activities/strengthening-legal-frameworks-for-uhc
- Victorian Equal Opportunity and Human Rights Commission. (2014). Rights and Risk: How human rights can influence support risk management for public authorities in Victoria. https://vgls.sdp.sirsidynix.net.au/client/search/asset/1271728
